Abstract
Backgrounds
Optimal pain management in bariatric patients is crucial for early recovery. This study aims to evaluate the effects of magnesium and ketamine combination on morphine consumption after open bariatric surgery (primary outcome), as well as on postoperative pain scores and occurrence of side effects.
Method
A total of 60 patients undergoing elective open gastric bypass were randomized into 3 groups. All patients received the same general anaesthesia protocol. The magnesium and ketamine group (Mg + K) received an IV bolus of magnesium 50 mg/kg and ketamine 0.2 mg/kg followed by continuous infusion of magnesium (8 mg/kg/h) and ketamine (0.15 mg/kg/h) until extubation. The ketamine group (K) received the same bolus and infusion of ketamine, together with a bolus and continuous infusion of normal saline. The placebo group (P) received normal saline. All patients received 48 h of paracetamol 1 g IV q6h and morphine sulphate 0.1 mg/kg subcutaneous q6h PRN. Morphine consumption, VAS pain scores and occurrence of side effects were recorded for 48 h postoperatively.
Results
Patients in group (Mg + K) (2.4 ± 2.62 mg) and in group (K) (2.8 ± 2.66 mg) had significantly lower morphine consumption in the PACU compared with the patients in group (P) (4.85 ± 4.51 mg) (p = 0.045). Patients in group (Mg + K) consumed significantly less morphine the first 24 postoperative hours, with a relative reduction of 87% and 21% compared with group (K) and group (P) respectively (p = 0.028). However, this difference was not observed at 48 h. No significant difference was shown between the three groups in terms of nausea and vomiting, time to extubation or excessive sedation.
Conclusion
The association of magnesium and ketamine bolus followed by infusion in open bariatric surgery appears to be safe and decreases morphine requirements in the first 24 h compared with both ketamine alone and placebo.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The rise in the prevalence of obesity is accompanied by increases in bariatric surgeries that have demonstrated their effectiveness in achieving weight loss and reducing obesity-related comorbidities [1]. However, bariatric surgeries are not devoid of risks, and they present significant challenges to general anaesthesia. Obesity is a risk factor for perioperative cardiovascular, thromboembolic, gastrointestinal and respiratory complications [2]. Optimal management of postoperative pain in bariatric patients is therefore crucial, as it allows better respiration and early ambulation, and thus, improves procedural morbidity. Remifentanil with its strong potency and short duration of action is particularly interesting in bariatric surgery. It achieves adequate level of analgesia without increasing the risk of postoperative respiratory depression or delayed awakening compared with longer acting opioid such as fentanyl or sufentanil [3]. Moreover, obesity has no impact on its pharmacokinetics [4]. However, a major downside of remifentanil is its known potential to develop hyperalgesia and acute opioid tolerance, manifested by an increase in postoperative analgesics requirements [5,6,7,8]. Non-opioid analgesics acting on central excitability appear beneficial in counteracting hyperalgesia. This category includes N-methyl-D-aspartate (NMDA) receptor antagonists, such as ketamine and magnesium (Mg), which retain the greatest potential for inhibition of hyperalgesia by the central nervous system [9, 10].
Clinically, it is widely accepted that subanaesthetic doses of ketamine decrease opioid consumption following abdominal, orthopaedic, gynaecologic and cardiac surgery [11,12,13,14,15].
Furthermore, magnesium exerts its anti-nociceptive effects via a non-competitive NMDA receptor antagonist effect and by inhibiting the intracellular influx of calcium [16, 17]. In 1996, Tramer et al. conducted the first clinical trial showing less postoperative analgesic requirements associated with the perioperative administration of magnesium sulphate [18]. Multiple subsequent studies, based on this dual antagonism, demonstrated the postoperative opioid-sparing effect of systemic magnesium in cardiac, abdominal, gynaecologic and orthopaedic surgery [19,20,21,22].
Since ketamine and magnesium act on different sites of the NMDA receptor, it was postulated that the combination of both drugs may lead to a more effective analgesia with lower doses of each agent. An additive effect of the combination of magnesium and ketamine with less side effects was demonstrated in experimental and clinical trials [23, 24]. Literature involving ketamine and magnesium in bariatric surgical patients is very sparse. To our knowledge, no studies to date have focused on the synergistic effects of their coadministration in bariatric surgery. The purpose of this study was to evaluate the effects of magnesium and ketamine combination on opioid consumption during and after bariatric surgery (primary outcome), as well as its effect on postoperative pain scores.
Materials and Methods
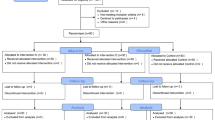
A prospective randomized double-blind study was conducted between March 2015 and April 2016 at Hotel-Dieu de France University hospital to test the hypothesis that ketamine and magnesium association contributes to an intraoperative and postoperative morphine-sparing effect, while providing adequate analgesia. After approval from the Ethical Review Committee of Saint Joseph University, 87 patients with morbid obesity, aged between 18 and 60 years and undergoing open One Anastomosis Gastric Bypass surgery (OAGB) were assessed for eligibility, and were included in the study. The exclusion criteria were patient refusal, allergy to ketamine, magnesium or morphine, chronic kidney disease (creatinine > 150 μmol/l), any neurological disorder, myopathy, cardiac dysfunction (ejection fraction < 40%), uncontrolled hypertension, documented psychiatric history, preoperative opioid use, recent magnesium intake, history of chronic pain and alcohol or opiates addiction.
Randomisation
Patients were randomized, into 3 groups of 20 patients each, using a computer-generated table by the hospital pharmacists: magnesium and ketamine group (group Mg + K), ketamine group (group K) and placebo group (group P). These same pharmacists prepared the study solutions. Care was taken to insure the same volume for all preparations. Investigators, patients and all clinical staff were unaware of the treatment group.
Treatment
All drugs were administered according to the theoretical ideal weight (TIW) except for suxamethonium, which was administered according to the real body weight. TIW was calculated by using the formula: TIW = 22 × (height)2 (height in meter) [25].
All patients were pre-medicated 1 h before surgery with oral hydroxyzine 1 mg/kg.
Monitoring included the following: electrocardiogram, pulse oximetry, blood pressure (invasive or non-invasive), gas analyser (EtCO2, sevoflurane), rectal temperature, train-of-four (TOF) at the adductor pollicis and Bispectral Index (BIS).
All patients received the same standardized general anaesthesia protocol. At induction propofol 3 mg/kg, bolus of remifentanil 0.5 μg/kg over 1 min and suxamethonium 1 mg/kg were administered intravenously. Maintenance of anaesthesia was achieved with a continuous intravenous (IV) infusion of remifentanil 0.05 to 0.25 μg/kg/min and sevoflurane in a gas mixture nitrous oxide/oxygen (0.6). BIS goals varied between 40 and 60 and mean arterial pressure between 60 and 80 mmHg. Rocuronium or cisatracurium was titrated as soon as one twitch was recorded on the train of four (TOF), and/or on surgeon demand when a post-tetanic count was above 15 (PTC > 15).
Patients in group (Mg + K) received after induction IV ketamine (racemic mixture) bolus of 0.2 mg/kg followed by a continuous infusion of 0.15 mg kg−1 h−1 until tracheal extubation, as well as an IV bolus of magnesium sulphate (50 mg kg−1 in 30 min) followed by a continuous infusion of magnesium at a rate of 8 mg/kg/h until tracheal extubation. Patients in group (K) received the same doses of ketamine (bolus and IV infusion) as well as a bolus and a continuous infusion of normal saline (placebo). Patients in group (P) received after induction two boluses and two continuous infusions of normal saline.
Forty minutes before the end of surgery, all patient received 0.1 mg/kg of morphine sulphate IV and 1 g of paracetamol. Remifentanil infusion was stopped at skin closure. Extubation was done as soon as T4/T1 > 90% after neuromuscular blockade reversal. After surgery, the patients were admitted to the post anaesthesia care unit (PACU) where they spent an average of 3 h. Intravenous morphine was titrated as needed according to the PACU’s protocol by a nurse that was unaware of the treatment group assignments. On the surgical ward, all patients received until 48 h postoperatively paracetamol 1 g IV q6 regularly and morphine sulphate 0.1 mg/kg subcutaneous q6 PRN to achieve a visual analogue scale (VAS) score less than 4.
Data Collection
The following variables were recorded: age, sex, weight, body mass index (BMI), operative time (time from incision to skin closure), time to endotracheal extubation (from discontinuation of sevoflurane to the extubation), total doses of remifentanil, rocuronium and cisatracurium and morphine received before extubation. In the PACU at 1 h (H1), 2 h (H2) and 3 h (H3), morphine titration doses, VAS at rest, with movement and cough, sedation scores (0 = fully awake, 1 = responds to verbal stimulation, 2 = responds to tactile stimulation, 3 = responds to painful stimuli) were also recorded. On the floor total morphine consumption at 24 h and 48 h postoperatively, morphine side effects (nausea, vomiting, pruritus and sedation), ketamine side effects (hallucinations, agitation) and magnesium side effects (hypotension, dysrhythmias) were also recorded.
Statistical Analysis
Statistical analysis was performed using the SPSS v21 software (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.). When required, analysis of variance was performed using Fisher test. Variables were tested for normality using Kolmogorov-Smirnov test when needed. Continuous normally distributed data are reported as mean ± standard deviation, and were compared by one-way analysis of variance (ANOVA) between the 3 groups. The Chi-square test was used for differences in proportions and Mann-Whitney U test for ordinal variables. A two-sided p < 0.05 was considered statistically significant.
Results
A total of 60 patients who met the inclusion criteria completed the study, with 20 patients in each group. Patients’ demographic and surgical characteristics are summarized in Table 1 and were comparable between the three groups.
Concerning morphine titration, patients in the group (Mg + K) and in the group (K) had significantly lower morphine consumption in the PACU compared with patients in the group (P). This difference was noted from H2 (Table 2).
Patients in the group (Mg + K) consumed significantly less morphine in the first 24 postoperative hours, with a relative reduction of 87% and 21% compared with group (K) and group (P) respectively. However, this difference was not observed at 48 H (Table 3). No difference was noted concerning the number of patients that received morphine in the first 24 h between the three groups (Group (Mg + K) (15); Group (K) (17); Group (P) (16)).
The remifentanil consumption tended to be lower in Group (Mg + K) (1834 μg ± 640 for group (Mg + K) versus 2131 μg ± 587 for group (K) and 2146 μg ± 502 for group (P)), but the difference was not statistically significant. The total dose of rocuronium and cisatracurium was similar in both groups (Table 4).
Concerning pain scores, only at H3 in the PACU patients in Group (K) experienced a higher VAS at rest (p = 0.049), with movement (p = 0.048) and cough (p = 0.043) compared with the other two groups (Fig. 1).
Regarding the occurrence of side effects related to analgesia, no significant difference was demonstrated between the three groups in terms of nausea and vomiting. No significant difference appeared in terms of time to extubation and sedation scores. There were no cardiovascular, respiratory or neurological side effects reported in the three groups.
Discussion
Bariatric surgery exposes patients to the following paradox: the more severe the obesity, the greater the expected beneficial results, but also the greater the associated perioperative complications. Since obese patients are more prone to perioperative pulmonary, cardiovascular and thromboembolic complications [2], effective analgesia is crucial for early recovery and ambulation, and thus improving procedural morbidity. However, opioid administration consequences are neither scarce nor benign for the patient. From this perspective, the Canadian consensus statement strongly recommends a reduced opioid use as part of a multimodal approach for enhanced recovery after surgery (ERAS) in bariatric surgery, as decreased opioids usage helps shortening patient recovery time and the duration of stay in hospital [26].
Most of the trials on opioid-free anaesthesia (OFA) have studied the analgesic and morphine-sparing effects of ketamine and magnesium when used alone [20, 21]. The synergistic effects of the two drugs were mostly described in animal models [23], and some orthopaedic surgeries [19]. But none have evaluated their coadministration in bariatric surgery.
This placebo-controlled double-blind study was designed to assess the effect of magnesium and ketamine on perioperative opioid requirements and pain scores in patients undergoing bariatric surgery. We have shown that the association of magnesium and ketamine reduces early morphine needs after bariatric surgery, when compared with ketamine alone, or to a control (placebo) group. However, it does not reduce intraoperative remifentanil consumption.
It is known that intraoperative remifentanil infusion could lead to the development of acute opioid tolerance, and could increase postoperative pain [5,6,7,8]. The mechanism of this hyperalgesia seems to involve the inactivation of NMDA receptors in the dorsal horn of the spinal cord.
Open OAGB is a painful surgery and it is crucial to achieve effective analgesia in order to improve procedural morbidity and patient outcomes [2]. Although opioids are the analgesics of choice, their use is associated with many side effects, including respiratory depression [27] that could exacerbate postoperative pulmonary complications in the more vulnerable obese patients, nausea and vomiting, sedation, ileus, confusion, hyperalgesia and chronic postoperative pain [28]. The American Society of Anesthesiologists Task Force on acute pain management therefore recommends adopting a multimodal approach for providing optimal analgesia while reducing the doses of different drugs and their related side effects [29]. From this perspective, opioids are usually combined to other analgesics such as paracetamol or non-steroid anti-inflammatory drugs (NSAIDs), and co-analgesic agents such as alpha-2-agonists or anti-NMDA receptors like ketamine or magnesium.
We found that the addition of magnesium to ketamine reduces morphine consumption in obese patients undergoing open bariatric surgery during the first 24 h postoperatively, and reduces the pain scores at rest, with movement and during cough before discharge from the PACU. Pain control was adequate since the average VAS in the three groups was constantly lower than 4/10. Many authors have shown that intraoperative use of low doses of NMDA receptor antagonists decreases morphine consumption during and after various surgeries [11,12,13,14,15, 20,21,22]. Moreover, Liu et al. described the “super-additive effect” of these two antagonists [24]. Nitrous oxide is also an NMDA receptor antagonist. However, its effect on pain intensity at rest or on movement is not clinically relevant [30]. It was also used in the three study groups with the same concentration, and therefore it was not a confounding factor.
In this study, pre-operative anti-nociception was based on remifentanil, knowing that this agent can be precisely titrated to reach the adequate desired effect. Thus, it represents a good model to study the real effects of co-administered analgesics.
The ketamine dose we used (0.2 mg kg−1 followed by continuous infusion of 0.15 mg kg−1 h−1) was chosen based on several previous studies that proved its safety and effectiveness [31]. At these analgesic doses (< 1 mg kg−1), the mind-altering effects of ketamine seem to be absent. Although ketamine is indicated for its opioid-sparing effect in patients with chronic pain or opioid dependency [12], these patients were excluded from this study, since a tendency to high morphine consumption could lead to biased outcomes.
In the present study, we chose the bolus (50 mg kg−1) and continuous (15 mg kg−1 h−1) infusion doses of magnesium sulphate based on previous investigations [20,21,22]. Levaux et al. have demonstrated a beneficial effect on pain relief after administering a single bolus dose of magnesium (50 mg kg−1) in major lumbar orthopaedic surgery [32], but O’Flaherty et al. failed to show any significant efficacy of a single bolus 30 mg kg−1 of magnesium sulphate during anaesthesia induction for tonsillectomy in children [33]. Therefore, using magnesium sulphate bolus injections alone seems to be insufficient, and should probably be complemented with either a continuous infusion or repeated boluses. In the current study, a magnesium bolus was given at induction of anaesthesia, followed by a continuous infusion throughout the surgery.
It should be noted that magnesium toxicity begins at serum concentration of 2.5–5 mmol L−1 [34]. We did not measure serum magnesium concentrations after the surgery, but in another study where the same magnesium sulphate bolus and twice the infusion doses were used, the measured serum magnesium levels were was much lower than the toxic levels [35]. Moreover, the reported doses in all of the above-mentioned studies are well below those administered usually during preeclampsia and cardiac arrhythmias. This suggests that intraoperative magnesium sulphate for analgesic purposes is safe to use.
In this study, the morphine-sparing effect did not only involve the early postoperative period after PACU discharge, but also lasted up to 24 h. These same results were found in scoliosis surgery using the same doses of magnesium and ketamine [19]. The possible synergy between these two agents as describe by Liu et al. [24] could explain the longer lasting morphine-sparing effect observed in our study when compared with Tramer’s study, where only a 6-h benefit was reported with the administration of magnesium alone [18]. The cumulative morphine dose was the lowest in the group (Mg + K), but was interestingly higher in the group (K) compared with the group (P), despite the well-known opioid-sparing effect of ketamine (Table 3). The same results were found when interpreting the VAS scores for the three groups (Fig. 1). This could be explained by the relatively low dose of ketamine used. In fact, although we used ketamine at a commonly accepted subanesthetic dose, the analgesic effects at such doses can sometimes be clinically insignificant (5 points reduction on a 100 points pain score as shown by Brinck et al. in their Cochrane review [30]). Therefore, the use of perioperative ketamine at the higher spectrum of the subanesthetic dose range has recently been encouraged (bolus doses up to 0.35 mg/kg and infusions up to 1 mg/kg/h) [36].
Our study did not show a statistically significant reduction in the need for intraoperative remifentanil. But we noted a tendency to decrease remifentanil doses with the addition of magnesium. In contrast, Koinig et al. found a significant reduction in the need for fentanyl in arthroscopic knee surgery using the same doses of magnesium (50 mg kg−1 bolus induction and 8 mg kg−1 h−1 until the end of surgery) [37]. In another study, Ryu et al. used much higher maintenance doses (15 mg kg−1 h−1) but did not find a significant reduction in the consumption of remifentanil. In our study, magnesium doses were calculated according to the ideal weight of obese patients. Administration of magnesium according to the real body weight would result in much higher doses. It is therefore possible that the doses we used are relatively low and the use of higher doses allows a more obvious reduction in perioperative opioid requirements. On the other hand, a larger number of patients could help to investigate the effect of this maintenance dose on the perioperative remifentanil requirements.
On a different note, it is well known that magnesium decreases the release of acetylcholine at the presynaptic neuromuscular junction. It should, in theory, extend the neuromuscular block and therefore, decrease the doses of intraoperative muscle relaxants requirements. Moreover, the risk of a possible residual neuromuscular blockade is deleterious in obese patients because of the pre-existing reduction of their oxygen reserve (decreased functional residual capacity, expiratory reserve volume and total lung capacity). Numerous studies have validated the role of magnesium in the potentiation of the neuromuscular block [38, 39]. In our study, we did not find any significant difference in the need for muscle relaxants between the three groups. This is mainly because neuromuscular transmission was monitored closely throughout the study and additional doses of muscle relaxants were administered based on strict criteria. We tend to believe that such difference could have been more obvious with a larger sample size.
Time to extubation depends on many confounding factors including opioid dose, residual muscle block and level of consciousness. Magnesium has been reported to increase sedation and potentially delay endotracheal extubation after surgery. Such effect was not observed in our study. The mean time to tracheal extubation, measured from discontinuation of sevoflurane, was concordant with other studies using the same definition [40]. Our results and those reported in the literature [35, 41] support the evidence that magnesium administration during bariatric surgery is safe and may decrease the risk of opioid related complications as postoperative morphine consumption was reduced.
We assessed in this study the synergistic effects of magnesium and ketamine in patients undergoing open bariatric surgery. The open approach has quickly lost terrain to laparoscopic techniques that have revolutionized patient care, and lead to decreased postoperative pain scores and earlier recovery [42]. However, in some situations, such as uncontrolled bleeding, bowel injury or adhesions due to surgical revision, a conversion to open surgery is required. In addition, the laparoscopic approach in not devoid of noxious stimuli, and patients often experience discomfort at incision and surgical dissection sites, as well as pain linked to stretching of intra-abdominal cavity, peritoneal inflammation and diaphragmatic irritation and retention of insufflated CO2 in the abdomen after surgery [43, 44]. Finally, opioid-free anaesthesia (OFA) and low opioid anaesthesia both have indications that are procedure and patient related. Obesity in particular is a well-accepted indication for minimizing/nullifying perioperative opioids, irrespective of the surgical technique used. Moreover, OFA has become a part of enhanced recovery after surgery (ERAS) protocols for bariatric interventions [26, 45]. Therefore, it would be interesting to extend the use of magnesium and ketamine combination in the setting of laparoscopic bariatric surgery.
Conclusion
The association of magnesium and ketamine boluses followed by a continuous infusion mode during open bariatric surgery appears to be safe and decreases morphine requirements in the first 24 postoperative hours. This association also shows a tendency to reduce perioperative remifentanil requirements. In the sight of these results, it would be useful to conduct a larger study, to assess the opioid-sparing effect of this association intraoperatively and after 24 h in the postoperative period.
References
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37.
Fernandez AZ, Demaria EJ, Tichansky DS, et al. Multivariate analysis of risk factors for death following gastric bypass for treatment of morbid obesity. Ann Surg. 2004;239:698–703.
Sudré ECM, de Batista PR, Castiglia YMM. Longer immediate recovery time after anesthesia increases risk of respiratory complications after laparotomy for bariatric surgery: a randomized clinical trial and a cohort study. Obes Surg. 2015;25:2205–12.
Egan TD, Huizinga B, Gupta SK, et al. Remifentanil pharmacokinetics in obese versus lean patients. Anesthesiology. 1998;89:562–73.
Guignard B, Bossard AE, Coste C, et al. Acute opioid tolerance intraoperative remifentanil increases postoperative pain and morphine requirement. Anesthesiol J Am Soc Anesthesiol. 2000;93:409–17.
Crawford M, Hickey C, Zaarour C, et al. Development of acute opioid tolerance during infusion of remifentanil for pediatric scoliosis surgery. Anesth Analg. 2006;102:1662–7.
Lee M, Silverman S, Hansen H, et al. A comprehensive review of opioid-induced hyperalgesia. Pain Physician. 2011;14(2):145–61.
Ramasubbu C, Gupta A. Pharmacological treatment of opioid-induced hyperalgesia: a review of the evidence. J Pain Palliat Care Pharmacother. 2011;25:219–30.
Joly V, Richebe P, Guignard B, et al. Remifentanil-induced postoperative hyperalgesia and its prevention with small-dose ketamine. Anesthesiology. 2005;103:147–55.
Song JW, Lee Y-W, Yoon KB, et al. Magnesium sulfate prevents remifentanil-induced postoperative hyperalgesia in patients undergoing thyroidectomy. Anesth Analg. 2011;113:390–7.
Boenigk K, Echevarria GC, Nisimov E, et al. Low-dose ketamine infusion reduces postoperative hydromorphone requirements in opioid-tolerant patients following spinal fusion: a randomised controlled trial. Eur J Anaesthesiol. 2019;36:8–15.
Nielsen RV, Fomsgaard JS, Siegel H, et al. Intraoperative ketamine reduces immediate postoperative opioid consumption after spinal fusion surgery in chronic pain patients with opioid dependency: a randomized, blinded trial. Pain. 2017;158:463–70.
Lahtinen P, Kokki H, Hakala T, et al. S(+)-ketamine as an analgesic adjunct reduces opioid consumption after cardiac surgery. Anesth Analg. 2004:1295–301.
Dahmani S, Michelet D, Abback P-S, et al. Ketamine for perioperative pain management in children: a meta-analysis of published studies. Paediatr Anaesth. 2011;21:636–52.
Elia N, Tramèr MR. Ketamine and postoperative pain – a quantitative systematic review of randomised trials. Pain. 2005;113:61–70.
Iseri LT, French JH. Magnesium: nature’s physiologic calcium blocker. Am Heart J. 1984;108:188–93.
Mebazaa MS, Ouerghi S, Frikha N, et al. Is magnesium sulfate by the intrathecal route efficient and safe? Ann Fr Anesth Reanim. 2011;30:47–50.
Tramer MR, Schneider J, Marti R-A, et al. Role of magnesium sulfate in postoperative analgesia. Anesthesiol J Am Soc Anesthesiol. 1996;84:340–7.
Jabbour HJ, Naccache NM, Jawish RJ, et al. Ketamine and magnesium association reduces morphine consumption after scoliosis surgery: prospective randomised double-blind study. Acta Anaesthesiol Scand. 2014;58:572–9.
Guo B-L, Lin Y, Hu W, et al. Effects of systemic magnesium on post-operative analgesia: is the current evidence strong enough? Pain Physician. 2015;18:405–18.
De Oliveira GS, Castro-Alves LJ, Khan JH, et al. Perioperative systemic magnesium to minimize postoperative pain: a meta-analysis of randomized controlled trials. Anesthesiology. 2013;119:178–90.
Albrecht E, Kirkham KR, Liu SS, et al. Peri-operative intravenous administration of magnesium sulphate and postoperative pain: a meta-analysis. Anaesthesia. 2013;68:79–90.
Savic Vujovic KR, Vuckovic S, Srebro D, et al. A synergistic interaction between magnesium sulphate and ketamine on the inhibition of acute nociception in rats. Eur Rev Med Pharmacol Sci. 2015;19:2503–9.
Liu H-T, Hollmann M, Liu W-H, et al. Modulation of NMDA receptor function by ketamine and magnesium: part I. Anesth Analg. 2001;92:1173–81.
Lemmens HJM, Brodsky JB, Bernstein DP. Estimating ideal body weight – a new formula. Obes Surg. 2005;15:1082–3.
Dang JT, Szeto VG, Elnahas A, et al. Canadian consensus statement: enhanced recovery after surgery in bariatric surgery. Surg Endosc. 2019;
Nagappa M, Weingarten TN, Montandon G, et al. Opioids, respiratory depression, and sleep-disordered breathing. Best Pract Res Clin Anaesthesiol. 2017;31:469–85.
de Boer HD, Detriche O, Forget P. Opioid-related side effects: postoperative ileus, urinary retention, nausea and vomiting, and shivering. A review of the literature. Best Pract Res Clin Anaesthesiol. 2017;31:499–504.
American Society of Anesthesiologists Task Force on Acute Pain Management. Practice guidelines for acute pain management in the perioperative setting: an updated report by the American Society of Anesthesiologists Task Force on acute pain management. Anesthesiology. 2012;116:248–73.
Brinck EC, Tiippana E, Heesen M, Bell RF, Straube S, Moore RA, et al. Perioperative intravenous ketamine for acute postoperative pain in adults. Cochrane Database Syst Rev [Internet]. 2018 [cited 2019 Jun 2]; Available from: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD012033.pub4/full
Peltoniemi MA, Hagelberg NM, Olkkola KT, et al. Ketamine: a review of clinical pharmacokinetics and pharmacodynamics in anesthesia and pain therapy. Clin Pharmacokinet. 2016;55:1059–77.
Levaux C, Bonhomme V, Dewandre PY, et al. Effect of intra-operative magnesium sulphate on pain relief and patient comfort after major lumbar orthopaedic surgery. Anaesthesia. 2003;58:131–5.
O’Flaherty JE, Lin CX. Does ketamine or magnesium affect posttonsillectomy pain in children? Pediatr Anesth. 2003;13:413–21.
Wacker WE, Parisi AF. Magnesium metabolism. N Engl J Med. 1968;278:712–7.
Ryu J-H, Kang M-H, Park K-S, et al. Effects of magnesium sulphate on intraoperative anaesthetic requirements and postoperative analgesia in gynaecology patients receiving total intravenous anaesthesia. Br J Anaesth. 2008;100:397–403.
Schwenk ES, Viscusi ER, Buvanendran A, et al. Consensus guidelines on the use of intravenous ketamine infusions for acute pain management from the American Society of Regional Anesthesia and Pain Medicine, the American Academy of Pain Medicine, and the American Society of Anesthesiologists. Reg Anesth Pain Med. 2018;43:456–66.
Koinig H. Magnesium sulfate reduces intra- and postoperative analgesic requirements. Anesth Analg. 1998;87:206–10.
Dubé L, Granry J-C. The therapeutic use of magnesium in anesthesiology, intensive care and emergency medicine: a review. Can J Anaesth J Can Anesth. 2003;50:732–46.
Fuchs-Buder T, Wilder-Smith OHG, Borgeat A, et al. Interaction of magnesium sulphate with vecuronium-induced neuromuscular block. Br J Anaesth. 1995;74:405–9.
Singh PM, Borle A, McGavin J, et al. Comparison of the recovery profile between desflurane and sevoflurane in patients undergoing bariatric surgery-a meta-analysis of randomized controlled trials. Obes Surg. 2017;27:3031–9.
Schulz-Stübner S, Wettmann G, Reyle-Hahn SM, et al. Magnesium as part of balanced general anaesthesia with propofol, remifentanil and mivacurium: a double-blind, randomized prospective study in 50 patients. Eur J Anaesthesiol. 2001;18:723–9.
Carr BM, Lyon JA, Romeiser J, et al. Laparoscopic versus open surgery: a systematic review evaluating Cochrane systematic reviews. Surg Endosc. 2018:1–17.
Jackson SA, Laurence AS, Hill JC. Does post-laparoscopy pain relate to residual carbon dioxide? Anaesthesia. 1996;51:485–7.
Joris J, Thiry E, Paris P, et al. Pain after laparoscopic cholecystectomy: characteristics and effect of intraperitoneal bupivacaine. Anesth Analg. 1995;81:379–84.
Thorell A, MacCormick AD, Awad S, et al. Guidelines for Perioperative Care in Bariatric Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations. World J Surg. 2016;40:2065–83.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jabbour, H., Jabbour, K., Abi Lutfallah, A. et al. Magnesium and Ketamine Reduce Early Morphine Consumption After Open Bariatric Surgery: a Prospective Randomized Double-Blind Study. OBES SURG 30, 1452–1458 (2020). https://doi.org/10.1007/s11695-019-04317-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-04317-1