Abstract
Purpose
The effectiveness of the standard biliopancreatic diversion with duodenal switch (BPD/DS) in terms of weight loss has been demonstrated. Increasing the strict alimentary limb length while maintaining the length of the common channel could lead to similar weight loss while reducing side effects.
Materials and Methods
The objective was to evaluate the effect of increasing the strict alimentary limb length on weight loss, comorbidities, nutritional deficiencies, and quality of life 2 years after surgery, compared with standard BPD/DS. An exploratory randomized, double-blind study evaluated the results of LADS at 2 years in comparison with the standard BPD/DS. Common channel was kept at 100 cm in both groups while alimentary limb was created at 100 cm from Treitz angle in the LADS group and at 150 cm total in the BPD/DS group.
Results
Twenty patients were recruited from May 2013 to June 2015. Mean percentage of excess weight loss was statistically significantly lower in the LADS group at 24 months (81.6 ± 6.6% in the LADS group and 97.1 ± 11.1% in the BPD/DS group (p = 0.001). No significant difference regarding the rate of remission of comorbidities was noted. Mean calcium, vitamin D, hemoglobin, zinc, and copper levels were statistically lower in the BPD/DS group. Quality of life was significantly improved in both groups, with no statistically significant difference between the two groups.
Conclusions
At 24 months, weight loss was lower in the LADS group. However, no difference was observed in the improvement in quality of life. LADS technique was discontinued following this study.
Trial registration
ClinicalTrial.gov Ref. NCT03097926
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity has now become a global public health problem. The Canadian population is no exception to this trend: the latest available data from 2009 to 2011 showed an obesity prevalence of 26.1% in the adult population [1]. Moreover, over the past four decades, this prevalence has been increasing [1, 2]. Obesity is a chronic disease, leading to the development of several comorbidities such as T2D, dyslipidemia, and hypertension. Bariatric surgery is the most effective long-term option in case of severe obesity. Different types of bariatric surgeries exist. The biliopancreatic diversion with duodenal switch (BPD/DS) was described in the early 1990s by Hess and Marceau [3]. BPD/DS results in an excellent weight loss, with an average percentage of excess weight loss (EWL) of 70% [4]. In addition, it leads to resolution or improvement in most obesity-related diseases. However, patients are at a lifelong risk of protein malnutrition or deficiency in fat-soluble vitamins and trace elements. In addition, gastrointestinal side effects can be bothersome [5]. The purpose of this study is to determine whether increasing the strict alimentary limb while maintaining the common channel at 100 cm can yield similar benefits compared with standard BPD/DS while improving side-effect profile. We present the results at 2 years of a prospective randomized trial comparing the two techniques. The 1-year results were published in Surgery for Obesity and Related Diseases in January 2018 [6].
Material and Methods
Trial Design
This exploratory randomized, double-blind (patient and evaluator) study was conducted in a university-affiliated tertiary care center (Institut universitaire de cardiologie et pneumologie de Québec, IUCPQ). The study protocol was approved by our ethic committee and recorded in a public registry (ClinicalTrial.gov Ref. NCT03097926).
Enrollment and Randomization of Patients
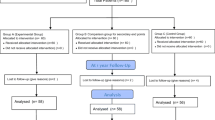
Patients were initially referred to our center for a bariatric procedure evaluation. Patients included were 18 to 60 years of age and fulfilled the National Institutes of Health (NIH) recommendations for bariatric surgery [2]; we included patients with a body mass index (BMI) of > 40 kg/m2 and patients with a BMI of > 35 kg/m2 with comorbidities related to obesity. We excluded patients who had specific contraindications to biliopancreatic diversion with duodenal switch [3] (irritable bowel syndrome, inflammatory bowel disease, chronic narcotic consumption, etc.), a BMI ≥ 50 kg/m2, a pacemaker, or cirrhosis, or who were planning to become pregnant in the next 2 years. Informed consent to participate in this research trial was obtained, and patients were randomly assigned to the group “standard BPD/DS” (control group) or to the group “modified biliopancreatic diversion with a longer strict alimentary limb” (LADS, study group) with an allocation ratio of 1:1. Sealed and opaque envelopes containing the assignation were prepared by a research nurse in a sequence randomly generated by computer. An envelope was then randomly given to the surgeon and opened at the beginning of surgery. Five different surgeons participated to the study. Patients, nurses, and nutritionists were blinded to the allocation group. A different surgeon who was not aware of the patient allocation group was responsible for the follow-up. There was no significant change to methods after trial commencement.
Preoperative Workup
A multidisciplinary team including a bariatric surgeon, a nutritionist, and a specialized bariatric nurse evaluated all the patients. A sleep apnea screening test was systematically done, and as needed, a consultation with a sleep medicine specialist was ordered. At the initial visit, demographic data (age, sex) and preoperative comorbidities (T2D, arterial hypertension, dyslipidemia, sleep apnea, asthma, obstructive pulmonary disease, and coronary artery disease) were noted. Vital signs, weight, height, BMI, and waist circumference were measured. Four-electrode full-body bioimpedance was used to measure lean body mass, body fat mass, and percentage of body fat. Preoperative blood tests included a complete blood cell count, liver enzymes, albumin, calcium, vitamin D, parathyroid hormone, vitamin A, serum iron, ferritin, glycated hemoglobin, total cholesterol, triglyceride, high-density lipoproteins, low-density lipoproteins, Apo-B, and trace elements (chromium, copper, molybdenum, zinc, selenium, and manganese). Patients completed the Laval questionnaire [7] about quality of life and a questionnaire on gastrointestinal symptoms.
Surgical Technique
All patients received routine antibioprophylaxis and thromboprophylaxis. Patients were positioned in split-leg position. The technique for the standard BPD/DS has been reported before [8] and consisted in the creation of a 100-cm common channel and a 150-cm strict alimentary limb, in addition to a sleeve gastrectomy (SG). For the LADS group, the gastrectomy was fashioned using the same technique, over a 42 French bougie. The small intestine was transected 100 cm distal to the Treitz ligament and anastomosed to the first duodenum. The biliopancreatic limb (measuring 100 cm) was anastomosed to the ileum, 100 cm proximal to the caecum. Figure 1 illustrates the limb lengths of the standard BPD/DS and the modified BPD/DS. The whole intestinal length was measured in both groups. All patients had a routine cholecystectomy. The mesenteric and Peterson defects were closed.
Standard BPD/DS: fixed 100-cm common channel and 150-cm strict alimentary limb with the remaining bowel as the biliary limb (± 600 cm). LADS: fixed 100-cm common channel and 100-cm biliary limb with the remaining bowel as the strict alimentary limb (mean length of 570 ± 97 cm). *Original source: Cloutier A, Lebel S, Hould F, Julien F, Marceau S, Bouvet L, et al. Long alimentary limb duodenal switch (LADS): a short-term prospective randomized trial. Surgery for Obesity and Related Diseases. 2018 Jan; 14(1):30–7. Permission has been obtained from IUCPQ
Vitamin Supplementation
After their surgery, all patients left with a prescription of multivitamin (Centrum Forte) BID, calcium carbonate 500 mg BID, vitamin D 20,000 IU DIE, vitamin A 30,000 IU DIE, and ferrous sulfate 300 mg HS. The dosage was then adjusted according to the results of the laboratories carried out at all follow-ups.
Outcomes
The primary outcome of this study was to compare LADS group weight loss at 6, 12, 18, and 24 months to the conventional BPD/DS group weight loss. This primary outcome was presented as a percentage of excess weight loss and percentage of total weight loss. Other dependent variables calculated were BMI, BMI variation, lean body mass, body fat mass, and percentage of body fat mass. Among the secondary outcomes, the evolution of comorbidities at 24 months (T2D, arterial hypertension, dyslipidemia, sleep apnea) was measured. Standard definitions were used to measure the presence and evolution of comorbidities [9]. A pre-existing diagnosis was established when the patient had a prescribed medication or continuous positive airway pressure (CPAP) to treat the comorbidity. A new diagnosis of T2D was made if glycated hemoglobin was greater than 6.5%, of arterial hypertension if blood pressure exceeded 140/90 mmHg, and of dyslipidemia if the ratio of total cholesterol/high-density lipoprotein (HDL) was greater than 4.44. T2D was considered cured if glycated hemoglobin was less than 6% or fasting blood glucose was below 6.0 without the use of antidiabetic medication. Arterial hypertension was considered cured if the blood pressure was less than 120/80 mmHg without medication. Dyslipidemia was considered to be resolved if, without medication, the total cholesterol/HDL ratio was less than 4.44. In order to confirm the resolution of sleep apnea, polysomnography demonstrating the absence of sleep apnea was necessary. The nutritional parameters at 12 and 24 months were measured as well as the total number of vitamin and mineral tablets and the average daily dosage of the main vitamins. Complications, reoperations, and hospitalizations were recorded for each group. Quality of life was measured at 12 and 24 months using a questionnaire validated in patients with morbid obesity (Laval questionnaire). This survey includes 44 items divided into 6 domains: activity/mobility, symptoms, personal hygiene/clothing, emotions, social interactions, and sexual life [7]. Each category was graded on a scale from 1 to 7, 7 meaning no complaint at all. Finally, we assessed the presence of gastrointestinal symptoms as abdominal bloating, stool odor, number of stools, and problems with stool frequency. These variables were measured during clinical follow-up at 3, 6, 9, 12, 18, and 24 months postoperatively.
Statistical Methods
Continuous data were presented as mean with standard deviation. The normal distribution of the data was verified by analyzing the histograms and by using the Shapiro-Wilk statistical test. Student T test was used to compare averages of normally distributed data. In cases where the distribution was not Gaussian, a Mann-Whitney U test for independent samples was used. Categorical data were presented in terms of number and percentage. Fisher’s exact test was used to compare categorical data. A signed Wilcoxon associated sample rank test was used to compare quality of life scores and stool counts before and after the procedure. Statistical significance was set at p < 0.05.
Results
Twenty patients were enrolled from May 2013 to June 2015. The two groups were similar for age, sex, BMI, weight, and comorbidities (Table 1). All surgeries were completed laparoscopically. Mean operative time was 203.3 ± 50.8 min in the LADS group and 161.3 ± 16.9 in the BPD/DS group (p = 0.03). Mean total intestinal length and mean strict alimentary limb length were respectively 769.5 ± 96.9 and 569.5 ± 96.9 cm in the LADS group and 795.0 ± 66.1 and 150 cm in the BPD/DS group. The difference between the mean total intestinal lengths was not statistically significant between the two groups (p = 0.52). The mean hospital stay was 4.0 ± 1.3 days in the LADS group and 2.8 ± 0.6 in the BPD/DS group (p = 0.01).
Primary Outcome
All the patients completed the 24-month follow-up. The mean percentage of excess weight loss (EWL%) and the mean percentage of total weight loss (TWL%) are illustrated over time in Figs. 2 and 3, respectively. The difference in the mean EWL% was statistically significant between the two groups at 24 months: 81.6 ± 6.6% in the LADS group and 97.1 ± 11.1% in the BPD/DS group (p = 0.001). The mean TWL% at 24 months was 40.9 ± 3.7% in the LADS group and 48.3 ± 4.9% in the BPD/DS group (p = 0.001). Mean BMI at 24 months was 27.2 ± 1.5 kg/m2 with a change in BMI of 18.8 ± 2.0 kg/m2 and 23.8 ± 2.7 kg/m2 with a change of 22.0 ± 2.3 kg/m2 in the LADS and BPD/DS groups, respectively (p = 0.002, p = 0.004). At 24 months, 1 patient had a BMI less than 20 (19.8) in the BPD/DS group. At 24 months, 1 patient in the BPD/DS group had a BMI greater than 30. At 24 months, the lean body mass was 51.9 ± 7.3 kg in the LADS group and 50.7 ± 11.4 in the BPD/DS group (p = 0.8). At the same postoperative period, the body fat mass and the percentage of body fat were 22.5 ± 6.6 kg and 30.2 ± 7.6% in the LADS group and 14.5 ± 4.8 kg and 22.3 ± 6.4% in the BPD/DS group (p = 0.006 and 0.02, respectively).
Secondary Outcomes
Co-morbidities at 24 months are shown in Table 2. As illustrated, no significant difference was observed between the two groups. The mean glycated hemoglobin was 0.04 ± 0.01 in the LADS group and 0.04 ± 0.004 in the BPD/DS group (p = 0.88). Every patient in the groups had a glycated hemoglobin under 0.06 at 24 months. The mean cholesterol ratio (total cholesterol/HDL) was 2.5 ± 0.7 in the LADS group and 2.4 ± 0.6 in the BPD/DS group (p = 0.85) at 24 months. Nutritional parameters at 0, 12, and 24 months are reported in Table 3. Initially, no difference was found between the two groups. At 24 months, mean calcium, vitamin D, hemoglobin, zinc, and copper were statistically lower in the BPD/DS group than in the LADS group. In addition, the incidence of vitamin D deficiency was significantly more frequent after BPD/DS (0 versus 56% at 24 months). At 24 months, the mean daily dosage of the main vitamin supplements and the mean total number of tablets of vitamin and mineral supplements were not statistically different between the two groups, even though it was at 12 months (Table 4). At 12 months, 2 patients in the BPD/DS group were using pancreatic enzymes to treat a mild malnutrition (albumin level under 30 g/dl). At 24 months, 1 patient in the BPD/DS group was still using pancreatic enzymes. The difference between the two study groups was not statistically significant (p = 0.48 at 12 months, and p ≥ 0.99 at 24 months).
The quality of life data from the Laval questionnaire is shown in Figs. 4 and 5 for each group preoperatively and at 12 and 24 months postoperatively. In both groups, there was a statistically significant improvement in all the domains of the questionnaire between the initial values and 24 months values (p < 0.05). Also, there was no significant difference between the values at 12 and 24 months. There was no significant difference between the two groups when comparing each specific domain. Finally, Table 5 presents the data from the gastrointestinal questionnaire, with significantly fewer complaints for abdominal bloating and stool odors in the LADS group.
Complications
No major complications were observed within 30 days of surgery. However, 2 patients in the control group (BPD/DS) had to consult at the emergency in the days following the procedure for minor complications. One of these two patients was hospitalized for abdominal pain. The results of the investigations were negative, and no specific treatment was initiated. The other patient did not require hospitalization. An anastomotic bleeding was suspected, but no transfusion was needed. During the 2-year follow-up, a total of two patients from the control group developed nephrolithiasis. One patient in the control group also underwent reoperation 2 years after the initial surgery for an internal hernia of the biliopancreatic loop secondary to surgical adhesions. No cases of severe protein malnutrition (albumin level under 25 g/dl) were observed. No cases of rhabdomyolysis were reported.
Discussion
Key Results and Interpretations
In this pilot study, patients were randomly assigned to undergo either standard BPD/DS or the same procedure with a longer strict alimentary limb. The hypothesis behind the research question in this study was that LADS would potentially reduce the side effects associated with standard BPD/DS, while leading to similar weight loss. Thus, the effect of protein kinases and lipase secreted by the stomach combined with an increase in the length of the alimentary limb could improve the absorption of proteins and lipid-soluble vitamins. The common limb fixed at 100 cm would preserve the physiological mechanisms known to reduce lipid absorption after BPD/DS. This study is the first randomized control trials that compared the effect of a longer alimentary limb in BPD/DS with standard BPD/DS at 2 years. Other studies have looked at the effect of modifying the standard procedure. A study by Hamoui et al. [10] showed, for patients with BMI ≥ 60 kg/m2, that a biliopancreatic limb length of 45% of the total small bowel length minimally affects the long-term weight loss. Their study group had significantly lower hemoglobin, calcium, and potassium levels. McConnell et al. [11] studied the effect of a shorter (80–90 cm) versus a longer common channel (150 cm) on weight loss. This study showed a significantly lower %EWL in the group with a longer common channel. In 2016, our group published a retrospective study in which we concluded that a 200-cm common channel, compared with a 100-cm common channel, allows similar weight loss and remission rate of comorbidities. However, a higher weight regain was observed in the study group. Although not statistically significant, the 200-cm common channel group had a lower incidence of severe protein deficiency and hyperparathyroidism and required smaller amounts of vitamins A and D. We have witnessed a trend to increase the common channel length and bring it as an omega loop, with the increasing number of one-anastomosis duodenal switch (OADS). In a match cohort study published in 2017, Cottam et al. [12] compared the stomach intestinal pylorus sparing surgery (SIPS, with a 300-cm common channel length) with the standard BPD/DS. At 2 years, there was no significant difference in terms of weight loss and remission of T2D between SIPS and BPD/DS. In addition, nutritional parameters after surgery were not significantly different between the two groups. Another retrospective cohort study by Surve et al. [13] also compared the outcomes between BPD/DS and SIPS at 2 years. SIPS had significantly less perioperative and postoperative complications, shorter operative and hospitalization time, and similar nutritional results at 2 years, compared with BPD/DS. However, weight loss was greater in the BPD/DS group. Another modification of the standard BPD/DS described by Sanchez-Pernaute et al. [14] is the single-anastomosis duodeno-ileal switch (SADIS), in which the common channel is set at 250 cm. It is a simplified procedure with the advantage of reducing the operative time. Many studies have confirmed a similar short-term effectiveness of OADS for weight loss and resolution of obesity-related comorbidities when compared with BPD/DS [15,16,17,18,19]. However, long-term data and randomized control trials are still needed to evaluate the efficiency and safety of this procedure.
This study confirms the 2-year effectiveness of LADS, even though weight loss results were lower compared with BPD/DS. As mentioned in the first part of the study, the weight loss for both groups is not only significant but also particularly high. Indeed, all patients reached an EWL% > 50%, which is typically described as successful. It should be noted that, in both groups, mean preoperative BMI was lower than usually expected for patients having an indication of BPD/DS. This is explained by the fact that BPD/DS has been the main surgery offered to eligible patients at our center for a long time, regardless of the BMI, because of different beliefs about the role of BPD/DS in obese patients. Regarding the status of obesity-related comorbidities, no significant difference was noted between the two groups studied, even though the absolute number of comorbidities was small. The LADS procedure was associated with a significantly longer operating time. This difference can be explained by the fact that surgeons at our center have long-standing experience with standard BPD/DS, which makes them very efficient with this technique. Also, the operating time in this study is greatly prolonged compared with the normal operating time of the procedure since the study required to measure the entire length of the small intestine. There was no difference between the two groups in terms of nutritional deficiencies, but the mean levels of calcium, vitamin D, hemoglobin, zinc, and copper at 24 months were significantly higher in the LADS group. Indeed, one would expect that procedures associated with better weight loss would also yield a higher rate of vitamin and element deficiencies. However, the number of vitamins and supplements was similar between the two groups. There were also fewer gastrointestinal side effects (bloating and annoyance with stool odors) after LADS, although quality of life was not statistically different between the two groups. However, both groups reported a significant increase in their quality of life following surgery.
Strength and Limitations
Since this study is a randomized-controlled study, potential confounding biases are limited. However, the small sample size provides a weak statistical power to this study and does not differentiate the two procedures for outcomes that rarely occur (e.g., complications). The study was carried out from an exploratory perspective, hence the small sample size. In addition, it is important to try to explain the exceptional results of the BPD/DS group. A bias of volunteering could explain these results. Randomization should balance this bias while ensuring that the difference between the two groups truly exists. Finally, the short duration of the follow-up makes it impossible to evaluate the long-term results of this surgery, especially for vitamin deficiencies.
Conclusions
At 2 years, LADS surgery led to a significantly lower weight loss when compared with traditional BPD/DS. There was no difference between the two surgeries for complications and quality of life after surgery. Given the superiority of BPD/DS over LADS in terms of weight loss for a similar side-effect profile, the study was discontinued after 24 months as planned by the initial research protocol. As the results were clearly in favor of the BPD/DS, the authors did not see the relevance of performing a randomized controlled study with sample size calculation on this subject. The LADS surgical technique was discontinued following this study.
Abbreviations
- LADS:
-
Long alimentary limb duodenal switch
- BPD/DS:
-
Biliopancreatic diversion with duodenal switch
- BMI:
-
Body mass index
- EWL:
-
Excess weight loss
- EWL%:
-
Percentage of excess weight loss
- NIH:
-
National Institutes of Health
- SG:
-
Sleeve gastrectomy
- CPAP:
-
Continuous positive airway pressure
- HDL:
-
High-density lipoprotein
- TWL%:
-
Percentage of total weight loss
- SIPS:
-
Stomach intestinal pylorus sparing surgery
- OADS:
-
One-anastomosis duodenal switch
- kg/m2 :
-
Kilogram per meter squared
- kg:
-
Kilogram
- %:
-
Percentage
- N:
-
Number
- CVD:
-
Cardiovascular disease
- T2D:
-
Type 2 diabetes
- COPD:
-
Chronic obstructive pulmonary disease
- HTN:
-
Arterial hypertension
- g/L:
-
Gram per liter
- mM:
-
Millimole
- ng/L:
-
Nanogram per liter
- μM:
-
Micromole
- μg/L:
-
Microgram per liter
- mg:
-
Milligram
- IU:
-
International unit
References
Obesity in Canada - a joint report from the Public Health Agency of Canada and the Canadian Institute for Health Information. 2011.
Gastrointestinal surgery for severe obesity: National Institutes of Health Consensus Development Conference Statement. Am J Clin Nutr 1992;55(2 Suppl):615S–9S. https://doi.org/10.1093/ajcn/55.2.615s.
Marceau P, Biron S, Fau-Hould F-S, et al. Duodenal switch: long-term results. Obes Surg. 2007;17(11):1421–30.
Anderson B, Gill RS, de Gara CJ, et al. Biliopancreatic diversion: the effectiveness of duodenal switch and its limitations. Gastroenterol Res Pract. 2013;2013:974762. https://doi.org/10.1155/2013/974762.
Homan J, Betzel B, Fau-Aarts EO, et al. Vitamin and mineral deficiencies after biliopancreatic diversion and biliopancreatic diversion with duodenal switch—the rule rather than the exception. Obes Surg. 2015;25(9):1626–32.
Cloutier A, Lebel S, Hould F, et al. Long alimentary limb duodenal switch (LADS): a short-term prospective randomized trial. Surg Obes Relat Dis. 2018;14(1):30–7.
Therrien F, Marceau P, Turgeon N, et al. The Laval questionnaire: a new instrument to measure quality of life in morbid obesity. Health Qual Life Outcomes. 2011;9:66.
Biertho L, Lebel S, Marceau S, et al. Biliopancreatic diversion with duodenal switch: surgical technique and perioperative care. Surg Clin North Am. 2016;96(4):815–26.
Brethauer SA, Kim J, el Chaar M, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Obes Surg. 2015;25(4):587–606.
Hamoui N, Anthone Gj Fau-Kaufman HS, Kaufman Hs Fau-Crookes PF, et al. Maintenance of weight loss in patients with body mass index >60 kg/m2: importance of length of small bowel bypassed. Surg Obes Relat Dis. 2008;4(3):404–6.
McConnell DB, O’Rourke Rw Fau- Deveney CW, Deveney CW. Common channel length predicts outcomes of biliopancreatic diversion alone and with the duodenal switch surgery. Am J Surg 2005;189(5):536–540.
Cottam A, Cottam D, Portenier D, et al. A matched cohort analysis of stomach intestinal pylorus saving (SIPS) surgery versus biliopancreatic diversion with duodenal switch with two-year follow-up. Obes Surg. 2017;27(2):454–61.
Surve A, Zaveri H, Cottam D, et al. A retrospective comparison of biliopancreatic diversion with duodenal switch with single anastomosis duodenal switch (SIPS-stomach intestinal pylorus sparing surgery) at a single institution with two year follow-up. Surg Obes Relat Dis. 2017;13(3):415–22.
Sanchez-Pernaute A, Rubio MA, Conde M, et al. Single-anastomosis duodenoileal bypass as a second step after sleeve gastrectomy. Surg Obes Relat Dis. 2015;11(2):351–5.
Shoar S, Poliakin L, Rubenstein R, et al. Single anastomosis duodeno-Ileal switch (SADIS): a systematic review of efficacy and safety. Obes Surg. 2018;28(1):104–13.
Moon RC, Gaskins L, Teixeira AF, et al. Safety and effectiveness of single-anastomosis duodenal switch procedure: 2-year result from a single US institution. Obes Surg. 2018;28(6):1571–7.
Brown WA, Ooi G, Higa K, et al. IFSO-appointed task force reviewing the literature on SADI-S/OADS. Single anastomosis duodenal-Ileal bypass with sleeve gastrectomy/one anastomosis duodenal switch (SADI-S/OADS) IFSO position statement. Obes Surg. 2018;28(5):1207–16.
Moon RC, Kirkpatrick V, Gaskins L, et al. Safety and effectiveness of single- versus double-anastomosis duodenal switch at a single institution. Surg Obes Relat Dis févr. 2019;15(2):245–52.
Finno P, Osorio J, García-Ruiz-de-Gordejuela A, et al. Single versus double-anastomosis duodenal switch: single-site comparative cohort study in 440 consecutive patients. Obes Surg. 2020;30(9):3309–16.
Acknowledgments
The authors thank IUCPQ’s foundation for their support to this work.
Funding
Research grant from the Fondation de l’Institut universitaire de cardiologie et pneumologie de Quebec, Université Laval
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethics Declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Malo, FC., Marion, A., Rioux, A. et al. Long Alimentary Limb Duodenal Switch (LADS): an Exploratory Randomized Trial, Results at 2 Years. OBES SURG 30, 5047–5058 (2020). https://doi.org/10.1007/s11695-020-04968-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04968-5