Abstract
Intussusception after open Roux-en-Y gastric bypass procedure (RYGBP) is a rare complication. We present a retrospective review of three cases of antegrade intussusception occurring after laparoscopic RYGBP. To our knowledge, these are the first documented cases of intussusception after laparoscopic RYGBP. We describe the clinical presentation and our management of these three cases. Furthermore, we believe that the initial clinical presentation, radiographic findings, and management of these patients may be different than those patients who have undergone an open RYGBP. With increasing popularity of laparoscopic RYGBP, we are likely to see more of this entity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intussusception is a rare cause of small bowel obstruction (SBO) accounting for approximately 1% of all cases of SBO. It has been described after various gastrointestinal procedures such as esophagectomy, gastrectomy, and jejunoileal bypass [1]. In 90% of cases, it has been associated with a definable bowel lesion serving as a “lead point” [2, 3]. These lesions include tumors, adhesions, and local intestinal inflammation, which can serve as lead points by fixing the bowel or impairing intestinal motility [4–6].
With the increasing popularity of Roux-en-Y gastric bypass (RYGBP) as the surgical treatment of choice for morbid obesity, several cases of intussusception after RYGBP, have been described so far in the literature. Up to now, there have been nine cases of jejunojejunal intussusception and two cases of gastrojejunal intussusception that have been described [1–3, 7–10]. All of these cases have occurred in patients with significant and rapid weight loss (usually >45 kg). Furthermore, all the cases have occurred after open RYGBP at the common channel just distal to the jejunojejunal anastomosis. Although both antegrade (isoperistaltic) and retrograde (antiperistaltic) types have been described, the majority of the cases seem to be of the retrograde type. These patients were treated by open exploration and resection of the intussuscepted segment of small bowel.
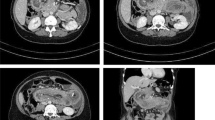
Our case series of three patients is unique in several aspects. All the three cases occurred after laparoscopic RYGBP, and the presentation was subacute rather than acute. Intraoperatively, although the intussuscepted bowel was in the common channel, it was not in proximity to the jejunojejunostomy. Furthermore, all three cases were antegrade. Rather than an open exploration, and resection, we were able to explore all three patients laparoscopically and reduce the intussuscepted bowel without resection. This allowed all three patients to be discharged home on postoperative day 1 (Table 1, Fig. 1).
Case 1
Thirty-one-year-old female status post-laparoscopic RYGBP in 2004, with 47 kg weight loss, presented 10 months later with a 3-day history of acute onset of abdominal pain. On examination, she was afebrile, and heart rate was 59 beats/min. Her abdomen was soft with mild tenderness in the left upper quadrant. Her white blood cell count was 5,600 cells/ml. A contrast-enhanced computed tomography (CT) scan of the abdomen was obtained, which was normal. She was admitted for 2 days, during which her pain completely resolved. She was scheduled for a diagnostic laparoscopy a week later. Intraoperative findings included small bowel intussusception involving the common channel 30 cm distal to the jejunojejunostomy. The intussusception was antegrade, and the length of intussuscepted segment of bowel was 15 cm. There was evidence of mildly dilated loops of bowel proximal to the intussusception and collapsed loops of bowel distal to it. The intussusception was reduced without any difficulty, and after reduction, the bowel was viable. Exploration of the rest of the abdomen, including laparoscopic palpation of the small bowel looking for intraluminal lesions, did not reveal any other abnormalities serving as lead points. The patient was discharged home on postoperative day 1 tolerating a regular diet. After a 22-month follow-up, she has not had any signs of recurrence.
Case 2
Forty-four-year-old female status post-laparoscopic RYGBP in 2004, with 71 kg weight loss, presented 30 months later with intermittent severe sharp periumbilical and epigastric pain associated with bloating and, at times, relieved by passing flatus or bowel movement. The pain worsened by eating. On examination, she was afebrile, and her heart rate was 64 beats/min. Her abdomen was soft but with some epigastric tenderness, without rebound or guarding. Her white blood cell count was 7,900 cells/ml. A contrast-enhanced CT scan of the abdomen was negative for bowel obstruction. By the time she was seen in the Emergency Department, her pain had completely resolved. She had experienced two other episodes, during which she was admitted to the hospital. She was scheduled for a diagnostic laparoscopy 5 days later. Intraoperative findings included small bowel intussusception involving the common channel 15 to 20 cm distal to the jejunojejunostomy. The intussusception was antegrade, and the length of intussuscepted segment of bowel was 10 cm. The intussusception was reduced without any difficulty, and after reduction, the bowel was viable. Exploration of the rest of the abdomen, including laparoscopic palpation of the small bowel looking for intraluminal lesions, did not reveal any other abnormalities serving as lead points. The patient was discharged home on postoperative day 1 tolerating a regular diet. After a 26-month follow-up, she has not had any signs of recurrence.
Case 3
Twenty-seven-year-old female status post-laparoscopic RYGBP in 2003, with 70 kg weight loss, presented 42 months later with symptoms of severe intermittent colicky left upper quadrant abdominal pain for a 2- to 3-week period. Her pain was exacerbated with eating or drinking. On examination, she was afebrile, and her heart rate was 68 beats/minute. Her abdomen was soft and non-tender. Her white blood cell count was 7,100 cells/ml. A contrast-enhanced abdominal CT scan revealed occasional loops of dilated small bowel. She was admitted for 2 days, and her symptoms were successfully treated conservatively. She was scheduled for diagnostic laparoscopy a week later. Intraoperative findings included small bowel intussusception involving the common channel 30 to 40 distal to the jejunojejunostomy. The intussusception was antegrade, and the length of intussuscepted segment of bowel was 10 cm. The intussusception was reduced without any difficulty, and after reduction the bowel was viable. Exploration of the rest of the abdomen, including laparoscopic palpation of the small bowel looking for intraluminal lesions, did not reveal any other abnormalities serving as lead points. The patient was discharged home on postoperative day 1 tolerating a regular diet. She is doing well after a 3-month follow-up.
Discussion
The RYGBP has become the most common method of surgical treatment of morbid obesity in the USA. Complication rates occur in 3–20% of all patients undergoing this procedure. Complications range from simple wound infection to anastomotic leak, strictures, marginal ulcers, deep venous thrombosis, and intestinal obstruction [7]. Frequency of SBO after laparoscopic RYGBP is reported to be between 0.2 and 4.5%, and it can occur months or years after surgery. Common causes of SBO include internal hernia at the mesocolic window and Peterson’s defect (jejunal mesenteric window) [10]. Although much less frequently seen, intussusception of the small bowel should also be included in the differential diagnosis of SBO in patients who have undergone RYGBP [8]. Although rare and often overlooked, intussusception can lead to serious complications from ischemia and necrosis of the intussuscepted segment.
In general, the clinical presentation of intussusception can be variable, and most patients do not present with a consistent history and do not appear ill. This is particularly true in bariatric patients whose presentations are vague and physical findings are unreliable. Presenting symptoms include abdominal pain, nausea and vomiting, and bloody stool.
The most common presenting sign is vague abdominal pain [10]. The severity of pain is often out of proportion to the physical exam findings [1]. Physical findings include abdominal tenderness, abdominal mass, and peritoneal irritation [10]. As in our case series, absence of obstruction symptoms and physical findings do not exclude intussusception. Furthermore, the symptoms can range from acute onset to subacute and intermittent [10]. In the acute form, patients report onset of pain within 24 h with progressive worsening of symptoms. In the subacute form, the patients have recurrent episodes of vague abdominal pain and cramping exacerbated by eating [10].
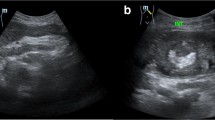
Given that the presentation can be variable and the symptoms misleading, a high index of suspicion is needed to avoid potential complications and adverse outcomes. Plain abdominal films have a low sensitivity in establishing diagnosis. CT scan has established itself as the diagnostic modality of choice with a reported diagnostic accuracy of 80% [10]. Pathognomonic findings include early target mass seen on the axial images and a sausage-like mass seen on the reconstructed sagittal images [10]. However, as in our cases, a normal CT does not exclude the presence of intussusception.
Interestingly, in the majority of patients who have presented with intussusception after RYGBP, there has been a history of significant and rapid weight loss [10]. One series of four patients showed a 90 to 104.5% excess weight loss [9]. Similarly, in our series, the average excess weight loss was 109.3%.
In general, the intussusception can propagate in an antegrade or retrograde direction. Most intussusceptions after RYGBP are retrograde, and most, if not all, appear to originate in the proximal common channel [10]. However, in the two patients reported by Bocker et al. [7], the intussusception originated in the afferent limb and progressed distally in an antegrade direction toward the jejunojejunostomy. Similarly, in all of our cases, the intussusception occurred in the antegrade fashion.
The cause of intussusception after RYGBP remains poorly understood and may be multifactorial. Proposed theories include the involvement of a lead point (suture lines, adhesions, and lymphoid hyperplasia), motility disturbances, and aberrant intestinal pacemakers [10].
Duane et al. [2] suggested that the suture lines might act as a lead point. This explains why all the cases described so far in the literature have occurred at the proximity of the jejunojejunal anastomosis. Given that all the cases described so far have occurred in open RYGBP cases, adhesions have been proposed as the culprit in the formation of intussusception [10].
Disordered motility seems to be the most accepted theory. This theory involves the appearance of an ectopic pacemaker that generates pacesetter potentials that propagate in a retrograde direction [2]. Motility disturbances of the Roux limb after Roux-en-Y gastroenterostomy have also been described in an animal model [11]. Steeg et al. [9] have suggested that this ectopic pacesetter in the Roux limb along with the normal pacesetter in the duodenum may cause two peristaltic contractile waves to reach the jejunojejunostomy simultaneously, producing a high amplitude peristaltic wave in the proximal common channel, which would engulf the quiescent bowel distal to it. This theory would explain why most intussusceptions after RYGBP occur in a retrograde fashion and at the very proximal common channel.
However, in our case series, all three intussusceptions occurred a good distance from the anastomosis. Furthermore, given that all our RYGBP were performed laparoscopically, we encountered minimal adhesions at the second operation. These findings argue against adhesions or staple lines playing a role in the etiology of intussusception. Although the presence of an ectopic pacemaker may be the culprit in the cause of intussusception, it would not completely explain why all three of our cases occurred in an antegrade fashion rather than retrograde as proposed by Steeg et al. [9].
An interesting observation we have made during all of our cases is that, after significant weight loss, the small bowel mesentery of these patients is extremely thin, floppy, and redundant. This observation may suggest that the lack of a thick mesentery to tether the small bowel in combination with small bowel dysmotility may lead to intussusception in an antegrade fashion. Additionally, given that intussusception can occur distal to the jejunojejunostomy, we recommend complete inspection of small bowel, especially the common channel, in patients explored for symptoms of SBO without a readily explained cause such as an internal hernia. Furthermore, in absence of a readily discernable etiology, we also recommend laparoscopic palpation of the small bowel to rule out intraluminal lesions that can serve as a lead point.
The treatment of intussusception after RYGBP is not well established. In the presence of gross bowel necrosis, resection is necessary. However, if the bowel appears viable, the need for resection is controversial. Hocking et al. [3] performed a reduction and Noble Plication after the recurrence of the intussusception that was initially treated with resection and primary anastomosis. However, the efficacy of small bowel fixation methods such as Noble plication in the prevention of recurrence of intussusception is not well established. In review of the literature, all other cases of intussusception after RYGBP have been treated with open exploration and bowel resection [10]. Edwards et al. [10] recommend expeditious exploration, anastomotic resection and reconstruction to avoid the possibility of unrecognized necrosis, and the risk of perforation. In all three of our cases, we were able to proceed with laparoscopic reduction of the intussusception without a need for resection or small bowel fixation such as Noble plication. Whether this would lead to recurrence in these patients is not known.
Conclusion
Intussusception is a rare cause of SBO or intermittent abdominal pain after RYGBP. We report the first case series of intussusception after laparoscopic RYGBP that were managed laparoscopically without the need for bowel resection. As the number of laparoscopic RYGBP procedures continues to rise, we will likely see more of this entity. Further studies to elucidate the etiology and a consensus for its management are warranted.
References
Goverman J, Greenwald M, Gadaleta D, et al. Antiperistaltic [retrograde] intussusception after Roux-en-Y gastric bypass. Am Surg 2004;70:67–70.
Duane TM, Wohlgemuta S, Ruffin K. Intussusception after Roux-en-Y gastric bypass. Am Surg 2001;66:82–4.
Hocking MP, McCoy DM, Vogel SB, et al. Antiperistaltic and isoperistaltic intussusception associated with abnormal motility after Roux-en-Y gastric bypass: a case report. Surgery 1991;110:109–12.
Begos DG, Sandor A, Modin IM. The diagnosis and management of adult intussusception. Am J Surg 1997;173:88–94.
Toso C, Erne M, Lenzlinger PM. Intussusception as a cause of bowel obstruction in adults. Swiss Med Wkly 2005;135:87–90.
Huang WS, Changchien CS, Lu SN. Adult intussusception: a 12-year experience, with emphasis on etiology and analysis of risk factors. Chang Gung Med J 2000;23:284–90.
Bocker J, Vasile J, Zager J, Goodman E. Intussusception: an uncommon cause of postoperative small bowel obstruction after gastric bypass. Obes Surg 2004;14:116–9.
Majeski J, Fried D. Retrograde intussusception after Roux-en-Y gastric bypass surgery. J Am Coll Surg 2004;199:988–9.
Steeg K. Retrograde intussusception following Roux-en-Y gastric bypass. Obes Surg 2006;16:1101–3.
Edwards M, Grinbaum R, Ellsmere J. Intussusception after Roux-en-Y gastric bypass for morbid obesity: case report and literature review of rare complication. Surg Obes Relat Dis 2006 Jul–Aug;2(4):483–9.
Tu BN, Kelly KA. Motility disorders after Roux-en-Y gastrojejunostomy. Obes Surg 1994;4:219–26.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zainabadi, K., Ramanathan, R. Intussusception After Laparoscopic Roux-en-Y Gastric Bypass. OBES SURG 17, 1619–1623 (2007). https://doi.org/10.1007/s11695-007-9291-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-007-9291-z