Abstract
Background
In the USA, three types of bariatric surgeries are widely performed, including laparoscopic sleeve gastrectomy (LSG), laparoscopic Roux-en-Y gastric bypass (LRYGB), and laparoscopic adjustable gastric banding (LAGB). However, few economic evaluations of bariatric surgery are published. There is also scarcity of studies focusing on the LSG alone. Therefore, this study is evaluating the cost-effectiveness of bariatric surgery using LRYGB, LAGB, and LSG as treatment for morbid obesity.
Methods
A microsimulation model was developed over a lifetime horizon to simulate weight change, health consequences, and costs of bariatric surgery for morbid obesity. US health care prospective was used. A model was propagated based on a report from the first report of the American College of Surgeons. Incremental cost-effectiveness ratios (ICERs) in terms of cost per quality-adjusted life-year (QALY) gained were used in the model. Model parameters were estimated from publicly available databases and published literature.
Results
LRYGB was cost-effective with higher QALYs (17.07) and cost ($138,632) than LSG (16.56 QALYs; $138,925), LAGB (16.10 QALYs; $135,923), and no surgery (15.17 QALYs; $128,284). Sensitivity analysis showed initial cost of surgery and weight regain assumption were very sensitive to the variation in overall model parameters. Across patient groups, LRYGB remained the optimal bariatric technique, except that with morbid obesity 1 (BMI 35–39.9 kg/m2) patients, LSG was the optimal choice.
Conclusion
LRYGB is the optimal bariatric technique, being the most cost-effective compared to LSG, LAGB, and no surgery options for most subgroups. However, LSG was the most cost-effective choice when initial BMI ranged between 35 and 39.9 kg/m2.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2008, approximately 1.4 billion adults were considered overweight worldwide [1]. Of the 1.4 billion adults, approximately 300 million women and > 200 million men were estimated to be obese. Twelve million adults in the USA are considered morbidly obese with body mass index (BMI) ≥ 40 kg/m2 [2].
Obesity is associated with several comorbidities that increase mortality rates [3]. It is associated with hypertension, coronary artery disease, dyslipidemia, metabolic liver disease, renal and urological diseases, sleep apnea, diabetes, osteoarthritis, psychiatric comorbidity, gastroesophageal reflux disease (GERD), and various cancers [4].
Behavioral therapy, diet, and weight reduction medications have been shown to be ineffective on morbidly obese patients [5,6,7]; since 2003, the use of surgery to treat morbid obesity has increased [8]. Bariatric surgery is considered as a treatment option for class III (BMI ≥ 40 kg/m2) or class II (BMI 35.0–39.9 kg/m2) obesity with obesity-related comorbidities that have previously not been successfully treated with nonsurgical interventions [9]. The long-term effect of bariatric surgery was proven to be successful with mean excess weight loss beyond 60%, but the short- and long-term surgical complication rate is relatively large [10, 11].
In the USA, three types of bariatric surgeries are widely performed, including laparoscopic sleeve gastrectomy (LSG), laparoscopic Roux-en-Y gastric bypass (LRYGB), and laparoscopic adjustable gastric banding (LAGB). LRYGB is most commonly performed and considered the gold standard technique due to its high level of efficacy [12, 13]. However, it is a very demanding technique and may require a longer learning curve. LAGB was used for many years by surgeons due to reversibility, technical simplicity, and lower postoperative complications. Nevertheless, LAGB showed significantly lower excessive weight loss than LRYGB [11]. LSG is considered the newest technique for morbid obesity. The advantage of LSG is that this procedure is easier to perform technically. This technique results in similar excess weight loss when comparing against the LRYGB [14].
Despite the obesity pandemic, few economic evaluations of bariatric surgery are published in the USA. There is also scarcity of studies focusing on the LSG alone. Therefore, the aim of this study is to assess the cost-effectiveness of bariatric surgery for morbid obesity in the USA using three different techniques.
Methods
Model Overview
A microsimulation model was developed using TreeAge Pro 2017 to project the cost-effectiveness of bariatric surgery using three different techniques as treatment for morbid obesity versus no surgery. This model concentrates on the change of BMI and surgical-related complications as predictors of lifetime cost, survival, and health-related quality of life. Patients’ movements through the model were mainly dependent on their BMI or death.
After the initial surgical period, patients transitioned through five different health states that reflected their current BMI level (not obese (BMI ≤ 30 kg/m2), obese (BMI 30–34.9 kg/m2), morbidly obese I (BMI 35–39.9 kg/m2), morbidly obese II (BMI 40–49.9 kg/m2), and super obese (BMI ≥ 50 kg/m2)) and death (Fig. 1). Health care sector perspective and lifetime horizon were used. Yearly cycle length was used to determine transitions between health states.
Model Population
A model was propagated based on a report from the first report of the American College of Surgeons [15]. The model was incorporated with different patient characteristics: age, sex, and BMI. The analysis in this model was limited to adult aged 18 to 74 years with BMI ≥ 35 kg/m2. Initial BMI ranged between 35 and 69, and 78% were female.
Model Parameters
All probability cost and utilities were derived from previously published studies and publicly available data sources (Table 1). In addition, an expert opinion in bariatric surgery was used to supplement the model.
Surgical Efficacy for Weight Management
For no surgical intervention, patients maintained their initial BMI level for the duration of the model. However, LRYGB and LAGB interventions were based on a randomized clinical trial with a 10-year follow-up [16, 17]. For LSG, observational studies with an 8-year follow-up were used [18, 19]. To our knowledge, that was the best and longest follow-up available in the literatures. In the base case analysis, we assumed that BMI levels remained constant after the first 10 years for LRYGB and LAGB and after the first 8 years for LSG.
Surgical Complications and Mortality
Based on the first report data of the American College of Surgeons, patients who undergo the surgery experienced a small risk of death in the first 30 days from the surgical interventions [15]. Background mortality was calculated based on age, BMI, and sex from the US Third National Health and Nutritional Examination Survey data [3]. Surgical-related complications were classified by severity. Complications were divided into early major surgical complications (e.g., reoperation due to surgical complications) or early minor complications (e.g., readmission for infection or dehydration) for the first 30 days based on the first report data from the American College of Surgeons [15]. In addition, after the first 30 days, the calculated probability of experiencing late surgical complications was based on data from meta-analysis and observational study with 12 years of follow-up [20, 24, 25]. We assumed that the annual probability of late complications of surgery was constant in the first 4 years, half in years 5 to 10, and zero after that [2]. Morbidly obese patients who did not receive surgery assumed to not have serious complications throughout the model.
Costs
The model included the cost associated with surgery, surgical-related complications, and health care costs associated with each BMI level. Previous cost-effectiveness models in bariatric surgery that were published in the USA were used to estimate the pre- and postoperative costs associated with bariatric surgery [2, 3, 22]. We consulted our clinical experts and prior published studies regarding the schedule of follow-up visits as follows: five visits in year 1, two visits in year 2, and one annual visit afterward for LSG; six visits in year 1, two visits in year 2, and one annual visit afterward for LRYGB; and nine visits in year 1, two visits in year 2, and one annual visit afterward for LAGB [2]. Medical expenditures specific to each BMI level were based on the US Medical Expenditure Panel Survey (MEPS) data [26]. Health care costs for treating obesity-related comorbidities were included in overall cost [26]. All costs from earlier years were inflation-adjusted to 2016 US dollars using the Consumer Price Index for medical care [27].
Health-Related Quality of Life
Different initial utility decrements were applied for all patients who had bariatric surgery and were applied for 6 weeks [2, 28, 29]. Also, decrements associated with earlier and late surgical-related complications for each severity level were incorporated into the model. Utility decrements were applied for 6 weeks for major complications and 4 weeks for minor complications [2, 28, 29].
BMI-specific utilities were calculated and stratified by age from the MEPS data [30]. We indirectly calculated utilities by approximating EuroQol five-dimension questionnaire (EQ-5D) scores from Short Form Health Survey version 2 (SF-12v2) using physical component summary (PCS) and mental component summary (MCS) score that are collected in the MEPS data [26]. For patients who did not have bariatric surgery, the assumption was made that their health-related quality of life did not change for the duration of the model except that it can decrease a bit as they age (Table 2).
Base Case Cost-Effectiveness Analysis
Total costs, quality-adjusted life-years (QALYs), and incremental cost-effectiveness ratios (ICERs) were estimated for each treatment strategy. Treatments were ranked per their QALYs. Thus, ICERs were calculated by comparing the most effective with the less effective and dividing the incremental cost with the incremental effectiveness. We stratified the base analysis by age, sex, and initial BMI. A willingness to pay (WTP) $100,000 per QALY was used as a threshold to recognize which treatment was most cost-effective. All costs and QALYs were discounted by 3% annually.
Sensitivity Analyses
Patients were assumed to regain half of their cumulative BMI after the first 10 years. In addition, the uncertainty and sensitivity of model inputs were assessed by performing a one-way sensitivity analysis and probabilistic sensitivity analysis (PSA). Different probabilistic distributions were used to reflect the underlying parameter of uncertainty [31].
Results
Base Case Results
The base case analysis results are reported in (Table 3). Results are presented over aggregate patient populations and stratified by initial BMI level, gender, and starting age. All bariatric techniques enhanced health outcomes compared to no surgery. These techniques offered extra discounted QALYs by 1.39 (LSG), 1.90 (LRYGB), and 0.93 (LAGB) for all treated patients. The ICERs for LSG versus no surgery, LRYGB versus no surgery, and LAGB versus no surgery were below $10,000 per QALY.
LRYGB was the optimal bariatric technique and most cost-effective compared to LSG, LAGB, and no surgery options. LRYGB has the maximum net monetary benefit (NMB) over a WTP range of $10,000–100,000. However, results change by running the model for short-term horizon at 8 to 10 years, i.e., within the data provided by these trials, and no surgery becomes the cost-effectiveness choice. In addition, bariatric surgery becomes cost-effective when model runs 12 years and more.
Across patient groups, results did not change and LRYGB remained the optimal bariatric technique, being most cost-effective compared to other options, except that with morbid obesity 1 (BMI 35–39.9 kg/m2) patients, LSG was the optimal choice with higher NMB. Subgroup analysis results displayed that bariatric surgery, particularly LRYGB, was more cost-effective for females and young patients with higher initial BMI (Table 3).
Sensitivity Analyses
One-way sensitivity analysis was performed over the base case values (Table 4). Most of the variations in the aggregate ICERs have less than $25,000 per QALY gain. However, the model was more sensitive to the maximum initial cost of bariatric techniques, late major surgical complication cost, and weight regain after the first 10 years.
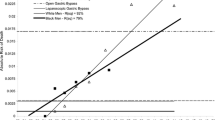
PSA on the aggregate patient populations over the lifetime horizon was performed (Fig. 2). PSA results are shown in cost-effective acceptability curves by providing the probabilities that each treatment option for morbid obesity would be considered cost-effective for different willingness-to-pay thresholds from the health care sector perspective. All aggregate patient population results did vary across willingness-to-pay thresholds. LRYGB was the optimal choice by performing 1000 PSA iterations using a cost-effectiveness threshold of 100,000 per QALY being cost-effective.
Discussion
In this cost-effectiveness study, we demonstrate the benefits of bariatric surgery, particularly LRYGB, as a treatment of morbid obesity. This model evaluated treatments related to mortality, complications, and weight loss as predictors of lifetime cost, health-related quality of life, and survival. To understand and evaluate the effect of the uncertainty around our analysis, deterministic and probabilistic sensitivity analyses were presented.
The base case analysis results reveal that bariatric surgery (LSG, LRYGB, and LAGB) is cost-effective when compared to no surgery. Furthermore, LRYGB was superior and the most cost-effective bariatric technique versus LSG and LAGB. Generally, the ICERs of bariatric surgery were lower for females, younger patients, and those who had higher initial BMI. LSG was observed to be the most cost-effective choice when initial BMI ranged between 35 and 39.9 kg/m2. However, LRYGB was the optimal choice if the patient had BMI more than 40 kg/m2. Deterministic and probabilistic sensitivity analyses showed that this cost-effectiveness result was very sensitive to the initial cost of bariatric techniques, late major surgical complication cost, and weight regain assumption.
The results of this study are similar to those of previous studies in the literature; these cost-effectiveness studies showed bariatric surgery was most cost-effective compared to no surgery [2, 22, 32, 33]. It was found in the USA, the results varied by gender and initial BMI. Bariatric surgery seems to be the most cost-effective for females and patients with higher initial BMI [2, 32]. In addition, it was discovered in Sweden that bariatric surgery was cost saving for all obese patients (severely, morbidly, and super obese) [34]. Fewer studies show evidence of cost saving associated with bariatric procedures [34]. Studies that were performed in Portugal and Spain yielded similar results to this study [35, 36], due to the use of long-term data in those models.
In the 10 years of efficacy of our study, data for bariatric surgery was incorporated [16,17,18,19] and was the longest follow-up available in the literature to our knowledge. Long-term and high-quality comparative data for the effectiveness of LSG, LRYGB, and LAGB was very limited in the literature; this may be due to loss to follow-up as well as changes in overall practices. Furthermore, head-to-head trials or long-term observational studies evaluating all bariatric techniques (LSG, LRYGB, and LAGB) together are lacking. Generating such evidence in the future may help to enhance the accuracy of the results and reduce uncertainty around the estimation of the cost-effectiveness analysis.
Showing the cost-effectiveness of bariatric surgery in USA is not new; however, evaluating the cost-effectiveness of newer techniques for morbid obesity such as laparoscopic sleeve gastrectomy in the past has not been previously conducted. Furthermore, fewer cost-effectiveness studies explore the heterogeneity among different morbidly obese subgroups. Deciphering which subgroup may experience greater expenditure reductions than others will increase the personalization of treatments. For example, the recent study with data collected from 204 LSG patients confirmed that LSG was effective particularly with lower BMI patients (35–43 kg/m2) [29]; however, this may be in discordance with some insurance companies who favor LSG for patients with higher BMI levels. LAGB intended to be favored for patient with low BMI (35–39 kg/m2) because they have smaller weight to lose. Yet, LAGB was proven inferior to weight reduction and plasma ghrelin levels [16, 17, 29, 37].
The use of lifetime horizon was an essential parameter since obesity is considered a chronic condition. Further, the Swedish Obese Subjects (SOS) trial revealed that the benefit of bariatric surgery on morbidly obese patients continued 20 years after surgery [38]. Choosing lifetime horizon in this model was consistent with SOS study results to capture how the frequency of morbid obesity-related events is reduced. This model also did compare LSG, LRYGB, and LAGB separately due to weight loss and complication of risk that differs according to the type of bariatric techniques.
On the other hand, our model did have some limitations. Several assumptions were made in this model. The first major assumption was that patients who were undergoing surgery had similar risk profile to those not undergoing surgery; however, there are many times given the requirements for bariatric surgery that some baseline characteristics differed between surgical and nonsurgical patients.
The second major assumption was that patients who did not undergo a surgical intervention maintained their initial BMI level for the duration of the model. This assumption was based on the ineffectiveness of usual care for morbidly obese patients [39]. There are several studies that suggest that obese, especially morbidly obese patients, will continue to gain weight without the assistance of bariatric surgery as well as accrue other comorbid conditions; for example, one such study illustrates that the mortality reduction is approximately 89%, as well as reduction in cardiovascular, endocrine, and mental health issues to name a few [40]. There is a high possibility that patients may regain weight and the severity of obesity may increase by age for morbidly obese patients who do not receive bariatric surgery [41]. Therefore, this assumption may have overestimated the benefit of no surgical intervention. If we included this information in the model, we could expect bariatric surgery to be more cost-effective and more attractive than what it is currently performed. However, we tried to design this model under conservative assumptions and show conservative results.
There was a lack of bariatric surgery-specific utility decrement data from literatures. Surrogate estimates were incorporated for laparoscopic surgery for hernia repair to overcome the lack of utility data. Extrapolation beyond clinical trials was necessary to model the outcomes as only 10-year randomized clinical trial data for LRYGB and LAGB and 8-year observational data for LSG were incorporated. Long-term comparative effectiveness data is needed to reduce the amount of assumptions made in this model.
Conclusions
All types of bariatric surgeries show significant weight loss compared to no surgery. LRYGB is the optimal bariatric technique, being most cost-effective compared to LSG, LAGB, and no surgery options for most subgroups. However, LSG was the cost-effective choice when initial BMI ranged between 35 and 39.9 kg/m2. Once a patient is considered for surgery, LRYGB seems the most cost-effective choice; however, other approaches to reducing obesity (e.g., legislation and taxation that targets consumer behavior) also need to be evaluated in the future.
References
World Health Organization. http://www.who.int/medicentre/factsheets/fs311/en/. Accessed 31 Mar 2016.
Campbell J, McGarry L, Shikora S, et al. Cost-effectiveness of laparoscopic gastric banding and bypass for morbid obesity. Am J Manag Care. 2010;16:174–87.
Fontaine K, Redden D, Wang C, et al. Years of life lost due to obesity. JAMA. 2003;289:187–93.
The Comptroller and Auditor General. Tackling obesity in England. https://www.nao.org.uk/wp-content/uploads/2001/02/0001220.pdf. Accessed 31 Mar 2016.
NIH Technology Assessment Panel. Methods for voluntary weight loss and control. Proceedings of NIH Technology Assessment Conference, Bethesda, MD, March 30–April 1, 1992. Ann Intern Med.1993;119:641–770.
Bray G, Ryan D, Gordon D, et al. Double-blind randomized placebo-controlled trial of sibutramine. Obes Res. 1996;4:263–70.
Davidson MH, Hauptman J, DiGirolamo M, et al. Weight controland risk factor reduction in obese subjects treated for 2 years withorlistat: a randomized controlled trial. JAMA. 1999;281:235–42.
Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2008. Obes Surg. 2009;19:1605–11.
NIH. NIH conference. Gastrointestinal surgery for severe obesity. Ann Intern Med. 1991;115:956–61.
Obesity Education Initiative Expert Panel on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults, National Heart, Lung, and Blood Institute. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—the evidence report. September 1998. NIH report 98-4083. http://www.nhlbi.nih.gov/guidelines/obesity/ob_gdlnspdf. Accessed 31 Mar 2016.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis [published correction appears in JAMA. 2005;293(14):1728]. JAMA. 2004;292(14):1724–37.
Himpens J, Cadiere GB, Bazi M, et al. Long-term outcomes of laparoscopic adjustable gastric banding. Arch Surg. 2011;146(7):802–7.
Spivak H, Abdelmelek MF, Beltran OR, et al. Long-term outcomes of laparoscopic adjustable gastric banding and laparoscopic Roux-en-Y gastric bypass in the United States. Surg Endosc. 2012;26(7):1909–19.
Khwaja HA, Bonanomi G. Bariatric surgery: techniques, outcomes and complications. Curr Anaesth Crit Care. 2010;21:13–38.
Hutter MM, Schirmer BD, Jones DB, et al. First report from the American College of Surgeons–Bariatric Surgery Center Network: laparoscopic sleeve gastrectomy has morbidity and effectiveness positioned between the band and the bypass. Ann Surg. 2011;254(3):410.
Angrisani L, Lorenzo M, Borelli V. Laparoscopic adjustable gastric banding versus Roux-en-Y gastric bypass: 5-year results of a prospective randomized trial. Surg Obes Relat Dis. 2007;3(2):127–32.
Angrisani L, Cutolo PP, Formisano G, et al. Laparoscopic adjustable gastric banding versus Roux-en-Y gastric bypass: 10-year results of a prospective, randomized trial. Surg Obes Relat Dis. 2013;9(3):405–13.
Lim DM, Taller J, Bertucci W, et al. Comparison of laparoscopic sleeve gastrectomy to laparoscopic Roux-en-Y gastric bypass for morbid obesity in a military institution. Surg Obes Relat Dis. 2014;10(2):269–76.
Gadiot RP, Biter LU, van Mil S, et al. Long-term results of laparoscopic sleeve gastrectomy for morbid obesity: 5 to 8-year results. Obesity Surg. 2017;27(1):59–63.2.
Osland E, Yunus RM, Khan S, et al. Late postoperative complications in laparoscopic sleeve gastrectomy (LVSG) versus laparoscopic Roux-en-Y gastric bypass (LRYGB): meta-analysis and systematic review. Surg Laparosc Endosc Percutan Tech. 2016;26(3):193–201.
Naef M, Mouton WG, Naef U, Kummer O, Muggli B, Wagner HE. Graft survival and complications after laparoscopic gastric banding for morbid obesity—lessons learned from a 12-year experience. Obesity Surg. 2010;20(9):1206–1214
Klebanoff MJ, Chhatwal J, Nudel JD, Corey KE, Kaplan LM, Hur C. Cost-effectiveness of bariatric surgery in adolescents with obesity. JAMA surgery. 2017;152(2):136–141.
Salem L, Devlin A, Sullivan SD, et al. Cost-effectiveness analysis of laparoscopic gastric bypass, adjustable gastric banding, and non-operative weight loss interventions. Surg Obes Relat Dis. 2008;4(1):26–32.
Tice JA, Karliner L, Walsh J, et al. Gastric banding or bypass? A systematic review comparing the two most popular bariatric procedures. Am J Med. 2008;121(10):885–93.
Himpens J, Cadière G, Bazi M, et al. Long-term outcomes of laparoscopic adjustable gastric banding. Arch Surg. 2011;146(7):802–7.
Agency for Health Care Research and Quality. Medical Expenditure Panel Survey. (2014). Accessed 10 Jan 2017: http://meps.ahrq.gov/mepsweb.
Sullivan PW, Ghushchyan V, Ben-Joseph RH. The effect of obesity and cardiometabolic risk factors on expenditures and productivity in the united states. Obesity. 2008;16(9):2155–62.
Danielsson P, Kowalski J, Ekblom Ö, et al. Response of severely obese children and adolescents to behavioral treatment. Arch Pediatr Adolesc Med. 2012;166(12):1103–8.
Gluck B, Movitz B, Jansma S, et al. Laparoscopic sleeve gastrectomy is a safe and effective bariatric procedure for the lower BMI (35.0–43.0 kg/m2) population. Obes Surg. 2011;21(8):1168–71.
US Bureau of Labor Statistics. CPI inflation calculator. http://www.bls.gov/data/inflation_calculator.htm. Accessed 15 Mar 2016.
Sullivan PW, Ghushchyan V. Mapping the EQ-5D index from the SF-12: US general population preferences in a nationally representative sample. Med Decis Mak. 2006;26(4):401–9.
Mooney CZ. Monte carlo simulation. Vol 116. 1st ed. Springfield: Sage Publications; 1997. p. 112.
Mäklin S, Malmivaara A, Linna M, et al. Cost–utility of bariatric surgery for morbid obesity in Finland. Br J Surg. 2011;98:1422–9.
Craig B, Tseng D. Cost-effectiveness of gastric bypass for severe obesity. Am J Med. 2002;113:491–8.
Li JF, Lai DD, Ni B, et al. Comparison of laparoscopic Roux-en-Y gastric bypass with laparoscopic sleeve gastrectomy for morbid obesity or type 2 diabetes mellitus: a meta-analysis of randomized controlled trials. Can J Surg. 2013;56(6):E158–E164.24.
Faria GR, Preto JR, Costa-Maia J. Gastric bypass is a cost-saving procedure: results from a comprehensive Markov model. Obes Surg. 2013;23:460–6.
Langer FB, Reza Hoda MA, Bohdjalian A, et al. Sleeve gastrectomy and gastric banding: effects on plasma ghrelin levels. Obes Surg. 2005;15(7):1024–9.
Schauer PR, Kashyap SR, Wolski K, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366(17):1567–76.
Castilla I, Mar J, Valcárcel-Nazco C, et al. Cost–utility analysis of gastric bypass for severely obese patients in Spain. Obes Surg. 2014;24:2061–8.
Christ N, Sampalis J, Liberman M, et al. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg. 2004;3:416–4123.
Karlsson J, Taft C, Rydén A, et al. Ten-year trends in health-related quality of life after surgical and conventional treatment for severe obesity: the SOS intervention study. Int J Obes. 2007;31(8):1248–61.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Ethical Approval
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Alsumali, A., Eguale, T., Bairdain, S. et al. Cost-Effectiveness Analysis of Bariatric Surgery for Morbid Obesity. OBES SURG 28, 2203–2214 (2018). https://doi.org/10.1007/s11695-017-3100-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-3100-0