Abstract
Background
To analyze the results regarding weight loss and complications related to the Spatz3® adjustable intragastric balloon (IGB) in Brazil.
Methods
This randomized prospective study covered patients who had undergone treatment using a Spatz3® adjustable IGB between October 2016 and June 2018 at a private clinic in Rio de Janeiro, Brazil. The patients had a minimum body mass index (BMI) of 27 kg/m2. The study examined complications of Spatz3® treatment and BMI reduction, percentage of total weight loss (%TWL), and % of excess weight loss (%EWL).
Results
One hundred eighty patients underwent a Spatz3® balloon implant in the period. The patients were randomly divided into one group in which the Spatz balloon was kept at the same volume (600 mL) throughout treatment (Control Group), and another adjustment group with 250 mL greater volume. The complication rate was 16.14%. No death or major complication occurred during the study. Mean BMI decreased from 39.51 to 32.84 kg/m2 (p < 0.0001), bodyweight from 111.87 to 90.28 kg (p < 0.0001), and excess weight from 41.55 to 22.99 kg (p < 0.0001). The adjustment resulted in greater mean weight loss of 4.35 kg (− 8 to 17.6 kg), and the average time of the procedure was 7.12 ± 1.63 months. The upward adjustment group did not present greater %TWL, %EWL, or BMI reduction when compared with the control group (p = 0.4413, p = 0,9245, p = 0.2729, respectively).
Conclusion
This study shows that Spatz3® IGB treatment is an effective procedure for weight reduction, with no mortality but higher morbidity compared with traditional IGBs. This procedure also enabled the balloon to stay in place for longer. The efficacy of upward adjustment still requires further confirmation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity treatment involving an intragastric balloon (IGB) has already been established to be a safe and effective method [1,2,3]. The volume of the conventional IGB is fixed at the time of the placement and cannot be changed thereafter. The balloon may remain in the stomach for a maximum of 180 days and it is imperative that it be removed by this deadline [4, 5]. The Spatz3® liquid adjustable balloon was approved in May 2010 in all 27 countries of the European Union for patients with a body mass index (BMI) of more than 27 kg/m2 whose previous attempts at weight loss have failed. In November 2014, the Spatz3® balloon was approved for clinical use in Brazil. Spatz3® ® IGB is now in its third generation and is a safer device and easier to use compared with earlier generations [6].
The Tarpon Springs Conference, held in 1987 in Florida [7], established the criteria for an IGB. These included having variable filling volume capacity (400–700 mL), being filled with liquid (water or saline), having a radiopaque marker for monitoring and control, being made of resistant and durable material to prevent leaks, and having a smooth surface. According to these criteria, the Spatz3® IGB, when compared with a conventional one, is better according to the first criterion, since its volume can be controlled throughout treatment and not only at the time of implantation [8]. However, Spatz3® IGB performs worse on the last criterion, since it does not have a completely smooth surface, the site for insertion of the filling valve forming a sort of “tail” [8].
The two main differentiating features of the Spatz3® IGB are post-implantation volume control and the maximum treatment period of 360 days [2, 7, 8]. The volume of the balloon can be adjusted—upward or downward—throughout treatment. The volume of the balloon may be reduced in cases of intolerance (excessive and/or persistent vomiting for more than 7 days). Withdrawal of 100 to 300 mL of the IGB volume improves symptoms and enables the patient to continue treatment. The balloon may also be increased in volume during treatment, at a predetermined date or when the patient reports a decrease in satiety. Increasing the volume of the balloon may improve the balloon’s effect on weight loss by creating a heightened sensation of satiety and further restricting food intake [8]. Furthermore, the balloon can remain in place for a maximum of 360 days and may facilitate sustained weight loss for one full year, thus providing more time for the patient to undergo food reeducation [9].
Although the adjustable IGB seems to possess a number potential benefits compared with conventional balloons (greater tolerability, gradual effective weight loss, and longer duration of implantation) [10], to date, few studies (some with a small number of participants) have evaluated its safety and efficacy [2, 8, 11, 12]. Moreover, some reports raise questions regarding its long-term safety [13,14,15].
The aim of this study was thus to analyze the results regarding weight loss and complications related to use of a Spatz3® adjustable IGB at a private center in Brazil.
Methods
Study Design and Setting
This prospective randomized study covered patients undergoing treatment with a Spatz3® (Genco et al., 2013) [2] (Spatz ABS, Spatz FGIA, Inc., Jericho, NY, USA) between October 2016 and June 2018 at a private clinic (EndogastroRio) in Rio de Janeiro/Brazil.
Eligibility
Inclusion Criteria
-
Adult patients with a BMI ≥ of 27 kg/m2 who did not lose weight in well-conducted clinical treatments for overweight/obesity.
Exclusion criteria
-
Teenagers
-
Patients with obesity due to hormonal or genetic causes
-
Users of alcohol or illicit drugs
-
Patients with known malignancy
-
Pregnant women
Baseline Pharmacotherapy, Comorbidities, and Anthropometric Parameters
No pharmacotherapy had been applied prior to the procedure. Anthropometric measures were obtained at the baseline (day of IGB insertion) and 6 months later at the end of the study (day of IGB removal). Height was measured using a stadiometer accurate to ± 0.5 cm and weight was obtained using a scale calibrated to ± 0.1 kg after participants, without shoes and wearing light clothing, attempted to empty their bladder. BMI was calculated using the standard equation (kg/m2) and classified as pre-obesity (25.00–29.99), grade I obesity (30.0–34.9), grade II obesity (35.0–39.9), and grade III obesity (≥ 40.0) [9].
A preliminary interview with each study participant established medical history, including previous attempts to lose weight, comorbidities, and the impact of obesity, both on a social and psychological level. The comorbidities considered were dyslipidemia, type 2 diabetes mellitus, chronic kidney disease with hemodialysis, hypertension, hypothyroidism, hepatic steatosis, insulin resistance, sleep apnea, hyperuricemia, polycystic ovary syndrome, systemic lupus erythematosus, and kidney transplantation.
Randomization of Groups
Of the total of 293 participants, 113 were excluded for the reasons explained in Fig. 1, leaving 180. After the randomization process, performed using Minitab® software, 86 patients were allocated to the upward adjustment group, and 94 patients were allocated to the non-adjustment group (control group).
Ethical Considerations
The study was reviewed and approved by the Clinical Institutional Review Board and was conducted in accordance with the ethical standards laid out in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Interventions
Balloon Placement
Balloon insertion was performed subsequent to a diagnostic endoscopy to detect pathologies that contraindicate balloon placement, such as active peptic ulcer, grade C-D esophagitis, large volume hiatal hernia, esophageal/fundus varices, esophageal strictures, and prior gastric surgery.
The endoscopy procedure has carried out under deep sedation without endotracheal intubation, with continuous oxygen support of 5 L/min, under the supervision of an anesthesiologist. If there were no impediments, the procedure to implant the balloon was initiated.
In the conventional technique recommended by the manufacturer, the Spatz3® balloon is inserted along with the endoscope (the balloon attached to the scope). The balloon kit contains a “condom,” which is connected to the tip of the endoscope. Along with the “condom wrapper,” the balloon is placed next to the device. The “condom” is then placed over the balloon, attaching it to the device. The balloon + scope assembly is then heavily lubricated with an appropriate gel, and endoscope and balloon are inserted together, slowly and gently, into the patient. In the gastric cavity, it is recommended that the endoscope be put into rearview to confirm that the balloon is in fully gastric position and has not detached from the endoscope during insertion, thereby avoiding the risk of complications resulting from inflation of the balloon in the esophagus. Balloon inflation was carried out under direct view, with the endoscope remaining in rearview position. The balloon was inflated with saline (3%) and 10 mL of 4% methylene blue. The initial balloon volume was set at 600 mL.
After the inflation procedure, the filling catheter was pulled up until the balloon valve had been fully removed through the patient’s mouth. At this point, it is important to introduce a finger into the patient’s mouth and place it on the base of the tongue. The catheter and the valve slide over the finger, protecting the base of the tongue from possible damage caused by the passage of the valve and preventing localized bleeding. When the catheter has been disconnected from the valve, it is covered with a suitable cap topped by a blue nylon loop. Holding the loop, the valve is gently re-inserted into the patient and released at the oropharynx. The scope is used to position the valve inside the stomach and the balloon is then visually inspected to detect possible leaks or valve malfunctions and to confirm its correct positioning in the gastric fundus. If leakage is detected, the defective balloon is promptly replaced.
Follow-up
After IGB insertion, patients were kept for around 1–2 h in an anesthesia recovery room until full recovery from sedation, whereupon they were discharged. Instructions were provided for a 5-day liquid diet (with progressive increase in the volume ingested). On the sixth day, a semi-solid diet was prescribed and, after the thirteenth day, solids were introduced into a 1200 kcal/day diet. After this (maximum 15 days after IGB placement), the patients were referred for personalized nutritional counseling, in which an individual diet within a range of 10–15 kcal/kg/day was prescribed. A monthly follow-up with a multidisciplinary team (dietician, psychologist, and doctor) was offered to all patients.
During the first 3 days after balloon insertion, patients were instructed to use three antiemetic drugs (metoclopramide, ondansetron, and dimenhydrinate), an anti-foaming drug (dimethicone), and analgesics/antispasmodics (scopolamine plus dipyrone and acetaminophen). All patients were instructed to use a proton pump inhibitor (PPI; pantoprazole magnesium) throughout treatment—a double dose in the first month (80 mg) and a full dose from the second month (40 mg) to the end of treatment. Vitamin and mineral supplements and probiotics (Lactobacillus acidophilus LA 16) were also given to all patients throughout treatment.
Balloon Adjustment
The volume of the balloon could be adjusted downwards in patients who exhibited balloon intolerance and was adjusted upwards by a standard volume of 250 mL in the course of the treatment in those assigned to the adjustment group.
For 5 days before balloon adjustment, patients were instructed to restrict themselves to a liquid diet. The procedure was carried out under deep intravenous sedation. The endoscopy involved the following sequence of steps:
-
1.
blue nylon loop clasp of valve cap grasped with foreign body forceps;
-
2.
scope carrying the valve withdrawn, protective cap unscrewed, and same adjustment catheter as used for filling the implant connected;
-
3.
balloon volume reduced (aspirating the liquid inside the balloon out through the catheter with a 60 mL syringe) or increased (by injecting fluid in through the catheter using a 60 mL syringe);
-
4.
adjustment catheter pulled up to remove the valve through the mouth in the same way as the balloon implant and then disconnected from the valve;
-
5.
protective cover replaced;
-
6.
valve returned to the gastric cavity.
Balloon Removal
Removal was routinely planned for 360 days after insertion but in fact occurred after a minimum of 270 and a maximum of 390 days after balloon implantation. Removal was preceded by a 5-day clear-fluid diet, to minimize the risk of residual food entering the trachea. Deep intravenous anesthesia without tracheal intubation was used, with the patient in a lateral decubitus position. If remnants of solid food were found to be present in the stomach, the procedure was canceled and another with adequate preparation was scheduled.
All the liquid content of the mucosal lumen was aspirated. After insertion of the gastroscope into the stomach, a needle catheter was pushed down into the working channel of the gastroscope and introduced into the balloon after puncture. The needle was withdrawn, applying a vacuum to empty the balloon. Following intravenous administration of scopolamine for relaxation of the lower esophageal sphincter, the catheter was removed and the balloon was grasped with a polypectomy snare by the base of the “tail,” and slowly extracted through the esophagus. No cases of aspiration were observed during this procedure. After balloon removal, endoscopy was performed to identify any damage caused by the passage of the balloon.
Outcomes of Interest
Primary Outcome
In the group that received the upward adjustment, a statistically significant difference in weight loss was expected compared with that of the group that did not receive any adjustment in the balloon.
Secondary Outcome
The secondary outcomes investigated in the present study included safety (treatment complications) and efficacy indicators such as weight loss (kg), change in BMI (kg/m2), % total weight loss (%TWL), and % excess weight loss (%EWL) during balloon use (minimum 270 days). Anthropometric measures were obtained for the baseline (day of IGB insertion) and at the end of the study (day of IGB removal). Height was measured using a stadiometer accurate to ± 0.5 cm, and weight has obtained using a digital scale accurate to ± 0.1 kg (Filizola S.A., São Paulo, SP, Brazil), with participants without shoes and wearing light clothing, after having attempted to empty their bladder. Body mass index (BMI) was calculated using the standard equation (kg/m2). BMI cutoff points were used to classify the participants as overweight (25–29.9), class I obese (30–34.9), class II obese (35–39.9), or class III obese (≥ 40) [16]. Excess weight (EW) was determined as the amount of weight in excess of ideal body weight (determined to be a BMI of 24.9). The success of the treatment was evaluated according to two criteria:
-
1)
the percentage of excess weight loss (%EWL): patients who did not achieve the goal of the treatment (< 20%), those with successful treatment (20–50%), and those with highly successful treatment (> 50%) [17] and;
-
2)
the percentage of total weight loss (%TWL): patients who did not achieve the goal of the treatment (< 10%), and those with successful treatment (≥ 10%) [17].
Statistical Analysis
For data analysis, a database was drawn up using a Microsoft Excel spreadsheet exported to the Minitab 18® statistical program (version 18, Minitab, LLC, State College, Pennsylvania, USA) (Minitab®) and also to OriginPro® 9 (DPR Group, Inc., Northampton, Massachusetts, USA) (Moberly, Bernards, Waynant, 2018). The Kolmogorov-Smirnov test for normality was used to confirm the normal distribution of the variables. The results are presented as mean ± standard deviation for numerical variables and absolute numbers (percentage) for categorical variables. A paired Student’s t test was used for comparisons between values obtained at the baseline and at the end of the treatment and a non-paired t test for comparisons between patients undergoing the upward balloon adjustment and those who did not. Comparisons between different reductions in total weight loss and excess weight loss, with and without Spatz3® adjustment, were made using one-way analysis of variance (ANOVA). Multivariate (dendogram) analysis was also performed to discover the degree of similarity (%) between mean %TWL and mean %EWL for all groups. In all statistical analyses, a p value < 0.05 was considered to be significant.
Results
The baseline patient characteristics are presented in Table 1. Of these patients (n = 180), eight (4.44%) were intolerant to the balloon between 2 and 4 weeks and agreed to volume adjustment. In four patients, the downward adjustment was performed in the second week after implantation and, in four others, in the fourth week. The range of volume removed was 220 mL (150–400 mL). An upward adjustment was carried out in 86 patients, three of whom (6.52%) presented intolerance after this procedure. All of the patients 1 week later underwent a downward adjustment of 50% of the volume added by upward adjustment (150–210 mL) and remained in treatment.
Changes in body weight, BMI, and EWL are shown in Table 2. The data are reported for the group of patients as a whole and separately for those who underwent the upward adjustment (n = 86) and those who underwent no adjustment (n = 94). There was a significant decrease in all nutritional parameters during the study period.
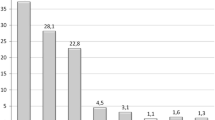
Complications were analyzed for the total number of patients in the study period (n = 180, 34.4% males). The complications occurring during treatment were as follows: spontaneous deflation (three, 1.66%), early retrieval unrelated to adaptation period symptoms (twelve, 6.66%), early retrieval due to prolonged adaptation period symptoms and rejection by the patient or impossibility proceeding with balloon placement (two, 1.11%), Mallory-Weiss syndrome (one, 0.55%), gastric ulcer leading to early retrieval (one, 0.55%), gastric ulcer diagnosed during the treatment without the need to remove the balloon (five, 2.77%), and gas production inside the balloon (one, 0.55%). No deaths occurred as a result of complications.
Eighty-six patients (47.78%) underwent upward adjustment. The adjustment resulted in further mean weight loss of 4.2 kg (− 9 to 20 kg). The standard upward adjustment volume was 250 mL, and the procedure was carried out after 7.06 ± 1.64 months (2–10). The upward adjustment group did not exhibit higher %TWL, %EWL, or higher BMI reduction compared with the group with no adjustment (p = 0.4413, p = 0.9245, and p = 0.2729, respectively).
Four patients (22.22%) did not meet the treatment goal in terms of %EWL (EWL < 25%). Fifty-two patients (28.89%) did not achieve treatment success for %TWL (TBWL < 10%). Twenty-one patients (11.66%) concluded the study with a BMI of 25 kg/m2 (Table 2). The success rate was higher in patients who underwent the upward adjustment (77.91%) compared with those who did not (64.89%).
Figures 2 and 4 show the dendogram graphs along with the degree of percentage similarity between average reduction in total weight loss (TWL) and the excess weight loss (EWL), with and without adjustment of Spatz3®. The results show that the degree of similarity between TWL with and without adjustment of Spatz3® was 77.07% (22.93% difference between them) and the degree of similarity for EWL was 76.44% (23.56% difference between them) (Figs 3 and 4).
Furthermore, Figs. 3 and 5, using the Box-Plot graph, intervals and mean and median TWL and EWL reduction values with and without Spatz3 ® adjustment, show that there was a statistically significant difference for both comparisons, with p = 0.056 > 0.05 and p = 0.058 > 0.05, respectively.
Discussion
IGB treatment is a well-recognized therapy for overweight/obesity [2, 3, 18, 19] and has been successfully used to generate weight loss for the last 20 years [11]. The mechanism of action of an IGB is multifactorial and incompletely understood [20, 21]. Theoretically, an IGB affects both the stretch receptors and gastric capacity, increases satiety while decreasing the residual volume available for food, and also increases gastric emptying time. It could therefore be considered a restrictive procedure for treating obesity [22]. Other proposed mechanisms include changes in appetite-regulating hormones (a decrease in ghrelin and leptin and an increase in CCK concentrations). However, there are conflicting reports regarding these. [20, 21] The best results with IGB occur when treatment is combined with behavioral changes [2, 3, 18, 19].
However, it is not possible to establish the ideal balloon size for a specific patient, since the threshold for nausea, vomiting, and abdominal pain are not measurable or predictable [8]. Moreover, some studies have demonstrated a decrease in IGB efficacy in promoting weight loss due to a reduction in the satiety effect after 3 months [22,23,24]. However, the traditional IGB has some limitations: a decrease in the efficacy of promoting weight loss after 2 to 3 months, a maximum length of treatment of 6 months, and a significant rate of complications during the early implantation period (nausea, vomiting, and discomfort), leading to balloon extraction in 4–5% of patients [5, 18, 22,23,24] [8]. The introduction of the Spatz3® Adjustable Balloon system provides features that address these limitations.
The main complication was the early removal of the balloon (removal < 9-month post-implantation). However, in most cases (n = 12, 6.66%), this was not due to adaptation symptoms, but for various other reasons, such as a desire to give up the treatment, weight loss considered insufficient by the patient, and psychological intolerance (desire to eat, to remove the device from inside the body). Only two removals (1.11%) were performed because of severe symptoms (excessive vomiting) in patients who did not wish to make the downward adjustment and decided to abandon treatment. The incidence of early removal in the present study was 7.77%, which is similar to that observed in other studies of the Spatz. Machytka et al. (2014) [6] reported 7.79%, Brooks et al. (2014) [11] 5.47%. However, this rate is higher than that observed in studies conducted using a conventional IGB for which Genco et al. (2005) [9] reported 0.44%, Lopez-Nava et al. (2011) [18] 0.8%, and Sallet et al. (2004) [1] 3.4%. It is important to note that, of the 14 early removals in this study, only two (1.24%) were due to intolerance, which is a similar rate to that previously described. Furthermore, all patients who underwent downward adjustment (n = 8; 4.44%), without exception, completed the minimum 9-month treatment, as observed in other Spatz® IGB studies [6, 11]. It thus seems that downward balloon adjustment may contribute to better adaptation and a lower removal rate.
There were three cases (1.66%) of spontaneous deflation prior to 9-month post-implantation—the minimum length of time established for treatment. In these cases, the defective balloon was replaced immediately and treatment continued. This rate is lower than that reported by Machytka et al. (2011) [8] for Spatz® (11.11%). Their study, however, used first and second-generation Spatz® balloons, while the present study used only the third generation, which has been described as having easier implantation and extraction procedures, which are less complicated and require fewer steps [6]. The spontaneous deflation index of the present study (1.66%) was lower than that found in a study conducted by Brooks et al. (2014) (4.1%) [11], who also used third generation Spatz® balloons.
In one (0.55%) patient, gas production inside the balloon was detected in the tenth week of treatment, when the patient started to vomit again. An x-ray of the abdomen was performed to gauge the air-fluid level inside the balloon. The balloon was then completely emptied and filled again with 3% sterile saline plus 10 mL of 4% methylene blue. The patient continued treatment without any problems or need for removal or replacement of the balloon. This complication has not been reported in any other Spatz® balloon study and it is believed to have occurred as a result of contamination of the liquid inside the balloon by anaerobic bacteria from the gastrointestinal tract.
There was one case (0.55%) of upper gastrointestinal bleeding without hemodynamic repercussions. Endoscopy detected a laceration in the gastroesophageal junction due to excessive vomiting after an upward balloon adjustment. Half of the upward adjustment volume was then removed, resulting in prompt improvement of symptoms and continuation of treatment, with no need for balloon removal. Machytka et al. (2014) [6] also reported one case (1.29%) of upper gastrointestinal bleeding, in their case due to gastric ulcer.
Six gastric ulcers (3.33%) were diagnosed in the lesser curvature of the gastric antrum. One of these (0.55%) necessitated removal of the balloon due to the intense pain and depth of the lesion. When asked, the patient reported not having taken the prescribed proton pump inhibitor (PPI). Five (2.77%) other ulcers were asymptomatic and were diagnosed during treatment (during an adjustment procedure) or on removal of the balloon. All were treated conservatively by increasing the dose of PPI and sucralfate, with the adequate response and healing of the lesion. The incidence of ulcers is higher in studies using Spatz® balloons (Machytka et al. (2014) [6], 1.29% and Brooks et al. (2014) [11], 2.73%) than in those using traditional balloons (Genco et al. (2005) [2], 0.2% and Sallet et al. (2004) [1], 0%). This may be explained by the fact that the Spatz® balloon does not have a completely smooth surface because of its “tail,” which acts as a compression point on the gastric mucosa [8] and could generate a pressure ulcer. In this study, there were no cases of gastric perforation, esophageal perforation, or death.
Weight loss has traditionally been the main outcome measure of the efficacy of IGB treatment and was observed in the majority of our patients. The %EWL in the present study was similar to or slightly higher than that observed in other Spatz® series reported in the literature [6, 8, 9, 11, 12].
However, weight loss after upward adjustment in the present study was lower than in other Spatz® studies [6, 8, 9, 11, 12]. This may be due to the fact that, in our study, the upward adjustment was performed later (7.12 ± 1.63 months) than in the studies conducted by Machytka et al. (2014) [6] and Brooks et al. (2014) [11], in which the mean adjustment time was 4.1 and 5.8 months, respectively, allowing more time for further weight loss, or more likely, upward adjustment is not effective in promoting extra weight loss.
In this study, the upward adjustment was carried out in all patients in the upward adjustment group. The incidence of this procedure (47.77%, n = 86 of 180) was higher compared with the Spatz® series of Genco et al. (2013) [9] and Machytka (2014) [6], with 22.5% and 19.48% of upward adjustments, mainly for reason of the patient reaching a weight plateau. However, the percentage of excess weight loss of patients who underwent adjustment was not significantly higher compared with those who did not. Similarly, Genco et al. (2013) [9] reported that the final mean BMI of the patients who underwent upward adjustment was higher than patients with Spatz® who did not. However, this was not statistically significant and the authors pointed out that this occurred only in a small number of patients and needs to be confirmed.
The sample size in our study model is limited but reasonable for a prospective study and larger than other studies with this type of balloon. The study has limitations, the main one being the absence of a sham group, which is difficult to provide in a private center. However, in our opinion, the possibility of evaluating the real-life tolerance, efficacy, and complications associated with the use of Spatz3® IGB and the presence of a control group (non-adjustment group) compensates for the absence of a sham group.
The extended length of treatment (1 year) enables more extensive nutritional counseling, to increase patient compliance and to reinforce the need for changes in behavior beginning in the very early stages of treatment. Patients should be aware that it is important not only to lose weight but also to sustain this loss, as noted by various authors [17, 25, 26]. Even 1 year after treatment, the majority of the patients were still obese (final BMI 32.84 kg/m2, only four patients with BMI < 25 kg/m2). Spatz3® use does not constitute a definitive treatment for obesity and needs to be combined with permanent changes in behavior and a probable second balloon treatment. At the time of writing, there is no contraindication for use of the Spatz3® for sequential therapy, as with traditional IGBs [9].
The present study therefore showed that Spatz3® IGB treatment is an effective procedure for weight reduction with no mortality. Currently, IGBs represent a safe and effective weight loss option for patients. It is clear that downward adjustment reduces the incidence of early removals due to intolerance. However, it is not clear whether upward adjustment is effective in promoting extra weight loss, since none of the parameters examined exhibited a statistical difference between the two groups. On the other hand, the adjustment group showed a slightly higher treatment success rate and also made it possible to maintain the balloon in the stomach for a longer period of time. Additional clinical trials are needed to understand the difficulties and problems associated with Spatz3® IGB use, and the efficacy of the upward adjustment.
References
Sallet JA, Marchesini JB, Paiva DS, et al. Brazilian multicenter study of intragastric balloon. Obes Surg. 2004;14:991–8.
Genco A, Bruni T, Doldi SB, et al. BioEnterics Intragastric balloon: the Italian experience with 2,515 patients. Obes Surg. 2005;15:1161–4.
Forlano R, Ippolito AM, Iacobellis A, et al. Effect of the BioEnterics intragastric balloon on weight, insulin resistance, and liver steatosis in obese patients. Gastrointest Endosc. 2010;71:927–33. https://doi.org/10.1016/j.gie.2009.06.036.
Wahlen CH, Bastens B, Herve J, et al. The bio enterics intragastric balloon (BIB): how to use it. Obes Surg. 2001;11:524–7.
Imaz I, Martínez-Cervell C, García-Alvarez EE, et al. Safety and effectiveness of the intragastric balloon for obesity. A meta-analysis. Obes Surg. 2008;18:841–6. https://doi.org/10.1007/s11695-007-9331-8.
Machytka E, Brooks J, Buzga M, et al. One year adjustable intragastric balloon: safety and efficacy of the Spatz3 adjustable balloons [v1; ref status: approved with reservations 2, http://f1000r.es/471]. F1000Research. 2014;3:203. https://doi.org/10.12688/f1000research.5099.1.
Schapiro M, Benjamin S, Blackburn G, et al. Obesity and the gastric balloon: a comprehensive workshop. Tarpon Springs, Florida, March 19-21, 1987. Gastrointest Endosc. 1987;33:323–7.
Machytka E, Klvana P, Kornbluth A, et al. Adjustable intragastric balloons: a 12-month pilot trial in endoscopic weight loss management. Obes Surg. 2011;21(10):1499–507. https://doi.org/10.1007/s11695-011-0424-z.
Genco A, Dellepiane D, Baglio G, et al. Adjustable intragastric balloon vs non-adjustable intragastric balloon: case-control study on complications, tolerance, and efficacy. Obes Surg. 2013;23(7):953–8. https://doi.org/10.1007/s11695-013-0891-5.
Sampath K, Dinani AM, Rothstein RI. Endoscopic devices for obesity. Curr Obes Rep. 2016;5(2):251–61. https://doi.org/10.1007/s13679-016-0217-8.
Brooks J, Srivastava ED, Mathus-Vliegen EM. One-year adjustable intragastric balloons: results in 73 consecutive patients in the U.K. Obes Surg. 2014;24(5):813–9. https://doi.org/10.1007/s11695-014-1176-3.
Russo T, Aprea G, Formisano C, et al. BioEnterics Intragastric Balloon (BIB) versus Spatz adjustable balloon system (ABS): our experience in the elderly. Int J Surg. 2017;38:138–40. https://doi.org/10.1016/j.ijsu.2016.06.013.
Kim SH, Chun HJ, Choi HS, et al. Current status of intragastric balloon for obesity treatment. World J Gastroenterol. 2016;22(24):5495–504. https://doi.org/10.3748/wjg.v22.i24.5495.
Daniel F, Abou Fadel C, Houmani Z, et al. Spatz 3 adjustable intragastric balloon: long-term safety concerns. Obes Surg. 2016;26(1):159–60. https://doi.org/10.1007/s11695-015-1897-y.
Yap Kannan R, Nutt MR. Are intra-gastric adjustable balloon system safe? A case series. Int J Surg Case Rep. 2013;4(10):936–8. https://doi.org/10.1016/j.ijscr.2013.07.025.
Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63:2985–3023. https://doi.org/10.1016/j.jacc.2013.11.004.
Herve J, Wahlen CH, Schaeken A, et al. What becomes of patients one year after the intragastric balloon has been removed? Obes Surg. 2005;15:864–70.
Lopez-Nava G, Rubio MA, Prados S, et al. BioEnterics® Intragastric Balloon (BIB®). Single ambulatory center Spanish experience with 714 consecutive patients treated with one or two consecutive balloons. Obes Surg. 2011;21:5–9. https://doi.org/10.1007/s11695-010-0093-3.
Stimac D, Majanović SK, Turk T, et al. Intragastric balloon treatment for obesity: results of a large single center prospective study. Obes Surg. 2011;21:551–5. https://doi.org/10.1007/s11695-010-0310-0.
Papademetriou M, Popov V. Intragastric balloons in clinical practice. Gastrointest Endosc Clin N Am. 2017;27(2):245–56. https://doi.org/10.1016/j.giec.2016.12.006.
Laing P, Pham T, Taylor LJ, et al. Filling the void: a review of intragastric balloons for obesity. Dig Dis Sci. 2017;62(6):1399–408. https://doi.org/10.1007/s10620-017-4566-2.
Mion F, Napoléon B, Roman S, et al. Effects of intragastric balloon on gastric emptying and plasma ghrelin levels in nonmorbid obese patients. Obes Surg. 2005;15:510–6.
Mui WL, Ng EK, Tsung BY, et al. Impact on obesity-related illnesses and quality of life following intragastric balloon. Obes Surg. 2010;20(8):1128–32. https://doi.org/10.1007/s11695-008-9766-6.
Al Kahtani K, Khan MQ, Helmy A, et al. Bio-enteric intragastric balloon in obese patients: a retrospective analysis of King Faisal Specialist Hospital experience. Obes Surg. 2010;20(9):1219–26. https://doi.org/10.1007/s11695-008-9654-0.
Kotzampassi K, Grosomanidis V, Papakostas P, et al. 500 intragastric balloons: what happens 5 years thereafter. Obes Surg. 2012;22:896–903. https://doi.org/10.1007/s11695-012-0607-2.
Dastis NS, François E, Deviere J, et al. Intragastric balloon for weight loss: results in 100 individuals followed for at least 2.5 years. Endoskopie Heute. 2009;22:151–8. https://doi.org/10.1055/s-0029-1214826.
Funding
This article is supported by EndogastroRio Clinic, Rio de Janeiro-RJ, Brazil.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Core tip: The present study analyzed the results and complications of patients undergoing treatment for overweight using a Spatz3® adjustable balloon, which had the potential for adjustment of volume during treatment, which may lead to a lower incidence of early removal due to intolerance when downward adjustment is performed, and to greater weight loss when the adjustment performed during treatment is upward. However, these benefits carry the risk of a number of complications, which are of low severity but somewhat greater in number than those associated with the traditional balloon.
Rights and permissions
About this article
Cite this article
Fittipaldi-Fernandez, R.J., Zotarelli-Filho, I.J., Diestel, C.F. et al. Randomized Prospective Clinical Study of Spatz3® Adjustable Intragastric Balloon Treatment with a Control Group: a Large-Scale Brazilian Experiment. OBES SURG 31, 787–796 (2021). https://doi.org/10.1007/s11695-020-05014-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-05014-0