Abstract
Introduction and Aim
Recently, the incidence of obesity has been rising exponentially. Clinical studies have demonstrated that different subtypes of pulmonary hypertension (PH) are linked to obesity. The current work mainly aims to assess the impact of laparoscopic sleeve gastrectomy (LSG) on PH in a cohort of obese cases.
Patients and Methods
The present prospective work included 37 obese cases with PH for whom LSG was done. Only cases with PH and presurgical right ventricular systolic pressure (RVSP) ≥ 35 mmHg using Doppler echocardiogram were enrolled. Fifteen months later, patients were reassessed regarding new weight and BMI in addition to changes in RVSP.
Results
At the end of follow-up, the average BMI improved from 45.8 + 3.9 to 33.8 + 2.5 Kg/m2 (p value < 0.001). Improved right ventricular (RV) size compared to baseline echo was observed in 20 patients. RV size decreased from 2.68 + 0.44 cm to 2.34 + 0.36 cm (p value < 0.001). Notable decrease of PH to less than 30 mmHg occurred in 33 patients. Mean RVSP decreased from 39.62 + 2.1 to 31.81 + 3.1 mmHg (p value < 0.001). LSG significantly decreased the requirements for PH drugs and supplemental oxygen therapy.
Conclusion
The current work suggests that LSG-induced weight loss may result in a considerable decrease in pulmonary pressures as well as RV size with a concurrent resolution of other metabolic comorbidities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recently, the incidence of obesity has been rising exponentially. There are scarce data about the rate of occurrence of pulmonary hypertension (PH) in obese people, and most of the data come from retrospective single-center researches [1].
Clinical studies have demonstrated that different subtypes of PH are linked to obesity. A previous single-center study showed that the incidence of PH was 38% among the obese cases [2].
The pathogenesis of obesity-linked PH is complex and multifactorial. Adipose tissue is an endocrine organ that has a pivotal role in vascular and metabolic homeostasis. Besides, it secretes many types of bioactive molecules, adipocytokines, that are implicated in the local and systemic inflammatory response [3].
This inflammatory response, in addition to insulin resistance and oxidative stress, has a substantial contribution to the pathogenesis of obesity and PH [4].
PH is classically depicted by mean pulmonary artery pressure (PAP) more than 25 mmHg during a right heart catheterization. Nevertheless, an echocardiogram is a more accessible non-invasive conventional screening tool for PH as it can give estimates of peak pulmonary artery systolic pressure (PASP) [5].
PH spectrum, according to the World Health Organization definition, includes primary pulmonary arterial hypertension (PAH), PH secondary to left-sided cardiac failure, PH due to lung disorders, PH due to thromboembolic phenomena, and PH due to miscellaneous causes [6].
The current management of PH concentrates on the treatment of the underlying causes, in addition to diuretics and oxygen therapy. More advanced medications can affect PAP directly. They include prostacyclin analogues, endothelin receptor antagonists, and phosphodiesterase 5 inhibitors [6].
The rate of adverse events in cases with PH is albeit high, despite the recent milestones in treatment [7].
Metabolic surgery has been recognized as an effective treatment strategy for obesity, with a rapidly rising number of operations. Laparoscopic sleeve gastrectomy (LSG) is now considered the most wide-spread type of bariatric surgery [8].
Moreover, LSG seems to be a safe and efficacious option in terms of loss of excess body weight and amelioration of obesity-associated comorbidities [9].
The impact of bariatric surgery, including LSG, on cases with PH, is still very limited and understudied. Given the effectiveness of bariatric operations in the resolution of the predisposing factors that may be implicated in PH, weight-loss procedures, including LSG, may result in the resolution of PH [10].
The current work originally endeavors to assess the impact of LSG on pulmonary hypertension in a group of obese subjects.
The secondary objective was to assess perioperative complications of LSG in this high-risk group of patients in addition to improvement of obesity-related morbidities post-LSG.
Subjects and Methods
Study Cohort
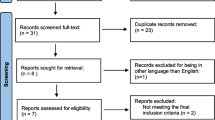
All patients who presented during the study period (from July 2013 to February 2018) underwent a cardiologic evaluation (n 256), and only those with an increase in PAP were considered for the study (n 55). After exclusion of those who were lost to follow-up, this prospective work enrolled 37 obese patients with PH who underwent LSG.
The work protocol obtained the agreement of the institutional review board. We adopted the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) instructions during the preparation of the current prospective work. All cases gave a written informed consent prior to enrollment.
Patients who were eligible to participate in the study included motivated obese patients with PH and BMI more than 40 Kg/m2 or more than 35 Kg/m2 with relevant comorbidities, patients who are willing to participate in the management and regular follow-up, cases in whom conservative strategies did not succeed to achieve adequate weight control, ages from 18 to 60 years, and finally those with no endocrine causes for their obesity.
Diagnosis of PH was assured by pulmonologist according to the Task Force for the definition and Diagnosis of Pulmonary Hypertension by the American College of Cardiology Foundation [11].
Right ventricular systolic pressure (RVSP) was assessed employing the transthoracic Doppler echocardiography. RVSP was employed as an alternative method for PAP because it is non-invasive [6]. Echocardiography was done to candidate participants, and only cases with PH and RVSP ≥ 35 before surgery mmHg using Doppler echocardiogram “either previously labeled or first diagnosed’ were included.
Patients were not included in the research if they seem to be at very high risk for anesthesia, reluctant to modify lifestyle postoperative, on drugs or alcohol, previous bariatric procedure, pregnancy, or lactation at screening or surgery.
Besides, cases with RSVP ≤ 35 mmHg and those who did not finish the follow-up evaluation period, “there were 18 cases that were lost to follow-up” were precluded from the study. Furthermore, cases with inadequate acoustic windows that made echocardiogram technically difficult were not included in the analysis.
Data Registry
Initial variables comprised case demographics, initial weight, height, and body mass index (BMI). In addition, other data included the duration of PH in previously labeled cases, smoking history, associated comorbidities including diabetes mellitus, elevated blood pressure, dyslipidemia, obstructive sleep apnea “OSA,” gastro-esophageal reflux disease (GERD), chronic obstructive pulmonary disease (COPD), renal impairment (RI), and coronary artery disease (CAD).
Cases were decided for LSG after multidisciplinary group assessment, including surgeons, bariatric physicians, pulmonologists, cardiologists, anesthesiologists, psychologists, and nutritionists.
Sleeve Procedure
The operation was done by the same expert surgical group. A sleeve was tailored using a 36F bougie 3–4 cm from the pylorus and reaching to the angle of His. The entire staple line was strengthened with non-interrupted ligatures and examined for a leak by upper endoscopy. The gastric portion was retracted through the 15-mm trocar situated at the right upper abdomen. A closed suction drain was put in all cases and taken out 5 days postoperative.
Perioperative Assessment
Perioperative parameters comprised the American Society of Anesthesiologist (ASA) score, surgery duration, average blood loss, intraoperative problems, and postoperative hospitalization period. Early postsurgical problems (≤ 30 days) were subtyped as major problems and minor problems as per the American Society of Metabolic and Bariatric Surgery (ASMBS) outcome reporting standards [12].
Fifteen months later, patients were reassessed regarding new weight and BMI in addition to changes in concomitant metabolic comorbidities.
Most importantly, RVSP and right ventricular (RV) size were reassessed by the same experienced cardiologist, and changes were compared to the results of the preoperative evaluation.
Statistical Analysis
Data were tabulated using Excel 2010 and processed using SPSS version 20 for Windows 2010. For numerical variables, normally distributed data were presented in mean + SD, while abnormally distributed data were expressed in median and IQR. Categorical data were expressed in number and percentage. Quantitative data (numerical values) were compared using paired t test. The McNemar test was used to analyze the change in proportion for the paired nominal data. A univariate correlation analysis of the change in pulmonary hypertension with preoperative and postoperative covariates was performed, and independent factors having a P value < 0.150 were introduced in multiple linear regression analysis to identify independent factors affecting the change in pulmonary hypertension. P value ≤ 0.05 was considered statistically significant.
Results
Preoperative Data
A total number of 256 bariatric surgery candidates who presented during the study period underwent echocardiographic assessment; 55 patients had RVSP more than 35 mmHg by echocardiographic criteria and were enrolled in the study. Of these, 18 cases were lost to follow-up. So, the final analysis of the data was done to only 37 patients.
Demographic data of the patients are shown in Table 1.
Operative Details
The mean procedure time was 142 + (13.9) min. Only two patients had intraoperative complications, liver injury and hypoxia that were managed successfully (Table 2).
The hypoxia was due to bronchial spasm in a smoker patient with group III PH. It was rapidly corrected after adjusting oxygen parameters, frequent bronchodilators, and IV hydrocortisone.
30-Day Postoperative Details
Mean hospital stay was 2.67 + 0.816 days. Early postsurgical problems (less than 1 month) were encountered in 8 cases. Major complications were respirator failure, pulmonary embolism, pulmonary edema, and organ space surgical site infection. The first 3 necessitated ICU admission. Minor complications were in the form of wound infection, chest infection, and dehydration (Table 2).
Two patients developed more than one early postoperative problems. Respiratory comorbidities were recorded in 4 cases. Out of the 8 cases that experienced postsurgical comorbidities, none required revisional operations. There were no reported 1-month deaths in the studied group (Table 2).
Long-Term Follow-Up
At the end of the follow-up period (15 months), there was a significant improvement in the average weight and BMI (p value < 0.001). There was also a significant improvement in the metabolic parameters of the patients regarding diabetes, hypertension, and dyslipidemia. There was a significant drop of the RVSP and the RV size during the follow-up (p value < 0.001) (Table 3).
Notably, 33 patients out of all patients had their PH fallen below 30 mmHg. Five patients were able to discontinue their diuretic therapy, while four decreased their doses (from 40 to 80 mg furosemide daily to only 20 mg daily in the four cases). In addition, four patients discontinued their vasodilator therapy “sildenafil,” and two were able to decrease the required dosed (from 50 mg daily to 25 mg daily in the two cases). Similarly, two patients were able to discontinue home oxygen altogether, and one patient was able to decrease his oxygen requirements (from 3 L O2 nasal cannula to only 1 L).
Pre- and Postoperative Correlation Analysis
Univariate correlation analysis between all preoperative variables and pulmonary hypertension difference (pre- and postoperative RVSP) demonstrated a statistically significant negative correlation with three variables (age, hypertension, and vasodilator therapy) (Table 4); however, in addition to these three variables, right ventricular size (P = 0.070) and weight (P = 0.137) were introduced in the multiple linear regression analysis. Independent preoperative predictors affecting pulmonary hypertension were weight, RV size, hypertension, and vasodilator therapy (Table 5). The model successfully explained 39.2 % of the change in pulmonary hypertension (P = 0.001, adjusted R square = 0.392).
On the other hand, univariate correlation analysis between all postoperative variables and pulmonary hypertension difference demonstrated a statistically significant negative correlation with six variables (age, weight, total cholesterol, LDL cholesterol, vasodilator therapy, and RV size) (Table 6). In contrast, in multiple linear regression analysis, the independent predictors were dyslipidemia, weight, vasodilator therapy, and RV size (Table 7). Forty-two percent of the change in pulmonary hypertension was attributed to the predictors in the model (P < 0.001, adjusted R square = 0.421).
Discussion
PH is a clinical syndrome that is depicted by sustained elevated levels of PAP, which may finally result in right-sided heart failure and mortality [13].
Multiple factors are involved in the pathogenetic mechanisms of PH, such as insulin resistance, other aspects of metabolic syndrome, and adipokine dysfunction [14].
The effect of LSG on PH is not well understood. Metabolic surgery may possess endocrinal or metabolic impact that can have a direct impact on the pulmonary circulation [15]. A previous study demonstrated a substantial improvement after a bariatric procedure in a case with severe obesity and elevated PAP [15].
The main finding of this study is the considerable improvement of PH and right ventricular size in most of the studied patients with a notable coinciding reduction in the need for PH medications. Besides, our analysis showed marked improvement of other aspects of the metabolic syndrome post-LSG.
These results agree with the results obtained by Hanipah and colleagues 2018, who demonstrated that bariatric cases with PH attained a substantial weight reduction with a concomitant amelioration in RVSP [10]. Moreover, Sheu et al. found that laparoscopic gastric bypass and SG in obese cases amended PAP in the short term [6].
Additionally, two case reports were declared on the results of laparoscopic gastric bypass in two obese cases complaining of primary PH [15, 16]. Both cases demonstrated marvelous amelioration in functional capacity postoperatively, with associated amelioration in PAP and RV function.
PH can lead to perioperative significant cardiovascular complications. Meticulous choice of patients, determination of perioperative risk factors, and careful intraoperative hemodynamic assessment may decrease perioperative cardiovascular adverse events [17].
Previous research has shown that cases with PH who undergo non-cardiac operations had an elevated risk of adverse outcomes and death in comparison with those who do not have, regardless of the severity of the case [18].
Moreover, the Bariatric Outcomes Longitudinal Database (BOLD) reported that PH is considered an important predisposing factor of morbidity and mortality post metabolic operations. Chest infection and respiratory failure are major adverse outcomes in PH cases [19].
The current study showed an acceptable perioperative complication rate in PH undergoing bariatric surgery with no reported mortality. In agreement with this, a previous study found that metabolic surgery can be done without significant comorbidities in cases with PH [10].
These results may emphasize the role of multidisciplinary assessment, including skilled surgical, cardiopulmonary, and critical care groups, in the careful selection of such complex patient populations.
The present series suggested a possible benefit of LSG on PH in the obese population. LSG decreased the requirement for PH drugs and supplemental oxygen requirements.
The current work comprised cases with different subtypes of PH. Nevertheless, we could not decide whether particular subtypes of PH respond better than other types to LSG.
It should be noted that although smoking is counterproductive from metabolic, surgical, and cardiopulmonary perspectives, we included smokers to increase the number of the studied cohort for better validation of results.
The main limitation of this study was the quite large number of cases that were lost to follow-up (they did not come back for their scheduled appointments despite previous confirmations). Although patients could be dead or their cardiovascular conditions worsened, we had decided to include only those who finished the follow-up interval “which may have biased the results.” Nevertheless, a quite reasonable sample size and prospective study design are definite points of strength.
Other limitations of this work include non-consideration of changes in adipokines associated with weight loss and PH improvement, and the single-center nature of the work without a control cohort.
In conclusion, the present work suggests that LSG-induced weight loss can result in a considerable decrease of pulmonary pressures as well as RV size with a concurrent resolution of other metabolic comorbidities “although PH was diagnosed by indirect measures and most patients in this report remained within the diagnostic range for PH.” Prospective, more extensive studies are warranted (probably using the gold standard right heart catheterization) to explore the extent and durability of LSG as a successful strategy for PH and to determine favorable inclusion criteria for surgical candidates in such high-risk group.
What Is Already Known on This Topic
PH in obese cases has different pathogenetic mechanisms. LSG in these cases can lead to substantial weight loss with significant resolution of different comorbidities such as diabetes and hypertension; however, the effect of LSG on PH is still not precisely defined.
What Does This Study Add?
There are very few published data in the literature addressing PH in obese patients after LSG, and to our knowledge, the current work is the first prospective one in this field. Besides, one of the merits of this analysis is the considerable number of included patients with a quite long follow-up duration.
Pulmonary hypertension improvement after LSG might present as a new indicator or as a supplement to the indications of metabolic surgery, with the growing body of evidence that may be an aspect of the metabolic syndrome, yet this should be done on a case by case basis. Therefore, highlighting such field of research might be viewed as a novel, interesting point of the present study.
Abbreviations
- ASA:
-
American Society of Anesthesiologist
- ASMBS:
-
American Society of Metabolic and Bariatric Surgery
- BMI:
-
body mass index
- BOLD:
-
Bariatric Outcomes Longitudinal Database
- CAD:
-
coronary artery disease
- COPD:
-
chronic obstructive pulmonary disease
- GERD:
-
gastro-esophageal reflux disease and
- ICU:
-
intensive care unit
- LSG:
-
laparoscopic sleeve gastrectomy
- OSA:
-
obstructive sleep apnea
- PAH:
-
pulmonary arterial hypertension
- PAP:
-
pulmonary artery pressure
- PASP:
-
pulmonary artery systolic pressure
- PH:
-
pulmonary hypertension
- RI:
-
renal impairment
- RV:
-
right ventricular
- RVSP:
-
right ventricular systolic pressure
- STROBE:
-
STrengthening the Reporting of OBservational studies in Epidemiology
References
Perrotta F, Nigro E, Mollica M, et al. Pulmonary hypertension and obesity: focus on Adiponectin. Int J Mol Sci. 2019;20(4):912.
Taraseviciute A, Voelkel NF. Severe pulmonary hypertension in postmenopausal obese women. Eur J Med Res. 2006;11(5):198–202.
de Carvalho MH, Colaço AL, Fortes ZB. Cytokines, endothelial dysfunction, and insulin resistance. Arq Bras Endocrinol Metabol. 2006;50(2):304–12.
Ayinapudi K, Singh T, Motwani A, et al. Obesity and pulmonary hypertension. Curr Hypertens Rep. 2018;20(12):99.
Simonneau G, Gatzoulis MA, Adatia I, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2013;62:D34–41.
Sheu EG, Channick R, Gee DW. Improvement in severe pulmonary hypertension in obese patients after laparoscopic gastric bypass or sleeve gastrectomy. Surg Endosc. 2016;30:633–7.
Pugh ME, Robbins IM, Rice TW, et al. Unrecognized glucose intolerance is common in pulmonary arterial hypertension. J Heart Lung Transplant. 2011;30:904–2011.
Boza C, Salinas J, Salgado N, et al. Laparoscopic sleeve gastrectomy as a stand-alone procedure for morbid obesity: report of 1,000 cases and 3-year follow-up. Obes Surg. 2012;22(6):866–71.
Neagoe R, Muresan M, Timofte D, et al. Long-term outcomes of laparoscopic sleeve gastrectomy – a single-center prospective observational study. Wideochir Inne Tech Maloinwazyjne. 2019;14(2):242–8.
Hanipah ZN, Mulcahy MJ, Sharma G, et al. Bariatric surgery in patients with pulmonary hypertension. Surg Obes Relat Dis. 2018;14(10):1581–6.
Hoeper MM, Bogaard HJ, Condliffe R, et al. Definitions and diagnosis of pulmonary hypertension. J Am Coll Cardiol. 2013;62(Suppl):D42–50.
Brethauer SA, Kim J, el Chaar M, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Surg Obes Relat Dis. 2015;11:489–506.
Farber HW, Loscalzo J. Pulmonary arterial hypertension. N Engl J Med. 2004;351:1655–65.
Zamanian RT, Hansmann G, Snook S, et al. Insulin resistance in pulmonary arterial hypertension. Eur Respir J. 2009;33(2):318–24.
Mathier MA, Zhang J, Ramanathan RC. Dramatic functional improvement following bariatric surgery in a patient with pulmonary arterial hypertension and morbid obesity. Chest. 2008;133(3):789–92.
Pugh ME, Newman JH, Williams DB, et al. Hemodynamic improvement of pulmonary arterial hypertension after bariatric surgery: potential role for metabolic regulation. Diabetes Care. 2013;36(3):e32–3.
Smilowitz NR, Armanious A, Bangalore S, et al. Cardiovascular outcomes of patients with pulmonary hypertension undergoing noncardiac surgery. Am J Cardiol. 2019;123(9):1532–7.
Yang E. Perioperative management of patients with pulmonary hypertension for non-cardiac surgery. Curr Rheumatol Rep. 2015;17(3):15.
Maciejewski ML, Winegar DA, Farley JF, et al. Risk stratification of serious adverse events after gastric bypass in the bariatric outcomes longitudinal database. Surg Obes Relat Relat Dis. 2012;8:671–7.
Funding
This study was supported by the authors. No any other fund was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests
The authors declare that they have no conflict of interest.
Ethics Approval and Consent to Participate
The work’ protocol obtained the agreement of the institutional review board. All cases gave a written informed assent before enrollment.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Acknowledgements
1. Mohamed D Sarhan, MD
General Surgery Department, Faculty of medicine, Cairo University, Egypt
Drsarhan777@hotmail.com
00201005244713
2. Ahmed Abdallah, MD
General Surgery Department, Faculty of medicine, Cairo University, Egypt
Phone: 00201287406494
ahmed_safina92@yahoo.com
3. Ahmed Rabiee, MD
Internal Medicine Department, Faculty of medicine, Cairo University, Egypt
Phone: 00201023006629
Ahmedrabeeh2020@yahoo.com
4. Shaimaa Elkholy, MD
Author Accepted Manuscript
Internal Medicine Department, Faculty of medicine, Cairo University, Egypt
Phone: 00201060407761
shuma50082@gmail.com
5. Ahmed Soliman, MD
Internal Medicine Department, Faculty of medicine, Cairo University, Egypt
Phone: 00201222166979
drsolimans@yahoo.com
6. Ossama Ramzy Youssef, MD
Department of Anaesthesia and Intensive Care, Ain Shams University
dr.oramzy@yahoo.com
0020100 1429707
Rights and permissions
About this article
Cite this article
Salman, A.A., Salman, M.A., Shaaban, H.ED. et al. Effect of Bariatric Surgery on the Cardiovascular System in Obese Cases with Pulmonary Hypertension. OBES SURG 31, 523–530 (2021). https://doi.org/10.1007/s11695-020-04852-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04852-2