Abstract
Introduction
Intussusception represents an uncommon cause of intestinal obstruction after Rouxen-Y gastric bypass. Symptoms are not specific and clinical presentation may vary from acute intestinal obstruction with or without bowel necrosis to intermittent or chronic pain. CT scan is the diagnostic test of choice.
Materials and Methods
A 38-year-old woman who had undergone RYGBP 5 months prior was admitted to our Emergency Department with acute abdominal pain, alimentary and bilious vomiting, and fever. A CT scan revealed an intussusception after the anastomosis and dilatation of the biliopancreatic limb and the gastric remnant. An emergency laparoscopic exploration was performed.
Results
The patient undergoes an explorative laparoscopy. A bowel intussusception starting distally at the jejunojejunostomy and involving the latter is discovered. The common channel is divided first, and after that, the alimentary limb is resected. The biliary limb is identified, marked, and finally divided. A side-to-side jejunojejunal anastomosis is created between the alimentary limb and the common limb. Finally, the anastomosis between the common limb and the biliopancreatic limb is fashioned about 30 cm distally from the latter anastomosis. The total operative time was 130 min. Postoperative course was uneventful, and the patient was discharged on the fifth postoperative day.
Conclusion
Although rare, intussusception after RYGBP must be considered as a possible cause of intestinal obstruction. In case of a small bowel intussusception, a surgical resection is recommended. A laparoscopic approach to treat bowel intussusception after RYGBP is safe and feasible.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intussusception represents an uncommon cause of intestinal obstruction after Roux-en-Y gastric bypass (RYGBP) with a reported prevalence of 0.07% to 1.2% [1, 2]. Even if some cases of anterograde intussusception after RYGBP have been reported, it occurs in a great majority of cases in a retrograde fashion, and it is not triggered by a lead point as generally found in intussusceptions in adults [1,2,3,4,5]. It has been hypothesized that this complication may be due to small bowel motility disturbances caused by the construction of the Roux limb [1, 6]. In addition, even weight loss could play a role in developing intussusception after RYGBP because of less resistance related to the decreased thickness of the mesentery of the intussuscepted segment [1]. Finally, it has been postulated that the suture line at the jejunojejunostomy could act as a lead point, even if this phenomenon does not explain the occurrence of retrograde antiperistaltic intussusception [1, 7, 8].
Symptoms are not specific, and clinical presentation may vary from acute intestinal obstruction with or without bowel necrosis to intermittent or chronic pain [1]. CT scan is the diagnostic test of choice as it shows the typical “target” sign in about 80% of cases [9].
Concerning the treatment, different options exist, including only the reduction of the intussuscepted segment or with concomitant enteropexy, plication, or resection with or without revision of the jejunojejunostomy [2]. However, resection of the intussuscepted bowel or of the jejunojejunal anastomosis (if involved) seems to be preferred over a simple reduction or reduction and various types of intestinal plications because of a lower risk of recurrence [1, 4, 10, 11]. The operation can be performed by laparoscopy or by laparotomy according to the clinical presentation, the patient’s clinical state, and the experience of the surgeon [2, 12]. Nevertheless, in case of intussusception after RYGBP, a conservative management should be discouraged [1, 13].
Materials and Methods
A 38-year-old woman who had undergone RYGBP 5 months prior was admitted to our Emergency Department with acute abdominal pain, alimentary and bilious vomiting, and fever. The patient reported typical symptoms of intestinal obstruction including cessation of bowel function and nausea. Physical examination showed intense abdominal pain located in the upper left part of the abdomen.
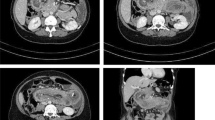
The patient’s blood count showed a high white blood cell count (19,000/μL). A CT scan revealed an intussusception after the anastomosis and dilatation of the biliopancreatic limb and the gastric remnant. An emergency laparoscopic exploration was performed.
Results
Video run time is 6:14 min. First, the video shows the preoperative CT scan: an intussusception located at the jejunojejunostomy site is evidently causing a dilatation of the biliopancreatic limb and the gastric remnant.
(MP4 359,761 kb)
The patient undergoes an explorative laparoscopy. The alimentary limb is explored, starting from the gastrojejunal anastomosis. A bowel intussusception starting distally at the jejunojejunostomy and involving the latter is discovered. After some unsuccessful attempts to decompress the biliopancreatic limb and to reduce intussusception, the decision to resect the jejunojejunal anastomosis is taken. The common channel is divided first, and after that, the alimentary limb is resected. In sectioning the mesentery at the jejunojejunal anastomosis, great attention is paid to preserve adequate blood supply to the alimentary limb. Then, the mesentery of the intussuscepted limb is divided. The biliary limb is identified, marked, and finally divided.
A side-to-side jejunojejunal anastomosis is created between the alimentary limb and the common limb. Finally, the anastomosis between the common limb and the biliopancreatic limb is fashioned about 30 cm distally from the latter anastomosis. The mesentery is closed using a running barbed suture.
The total operative time was 130 min. Postoperative course was uneventful, and the patient was discharged on the fifth postoperative day.
Conclusion
Although rare, intussusception after RYGBP must be considered as a possible cause of intestinal obstruction. Presentation can be vague, and clinical examination can be unhelpful [1, 14]. A CT scan is an important diagnostic tool in bariatric patients and can help find typical signs that lead to the appropriate diagnosis [9].
In case of clinical suspicion of intestinal obstruction in a patient who had previously undergone RYGBP, an explorative laparoscopy should be performed. If a small bowel intussusception is found, above all in case of ischemia, a surgical resection is recommended [1, 12]. A laparoscopic approach to treat bowel intussusception after RYGBP, even if it occurs at the jejunojejunostomy site, appears to be safe and feasible.
References
Daellenbach L, Suter M. Jejunojejunal intussusception after Roux-en-Y gastric bypass: a review. Obes Surg. 2011;21:253–63.
Varban O, Ardestani A, Azagury D, et al. Resection or reduction? The dilemma of managing retrograde intussusception after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2013;9:725–30.
Bocker J, Vasile J, Zager J, et al. Intussusception: an uncommon cause of postoperative small bowel obstruction after gastric bypass. Obes Surg. 2004;14:116–9.
Coster DD, Sundberg SM, Kermode DS, et al. Small bowel obstruction due to antegrade and retrograde intussusception after gastric bypass: three case reports in two patients, literature review, and recommendations for diagnosis and treatment. Surg Obes Relat Dis. 2008;4:69–72.
Zainabadi K, Ramanathan R. Intussusception after laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2007;17:1619–23.
Hocking MP, McCoy DM, Vogel SB, et al. Antiperistaltic and isoperistaltic intussusception associated with abnormal motility after Roux-en-Y gastric bypass: a case report. Surgery. 1991;110:109–12.
Duane TM, Wohlgemuth S, Ruffin K. Intussusception after Roux-en-Y gastric bypass. Am Surg. 2000;66:82–4.
Wittgrove AC, Clark GW. Laparoscopic gastric bypass, Roux-en-Y-500 patients: technique and results, with 3-60 month follow-up. Obes Surg. 2000;10:233–9.
Gayer G, Zissin R, Apter S, et al. Pictorial review: Adult intussusception—a CT diagnosis. Br J Radiol. 2002;75:185–90.
Simper SC, Erzinger JM, McKinlay RD, et al. Retrograde (reverse) jejunal intussusception might not be such a rare problem: a single group’s experience of 23 cases. Surg Obes Relat Dis. 2008;4:77–83.
Stephenson D, Moon RC, Teixeira AF, et al. Intussusception after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2014;10:666–70.
Jenkins M, Chui P, Parikh M. Laparoscopic treatment of intussusception after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2017;13:364–5.
Ver Steeg K. Retrograde intussusception following Roux-en-Y gastric bypass. Obes Surg. 2006;16:1101–3.
Shaw D, Huddleston S, Beilman G. Anterograde intussusception following laparoscopic Roux-en-Y gastric bypass: a case report and review of the literature. Obes Surg. 2010;20:1191–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
The procedure involving human participation performed in this study was in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from the participant included in this study.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Facchiano, E., Soricelli, E., Leuratti, L. et al. Intussusception After Roux-en-Y Gastric Bypass: Laparoscopic Management. OBES SURG 28, 2145–2147 (2018). https://doi.org/10.1007/s11695-018-3265-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3265-1