Abstract
Introduction
Biliopancreatic diversion with duodenal switch (BPD-DS) has often been reserved for patients with BMI > 50 kg/m2. We aim to assess the safety of BPD-DS in patients with morbid obesity (BMI 335 kg/m2 and < 50 kg/m2) using a 150-cm common channel (CC), 150-cm Roux limb, and 60-fr bougie.
Methods
A retrospective review was performed on patients with a BMI < 50 mg/k2 who underwent a BPD-DS in 2016–2019 at a single institution. Limb lengths were measured with a laparoscopic instrument with minimal tension. Sleeve gastrectomy was created with 60-fr bougie. Variables were compared using paired t test, Chi-square analysis or repeated measures ANOVA where appropriate.
Results
Forty-five patients underwent BPD-DS. CC lengths and Roux limb lengths were 158 ± 20 cm and 154 ± 18 cm, respectively. Preoperative BMI was 44.9 ± 2.3 kg/m2 and follow-up was 2.7 ± 1.4 years. One patient required reoperation for bleeding and died from multiorgan failure and delayed sleeve leak. There was 1 (2.2%) readmission for contained anastomotic leak and 2 ED visits (4.5%) within 30 days. There were no marginal ulcers, limb length revisions, or need for parental nutrition. Percent excess weight loss was 67.2 ± 19.7%. 88.9% (N = 8), 86.6% (N = 13), and 55.5% (N = 5) of patients had resolution or improvement of their diabetes mellitus type II, hypertension, and hyperlipidemia, respectively. 40% (N = 4) of patients had resolution of their gastroesophageal reflux disease (GERD) and 11.4% (N = 5) developed de novo GERD. 32% (N = 14) of patients had vitamin D deficiency and 25% (N = 11) experienced zinc deficiency.
Conclusion
BPD-DS may be considered in patients with BMI < 50 kg/m2 with 150-cm CC, 150-cm Roux limb, and a 60-fr bougie sleeve gastrectomy. There was sustained weight loss and no protein calorie malnutrition, but Vitamin D and zinc deficiency remained a challenge. Careful patient selection and proper counseling of the risks and benefits are necessary.
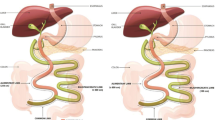
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Biliopancreatic diversion/duodenal switch (BPD-DS) is considered the most effective for sustained weight loss and comorbidity resolution [1, 2]. BPD-DS, however, represents only 0.6% of the bariatric surgeries performed annually in the USA [3]. Due to concerns over nutritional deficiencies and a reversal rate ranging from 0.5% to 4.9% [4, 5], most surgeons are offering BPD-DS primarily in patients with BMI ≥ 50 kg/m2 [2, 6, 7].
The BPD-DS provides several benefits over other bariatric procedures, including greater weight loss, higher rates of diabetes mellitus type II (DMII) resolution, and lower marginal ulcers [1, 2, 8]. The BPD-DS technique also varies with common channel (CC) lengths ranging between 50 and 100 cm, Roux limb lengths 150–200 cm, and sleeve gastrectomies made with 34–60-fr bougies. Studies on BPD-DS with a 100-cm CC and 150 Roux limb have reported rates of severe malnutrition ranging between 4 and 14%, while a CC of 200 cm resulted in more weight regain [9,10,11]. Only 1 study with long-term follow-up investigated BPD-DS in patients with BMI < 50 kg/m2 with a 100-cm CC and 250-cm Roux limb and reported a 1.5% rate of revision [12]. We thus aim to assess whether BPD-DS with a longer CC of 150 cm, Roux limb length of 150 cm, and a larger sleeve gastrectomy with a 60-fr bougie can be performed in patients with BMI < 50 kg/m2 safely without a significant risk of protein calorie malnutrition.
Methods
After IRB approval, a retrospective review was performed of consecutive adult patients with BMI < 50 who underwent BPD-DS at a single institution between January 2016 and December 2019. Only patients who were eligible for at least 1-year follow-up were included. All patients were preoperatively evaluated by the surgeon, dietician, and psychologist to assess surgical candidacy. Postoperative follow-up occurred at 1 week, 1 month, 3 months, 6 months, 1 year, and annually thereafter. Comorbidities including DMII, hypertension (HTN), hyperlipidemia (HLD), obstructive sleep apnea (OSA), and gastroesophageal reflux disease (GERD) were defined as requiring prescription medication or treatment to manage the disease. Nutritional outcomes were documented, and abnormal values were reported.
Operative technique
All operations were performed laparoscopically by a single surgeon without the help of trainees. The sleeve gastrectomy was created over a 60-fr bougie starting at 5 cm from the pylorus. The small bowel was measured with minimal stretch using a laparoscopic instrument marked at 10 cm. Both common channel and Roux limb were measured similarly. The duodeno-ileostomy anastomosis and the ileo-ileostomy were created using linear stapler with the common enterotomy sewn closed.
Statistical analysis
Data are presented as mean ± standard deviation for continuous variables and percentages for categorical variables. Variables were compared using paired t test, Chi-square analysis, or repeated measures ANOVA where appropriate.
Results
Baseline characteristics
There were 45 patients with morbid obesity who underwent BPD-DS with average follow-up was 2.7 ± 1.4 years (Fig. 1). This group consisted of 40% of the BPD-DS that were performed in this period. CC lengths and Roux limb lengths were 158 ± 20 cm and 154 ± 18 cm, respectively. Average age was 40 ± 10 years, 87% were female, and average preoperative BMI was 44.9 ± 2.3 kg/m2 (Table 1).
30-day outcomes
There was 1 patient who required early reoperation for bleeding and died from multiorgan failure and delayed sleeve leak. Excluding this patient who had prolonged hospital stay, the average length of stay was 2.14 ± 0.68 days. In the remaining patients, there were 2 (4.5%) ED visits for nausea and dehydration and 1 (2.2%) readmission for a contained anastomotic leak within 30 days of surgery that resolved with antibiotics and bowel rest. There were no marginal ulcers, limb length revisions, or need for parental nutrition for protein calorie malnutrition during the duration of follow-up.
Weight loss and comorbidity resolution
Average percent excess weight loss (%EWL) was 67.2 ± 19.7, percent total weight loss (%TWL) was 29.4 ± 8.7, and BMI change was 16.2 ± 7.9 (Graph 1). Postoperative weight at 1 year was significantly lower than preoperative weight (p < 0.0001) without significant increase out to 5 years. Of the 9 patients who had preoperative DMII, 6 (66.7%) patients had resolution, 2 (22.2%) had improvement, and 1 (11%) had no change in DMII medications (Fig. 2). Of the 15 patients who had preoperative hypertension (HTN), 8 (53.3%) had resolution, 5 (33.3%) had improvement, 1 (6.7%) had no change, and 1 (6.7%) was lost to follow-up. Of the 9 patient who had HLD, 4 (44.4%) had resolution, 1 (11.1%) had improvement, 3 (33.3%) had no change, and 1 (11.1%) was lost to follow-up. Of the 10 patients who had preoperative GERD, 4 (40.0%) had resolution, 6 (60.0%) had no change, and 5 (11.4%) patients had de novo GERD. One patient had Barrett’s esophagus without dysplagia progressed to high-grade dysplasia at 5 years. Of the 6 patients who had preoperative OSA, 4 (66.6%) had resolution and the remainder had no change in their OSA.
Nutritional outcomes
Baseline nutritional labs are listed in Table 2. Patients with abnormal levels are listed out of the total number of patients who had values reported. One patient had anemia and one patient had low albumin at baseline. Nineteen (65.5%) patients had low vitamin D at baseline. Overall, no patient experienced hypoalbuminemia and 3 (7%) patients developed new anemia. The most common vitamin deficiency was vitamin D deficiency that affected 14 (32%) patients, 9 (64%) of which had vitamin D deficiency at baseline and the remainder were missing baseline values. The second most common deficiency was zinc deficiency that affected 11 (25%) patients.
Discussion
Many surgeons reserve the BPD-DS to patients with BMI ≥ 50 kg/m2 [2, 6, 7] with only one study by Biertho et al. reporting BPD-DS specifically in patients with a BMI < 50 kg/m2 [12]. We found in patients with morbid obesity (BMI 35–50 kg/m2), BPD-DS with an average CC of 150 cm, a 150-cm Roux limb, and a sleeve gastrectomy created with a 60-fr bougie resulted in significant and sustained weight loss, comorbidity resolution, and no protein calorie malnutrition. Vitamin D and zinc deficiencies, however, remained a challenge.
Patients in this study experienced an average %EWL of 67.2 ± 19.7% that was sustained out to 5 years. These results are consistent with other studies that have reported a %EWL between 65 and 70% [9, 10]. Overall, there was resolution or improvement of 88.9% DMII, 86.7% HTN, 55.6% HLD, 40% GERD, and 66.6% OSA. Other studies have reported similar rates of comorbidity resolution [10, 13]. De novo GERD following BPD-DS, however, has been less well documented. Badaoui et al. studied effect of BPD-DS on GERD and reported an 18.4% rate of de novo GERD [14]. We experienced an 11.4% rate of de novo GERD with 1 patient progressing from Barrett’s esophagus without dysplasia to high-grade dysplasia at 5 years. Rates of de novo Barrett’s esophagus after sleeve gastrectomy are between 2 and 8% [15, 16] with several case reports reporting progression to cancer [17,18,19]. Rates of Barrett’s esophagus or de novo GERD in BPD-DS when a larger bougie size are often used to greet the sleeve gastrectomy is currently unknown.
There are few studies that have investigated BPD-DS in patients with BMI < 50 kg/m2. In this study, 1 (2.2%) patient had a major complication requiring reoperation and died from multiorgan failure and delayed sleeve leak. There were 2 (4.5%) ED visits for nausea and dehydration and 1 (2.2%) readmission for a contained anastomotic leak 3 weeks after surgery. Biertho et al. studied open BPD-DS in patients with BMI < 50 kg/m2 and reported a major perioperative complication rate of 5.8% and a mortality rate of 0.6% [12]. Rezvani et al. compared laparoscopic BPD-DS in BMI < 50 kg/m2 to those with BMI > 50 kg/m2 and reported no mortalities and a perioperative complication rate of 11% without significant differences between groups rate [6]. Our mortality rate is higher than what has been reported likely due to a smaller sample size.
One of the well-documented risks of BPD-DS is protein calorie malnutrition and vitamin deficiencies. Few studies have investigated the relationship between limb lengths and malnutrition in BPD-DS. For BPD-DS with 100-cm CC and 150-cm Roux limbs, reports of severe malnutrition requiring parental nutrition or revision are between 4 and 14% [9, 10, 20]. Biertho et al. studied BPD-DS in patients with BMI < 50 kg/m2 with a 100-cm CC and 250-cm Roux limb and had a 1.5% rate of revision along with difficulty supplementing fat-soluble vitamins [12]. Lebel et al. demonstrated that by increasing the common channel length to 200 cm, patients experienced fewer nutritional deficiencies at the cost of more weight regain [11]. McConnell et al. compared CC lengths of 150 cm to 100 cm to 80–90 cm and found better weight loss in the 100 cm or less groups at the cost of more vitamin D deficiency [21]. Our average CC length of 150 cm and Roux limb of 150 cm resulted in no protein malnutrition or need for revision. Patients in this cohort did, however, experience vitamin D deficiency, particularly those that had preoperative vitamin D deficiency, and zinc deficiency, which are well-documented nutritional deficiencies with BPD-DS [22,23,24,25].
Lastly, the size of the sleeve gastrectomy may affect rates of early postoperative dehydration and nutrition. Studies investigating the effect of bougie size used to create the sleeve gastrectomy have found that a larger bougie size may decrease rates of dehydration and improved nutritional intake [26, 27]. Additionally, the bougie size in the BPD-DS has not been standardized and ranges from 34 to 60 fr [9, 11, 20]. The low rates of dehydration and protein malnutrition seen in this study may be due to a larger sleeve gastrectomy size as well as the longer CC length. More studies investigating the effect of sleeve gastrectomy vs limb lengths in the BPD-DS is required.
Limitations
There are limitations to this study. First, this study is limited by a small sample size and potential selection bias. Patients who were more likely to adhere to vitamin supplementation who had a significant smoking history or NSAID use may have chosen to undergo BPD-DS. This selection bias may only be mitigated by a randomized clinical trial. Second, available nutrition labs were < 50% after 3 years of follow-up. Additionally, GERD was defined as acid reflux symptoms requiring medication, which is not a specific assessment of true acid reflux. Subsequently, the focus of this paper is not the effect of BPD-DS on GERD. Understanding the relationship between BPD-DS on GERD will require dedicated studies. Lastly, the average follow-up in this study was 2.7 ± 1.4 years and thus, longer follow-up is needed to better understand the impact of BPD-DS on nutritional deficiencies in this population.
Conclusion
BPD-DS may be considered in patients with BMI < 50 kg/m2 when 150-cm CC, 150-cm Roux limb, and a sleeve gastrectomy with 60-fr bougie are used. There was sustained weight loss out to 5 years of follow-up and no protein calorie malnutrition, but vitamin D and zinc deficiency remained a challenge. Careful patient selection and proper counseling of the risks and benefits are necessary.
References
Skogar ML, Sundbom M (2017) Duodenal switch is superior to gastric bypass in patients with super obesity when evaluated with the bariatric analysis and reporting outcome system (BAROS). Obes Surg 27:2308–2316
Risstad H, Sovik TT, Engstrom M et al (2015) Five-year outcomes after laparoscopic gastric bypass and laparoscopic duodenal switch in patients with body mass index of 50 to 60: a randomized clinical trial. JAMA Surg 150:352–361
English WJ, DeMaria EJ, Brethauer SA, Mattar SG, Rosenthal RJ, Morton JM (2018) American society for metabolic and bariatric surgery estimation of metabolic and bariatric procedures performed in the United States in 2016. Surg Obes Relat Dis 14:259–263
Marceau P, Biron S, Hould FS et al (2009) Duodenal switch improved standard biliopancreatic diversion: a retrospective study. Surg Obes Relat Dis 5:43–47
Topart PA, Becouarn G (2015) Revision and reversal after biliopancreatic diversion for excessive side effects or ineffective weight loss: a review of the current literature on indications and procedures. Surg Obes Relat Dis 11:965–972
Rezvani M, Sucandy I, Klar A, Bonanni F, Antanavicius G (2014) Is laparoscopic single-stage biliopancreatic diversion with duodenal switch safe in super morbidly obese patients? Surg Obes Relat Dis 10:427–430
Merz AE, Blackstone RB, Gagner M et al (2019) Duodenal switch in revisional bariatric surgery: conclusions from an expert consensus panel. Surg Obes Relat Dis 15:894–899
Nelson DW, Blair KS, Martin MJ (2012) Analysis of obesity-related outcomes and bariatric failure rates with the duodenal switch vs gastric bypass for morbid obesity. Arch Surg 147:847–854
Topart P, Becouarn G, Delarue J (2017) Weight loss and nutritional outcomes 10 years after biliopancreatic diversion with duodenal switch. Obes Surg 27:1645–1650
Sethi M, Chau E, Youn A, Jiang Y, Fielding G, Ren-Fielding C (2016) Long-term outcomes after biliopancreatic diversion with and without duodenal switch: 2-, 5-, and 10-year data. Surg Obes Relat Dis 12:1697–1705
Lebel S, Dion G, Marceau S, Biron S, Robert M, Biertho L (2016) Clinical outcomes of duodenal switch with a 200-cm common channel: a matched, controlled trial. Surg Obes Relat Dis 12:1014–1020
Biertho L, Biron S, Hould FS, Lebel S, Marceau S, Marceau P (2010) Is biliopancreatic diversion with duodenal switch indicated for patients with body mass index <50 kg/m2? Surg Obes Relat Dis 6:508–514
Hedberg J, Sundstrom J, Sundbom M (2014) Duodenal switch versus Roux-en-Y gastric bypass for morbid obesity: systematic review and meta-analysis of weight results, diabetes resolution and early complications in single-centre comparisons. Obes Rev 15:555–563
Badaoui JN, Kellogg TA, Abu Dayyeh BK et al (2021) The outcomes of laparoscopic biliopancreatic diversion with duodenal switch on gastro-esophageal reflux disease: the mayo clinic experience. Obes Surg 31:4363–4370
Yeung KTD, Penney N, Ashrafian L, Darzi A, Ashrafian H (2020) Does sleeve gastrectomy expose the distal esophagus to severe reflux? A systematic review and meta-analysis. Ann Surg 271:257–265
Al Sabah S, AlWazzan A, AlGhanim K, AlAbdulrazzaq HA, Al HE (2021) Does laparoscopic sleeve gastrectomy lead to Barrett’s esophagus, 5-year esophagogastroduodenoscopy findings: a retrospective cohort study. Ann Med Surg (Lond) 62:446–449
El Khoury L, Benvenga R, Romero R, Cohen R, Roussel J, Catheline JM (2018) Esophageal adenocarcinoma in Barrett’s esophagus after sleeve gastrectomy: case report and literature review. Int J Surg Case Rep 52:132–136
Wright FG, Duro A, Medici JR, Lenzi S, Beskow AF, Cavadas D (2017) Esophageal adenocarcinoma five years after laparoscopic sleeve gastrectomy: a case report. Int J Surg Case Rep 32:47–50
Chen W, Wang Y, Zhu J, Wang C, Dong Z (2021) Esophagogastric cancer after sleeve gastrectomy: a systematic review of case reports. Cancer Manag Res 13:3327–3334
Strain GW, Torghabeh MH, Gagner M et al (2017) The impact of biliopancreatic diversion with duodenal switch (BPD/DS) over 9 years. Obes Surg 27:787–794
McConnell DB, O’Rourke RW, Deveney CW (2005) Common channel length predicts outcomes of biliopancreatic diversion alone and with the duodenal switch surgery. Am J Surg 189:536–540 (Discussion 40)
Salle A, Demarsy D, Poirier AL et al (2010) Zinc deficiency: a frequent and underestimated complication after bariatric surgery. Obes Surg 20:1660–1670
Homan J, Schijns W, Aarts EO, Janssen IMC, Berends FJ, de Boer H (2018) Treatment of vitamin and mineral deficiencies after biliopancreatic diversion with or without duodenal switch: a major challenge. Obes Surg 28:234–241
Topart P, Becouarn G, Salle A, Ritz P (2014) Biliopancreatic diversion requires multiple vitamin and micronutrient adjustments within 2 years of surgery. Surg Obes Relat Dis 10:936–941
Slater GH, Ren CJ, Siegel N et al (2004) Serum fat-soluble vitamin deficiency and abnormal calcium metabolism after malabsorptive bariatric surgery. J Gastrointest Surg 8:48–55 (Discussion 4–5)
Hawasli A, Jacquish B, Almahmeed T et al (2015) Early effects of bougie size on sleeve gastrectomy outcome. Am J Surg 209:473–477
Chang PC, Chen KH, Jhou HJ et al (2021) Promising effects of 33 to 36 Fr bougie calibration for laparoscopic sleeve gastrectomy: a systematic review and network meta-analysis. Sci Rep 11:15217
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Abdelrahman Nimeri received travel honorarium from Intuitive; Keith S. Gersin is a consultant in GI Dynamics; WL Gore is the honoraria speaker and received ownership interest from Standard Bariatrics. Alice Wang, Michael Genz, Jim Feimster, Kyle Thompson, Alexander Abdurakhmanov, Vilok Vijayanagar, Iain McKillop, Selwan Barbat, Timothy Kuwada, and Roc Bauman have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, A., Nimeri, A., Genz, M. et al. Safety of biliopancreatic diversion with duodenal switch in patients with body mass index less than 50 kg/m2. Surg Endosc 37, 3046–3052 (2023). https://doi.org/10.1007/s00464-022-09483-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09483-5