Abstract
Introduction
Bariatric surgery patients are at high risk for venous thromboembolism (VTE), and chemoprophylaxis is recommended.
Methods
Sheikh Khalifa Medical City (SKMC) is an American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) member since 2009. We report the rates of VTE in bariatric surgery patients from 2010 to 2016 compared to ACS NSQIP bariatric surgery programs before and after switching from heparin to low molecular weight heparin (LMWH), initiating mandatory risk assessment using Caprini scoring for VTE and adopting an aggressive strategy for high-risk patients regarding dosage of LMWH and chemoprophylaxis after discharge.
Results
During the study period, there were 1152 cases (laparoscopic Roux-en-Y gastric bypass (LRYGB) 625 and laparoscopic sleeve gastrectomy (LSG) 527) at Bariatric & Metabolic Institute (BMI) Abu Dhabi compared to 65,693 cases (LRYGB 32,130 and LSG 33,563) at ACS NSQIP bariatric surgery programs. VTE rates remained stable at ACS NSQIP bariatric surgery programs from 2010 to 2016 (0.45, 0.45, 0.45, 0.25, 0.35, 0.3, and 0.3%). In contrast, VTE rates at BMI Abu Dhabi decreased from 2.2% in 2011 to 0.35% after we adopted an aggressive strategy to VTE without an increase in bleeding complications. LRYGB patients with VTE had higher OR time, leak, collection, and mortality at ACS NSQIP hospitals compared to those at BMI Abu Dhabi. In contrast, rates were similar in LSG patients with VTE.
Conclusion
Changing our approach to VTE management led our VTE rates to decrease and become like those of ACS NSQIP bariatric surgery patients in LSG and LRYGB.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients undergoing bariatric surgery are considered high risk for venous thromboembolism (VTE), and the use of chemoprophylaxis is recommended in the peri-operative period [1,2,3,4]. In addition, some bariatric surgery patients are considered higher risk for VTE than others [5]. Furthermore, 80% of bariatric surgery patients develop VTE after discharge from the hospital [5]. Hence, using a fixed dose of VTE chemoprophylaxis for all bariatric surgery patients is not the best strategy [5]. In addition, there is a need to identify bariatric surgery patients who need extended prophylaxis after discharge [5]. We aim to compare the rates of VTE in our bariatric surgery patients at the Bariatric & Metabolic Institute (BMI) Abu Dhabi compared to those of the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) before and after we implemented mandatory risk assessment for VTE for patients undergoing bariatric surgery, and we changed our chemoprophylaxis in the hospital and after discharge.
Methods
Sheikh Khalifa Medical City (SKMC) is a tertiary care hospital and a member of the ACS NSQIP as a multi-specialty program since August 2009. ACS NSQIP is a risk-adjusted clinical registry that includes more than 600 hospitals in the USA, 48 hospitals in Canada, and 9 hospitals in the Middle East region (Lebanon, United Arab Emirates, Kingdom of Saudi Arabia, and Jordan). One of the requirements of ACS NSQIP for all participating hospitals is to obtain a 30-day follow-up in more than 80% of patients enrolled (https://www.facs.org/quality-programs/acs-nsqip). In addition, ACS NSQIP requires an independent surgical clinical reviewer to randomly select surgical cases for submission to the ACS NSQIP database. In 2010, our rates of VTE after surgery were higher compared to those of the ACS NSQIP hospitals. In response, we initiated a task force and implemented mandatory risk assessment for VTE at the time of admission to the hospital and this was added to the electronic medical record [6].
The Definition of VTE
All the ACS NSQIP sites use the same definition of VTE. The definition of VTE per the ACS NSQIP manual chapter 4 version of 2015 is “any venous New diagnosis of blood clot or thrombus within the venous system (superficial or deep) which may be coupled with inflammation and requires treatment. Criteria: Must be noted within 30 days after the principal operative procedure AND one of the following A or B below:
A. New Diagnosis of a [new] venous thrombosis (superficial or deep), confirmed by a duplex, venogram, CT scan, or any other definitive imaging modality (including direct pathology examination such as autopsy) AND the patient must be treated with anticoagulation therapy and/or placement of a vena cava filter or clipping of the vena cava, or the record indicates that treatment was warranted but there was no additional appropriate treatment option available. OR B. As per (A) above, but the patient or decision maker has refused treatment. There must be documentation in the medical record of the [patient’s] refusal of treatment.” [7]
Chemoprophylaxis for VTE
In 2012, we changed our management of VTE prophylaxis as follows: first, we started mandatory risk assessment of all bariatric surgery patients on admission (laparoscopic sleeve gastrectomy (LSG) and laparoscopic Roux-en-Y gastric bypass (LRYGB)). In addition, we switched from unfractionated heparin (UFH) three times a day to low molecular weight heparin (LMWH) twice a day. Furthermore, we initiated an aggressive strategy to identify high-risk patients, started them on a higher rate of LMWH, and sent them on LMWH for 2 weeks after discharge from the hospital. We used the Caprini risk scoring system for VTE risk assessment on admission as part of the electronic medical record (EMR) [6]. Patients are stratified as mild risk (Caprini score of 3 or less), moderate risk (Caprini score of 4), high risk (Caprini score of 5–6), and highest risk (Caprini score of more than 6) for VTE. All patients undergoing bariatric surgery receive sequential compression devices knee length and 5000 IU of UFH subcutaneously at the time of induction of anesthesia. In addition, they receive 40 mg of LMWH twice a day starting 8 h after the dose of UFH. Furthermore, all patients with a Caprini score of 5 or more receive the same dose of LMWH for 2 weeks after discharge. For patients with a Caprini score of more than 6, we place them on LMWH 60 twice a day and we measure their antifactor Xa 4 h after the third dose of LMWH.
All patients are ambulated within 2 h of surgery; they are assisted initially and then are on their own. We do not place urinary catheters, nasogastric tubes, or drains routinely as part of our enhanced recovery after the bariatric surgery program. In addition, patients are started on clear liquids as soon as they are awake and alert.
Using the ACS NSQIP prospective online database, we queried the database for bariatric surgery codes for (laparoscopic sleeve gastrectomy (LSG) 43775 and laparoscopic Roux-en-Y gastric bypass (LRYGB) 43644, 43645) for all hospitals with > 500 beds. We compared pre-operative demographics and intra-operative variables as well as outcomes of LSG and LRYGB performed at SKMC compared to those of ACS NSQIP bariatric surgery programs. Our primary outcome was the rate of VTE over time. Our secondary outcomes were operating room time, leak (sepsis and septic shock), collection, blood transfusion, and mortality.
We have described our technique of LRYGB and LSG previously [8]. In summary, we perform an ante-colic ante-gastric hand-sewn Roux-en-Y gastric bypass and we perform our LSG over a 32-Fr endoscope and over-sew the entire suture line in Lambert fashion and perform intra-operative endoscopy at the end of LRYGB and LSG in all cases.
Results
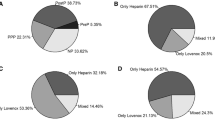
The total number of bariatric surgeries (LRYGB and LSG) done at BMI Abu Dhabi from January 2010 to December 2016 was 1152 cases (LRYGB 625 and LSG 527) compared to 65,693 cases (LRYGB 32,130 and LSG 33,563) at ACS NSQIP bariatric surgery programs. The rate of VTE in bariatric surgery patients at BMI Abu Dhabi from 2010 to 2016 was 0.8% (LRYGB 5/625 (0.8%) and LSG 4/527 (0.8%)) compared to 0.35% at ACS NSQIP bariatric surgery programs (LRYGB 98/32,032 (0.3%) and LSG 127/33,436 (0.4%)). While VTE rates remained stable at ACS NSQIP bariatric surgery programs, VTE rates at BMI Abu Dhabi decreased over time from a high of 2.2% in 2011 and stabilized at 0.35% in 2016 (0, 2.2, 0.9, 0.5, 0.95, 0.4, and 0.35%) (Fig. 1). The rate of bleeding complications at BMI Abu Dhabi was similar to that of ACS NSQIP hospitals during the entire study (Tables 1 and 3).
Demographics and Outcomes of VTE Patients After LRYGB and LSG at BMI Abu Dhabi Compared to Those of ACS NSQIP Bariatric Surgery Programs
Patients with VTE after LRYGB and LSG at BMI Abu Dhabi were younger and healthier with less co-morbidities, lower ASA scores, and less risk factors compared to patients with VTE after LRYGB and LSG in ACS NSQIP hospitals.
After LRYGB at BMI Abu Dhabi, our OR time, rates of pulmonary embolism, UTI, acute renal failure, sepsis, septic shock, intra-abdominal collections, and mortality were lower than those of patients with VTE after LRYGB in ACS NSQIP hospitals (Table 2).
After LSG at BMI Abu Dhabi, our rates of pulmonary embolism, UTI, acute renal failure, sepsis, septic shock, and intra-abdominal collections were lower than those of patients with VTE after LRYGB in ACS NSQIP hospitals. We had longer OR time and similar mortality to those of VTE patients after LSG in ACS NSQIP hospitals (Table 4).
Discussion
VTE rates at BMI Abu Dhabi after LRYGB and LSG decreased over time and became like the VTE rates at ACS NSQIP bariatric surgery programs after we implemented several changes to our approach to VTE without an increase in our rate of bleeding complications (Fig. 1). The first change was to switch from UFH three times a day to LMWH twice a day. Similarly, Birkmeyer et al. have shown that LMWH is more effective than UFH for prevention of VTE in bariatric surgery patients without an increased rate of bleeding [9]. Likewise, we did not encounter an increased rate of bleeding with this change in VTE chemoprophylaxis. We had one patient with VTE after LSG that needed blood transfusion. However, our overall rate of bleeding after LSG and LRYGB remained the same.
The second change was implementing mandatory VTE risk assessment to all patients as part of the electronic medical record. Similarly, we have observed a reduction in VTE rates in our surgery institute (General Surgery, Vascular Surgery, Orthopedics, and Neurosurgery) after we implemented mandatory risk assessment for surgery patients and using the Caprini risk assessment tool [6].
The third change was to send high-risk patients (Caprini score more than 5) home on LMWH twice a day for 2 weeks. This strategy of risk stratifying patients into moderate, high risk, and highest risk allows for identification of patients who need a higher dose of LMWH or need to go home on chemoprophylaxis. Likewise, Pannucci et al., Gupta et al., Caprini et al., Scarborough et al., and Merkow et al. have used other risk stratification models to identify high-risk patients for VTE [10,11,12,13,14,15]. Furthermore, Aminian et al. have shown that 80% of VTE occur after discharge and that it is important to risk stratify bariatric surgery patients into moderate, high, and highest risk and have a plan for chemoprophylaxis for VTE after discharge from the hospital [5].
The final change was to place patients with the highest risk for VTE (Caprini score more than 6) on a higher dose of LMWH (60 mg twice a day) and to measure antifactor Xa after the third dose to guide the dose at the time of discharge. We use an antifactor Xa target of 0.2–0.4 IU/ml to guide our LMWH dose in these patients. Similarly, Aminian et al., Borkgren-Okonek et al., and Nutescu et al. have found that measuring antifactor Xa, a useful adjunct for patients at the highest risk for VTE (previous VTE, wheelchair-bound patients, extreme BMI, etc.) or patients with renal dysfunction, is useful to guide the dose of chemoprophylaxis for VTE [5, 16, 17].
The rate for VTE after bariatric surgery in the study of 91,963 patients who underwent bariatric surgery at ACS NSQIP hospitals by Aminian et al. was found to be 0.29% [5]. The rates of VTE in the ACS NSQIP bariatric surgery programs were less than 0.45% throughout the study period (2010–2016). Our VTE rates at BMI Abu Dhabi steadily decreased and became less than 0.45% in 2015 for the first time.
LRYGB and LSG patients at BMI Abu Dhabi were younger and healthier with less co-morbidities, lower ASA scores, and less risk factors compared to LRYGB and LSG patients in ACS NSQIP hospitals. When comparing our outcomes after LRYGB at BMI Abu Dhabi to those of ACS NSQIP bariatric surgery programs, our OR time, re-operation, pulmonary embolism, UTI, acute renal failure, sepsis, septic shock, intra-abdominal collections, and mortality were lower. In contrast, we had a similar rate of blood transfusion and a higher rate of re-admission compared to ACS NSQIP hospitals (Table 1).
Similarly, when comparing our outcomes after LSG at BMI Abu Dhabi to those of ACS NSQIP bariatric surgery programs, our re-admission, re-operation, pulmonary embolism, acute renal failure, sepsis, septic shock, intra-abdominal collections, and mortality were lower. In contrast, we had a similar rate of blood transfusion, a higher rate of UTI, and longer OR time compared to ACS NSQIP hospitals (Table 3).
Despite our entire cohort of LRYGB and LSG being younger and healthier than LRYGB and LSG patients who had surgery in ACS NSQIP hospitals, our rates of peri-operative complications after LRYGB and LSG were either similar to or lower than those of ACS NSQIP hospitals. In addition, an aggressive strategy towards identifying patients with high risk for VTE and escalating chemoprophylaxis for these high-risk patients led to lower rates of VTE without an increase in the rate of bleeding complications (Tables 1 and 3).
Similarly, patients who developed VTE after LRYGB at BMI Abu Dhabi were younger and had shorter operative times, lower leak rates (lower sepsis, collection, and septic shock), lower rates of complications (UTI, acute renal failure, and pulmonary embolism), and lower mortality compared to patients who developed VTE after LRYGB at ACS NSQIP bariatric surgery programs (Table 2). These findings are similar to those of a previous comparative study we published in 2013 comparing bariatric surgery outcomes from BMI Abu Dhabi to those of ACS NSQIP bariatric surgery programs. In the 2013 comparative study, BMI Abu Dhabi patients were younger and had a lower leak rate (sepsis, septic shock) and lower mortality compared to patients from ACS NSQIP bariatric surgery programs [8]. Nevertheless, these findings should be interpreted with caution since the two groups in both studies were not matched and patients who developed VTE at ACS NSQIP hospitals after LRYGB were older, had a higher BMI, were more likely to be males, and have diabetes, hypertension, and an ASA score of 3 compared to 2 at BMI Abu Dhabi.
Similarly, patients who developed VTE after LSG at ACS NSQIP hospitals had higher rates of leak (sepsis collection and septic shock) compared to patients who developed VTE after LSG at BMI Abu Dhabi (Table 4).
Our study has several limitations, despite the large number of cases and random sampling of cases employed in the ACS NSQIP database because the two cohorts are not matched. In addition, our bariatric surgery patients were different in their pre-operative demographics compared to ACS NSQIP bariatric surgery patients. Furthermore, the improvement in our VTE rates could have been due to other cases.
Conclusion
Our VTE rates decreased after we implemented several changes to our VTE chemoprophylaxis protocol and became similar to ACS NSQIP VTE rates without an increase in bleeding complications. We believe an active strategy to risk stratify the risk of VTE in bariatric surgery patients is warranted.
References
American Society for Metabolic and Bariatric Surgery Clinical Issues Committee ASMBS updated position statement on prophylactic measures to reduce the risk of venous thromboembolism in bariatric surgery patients. Surg Obes Relat Dis. 2013 Jul-Aug;9(4):493–7. doi: https://doi.org/10.1016/j.soard.2013.03.006.
Winegar DA, Sherif B, Pate V, et al. Venous thromboembolism after bariatric surgery performed by Bariatric Surgery Center of Excellence Participants: analysis of the bariatric outcomes longitudinal database. Surg Obes Relat Dis. 2011;7:181–8.
Becattini C, Agnelli G, Manina G, et al. Venous thromboembolism after laparoscopic bariatric surgery for morbid obesity: clinical burden and prevention. Surg Obes Relat Dis. 2012;8:108–15.
Finks JF, English WJ, Carlin AM, et al. Predicting risk for venous thromboembolism with bariatric surgery: results from the Michigan Bariatric Surgery Collaborative. Ann Surg. 255:1100–4.
Aminian A, Andalib A, Khorgami Z, et al. Who should get extended thromboprophylaxis after bariatric surgery?: a risk assessment tool to guide indications for post-discharge pharmacoprophylaxis. Ann Surg. 2017 Jan;265(1):143–50. https://doi.org/10.1097/SLA.0000000000001686.
Nimeri AA, Gamaleldin MM, McKenna KL, Turrin NP, Mustafa BO. Reduction of venous thromboembolism in surgical patients using a mandatory risk-scoring system: 5-year follow-up of an American College of Surgeons National Surgical Quality Improvement Program. Clin Appl Thromb Hemost. 2015 Nov 25. pii:
(ACS NSQIP Operational Manual 2015 chapter 4 page 123) www.acsnsqip.org
Nimeri A, Mohamed A, El Hassan E, et al. Are results of bariatric surgery different in the Middle East? Early experience of an international bariatric surgery program and an ACS NSQIP outcomes comparison. J Am Coll Surg. 2013;216(6):1082–8. https://doi.org/10.1016/j.jamcollsurg.2013.01.063.
Birkmeyer NJO, Finks JF, Carlin AM, et al. Comparative effectiveness of unfractionated and low-molecular-weight heparin for prevention of venous thromboembolism following bariatric surgery. Arch Surg. 2012;147(11):994–8.
Pannucci CJ, Shanks A, Moote MJ, et al. Identifying patients at high risk for venous thromboembolism requiring treatment after outpatient surgery. Ann Surg. 2012;255:1093–9.
Gupta PK, Franck C, Miller WJ, et al. Development and validation of a bariatric surgery morbidity risk calculator using the prospective, multicenter NSQIP dataset. J Am Coll Surg. 2011;212:301–9.
Caprini JA. Thrombosis risk assessment as a guide to quality patient care. Dis Mon. 2005;51:70–8.
Pannucci CJ, Laird S, Dimick JB, et al. A validated risk model to predict 90- day VTE events in postsurgical patients. Chest. 2014;145:567–73.
Scarborough JE, Cox MW, Mureebe L, et al. A novel scoring system for predicting postoperative venous thromboembolic complications in patients after open aortic surgery. J Am Coll Surg. 2012;214:620–6. discussion 627-8
Merkow RP, Bilimoria KY, McCarter MD, et al. Post-discharge venous thromboembolism after cancer surgery: extending the case for extended prophylaxis. Ann Surg. 2011;254:131–7.
Borkgren-Okonek MJ, Hart RW, Pantano JE, et al. Enoxaparin thromboprophylaxis in gastric bypass patients: extended duration, dose stratification, and antifactor Xa activity. Surg Obes Relat Dis. 2008;4:625–31.
Nutescu EA, Spinler SA, Wittkowsky A, et al. Low-molecular-weight heparins in renal impairment and obesity: available evidence and clinical practice recommendations across medical and surgical settings. Ann Pharmacother. 2009;43:1064–83.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
This article does not contain any studies with human participants or animals performed by any of the authors. For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Nimeri, A.A., Bautista, J., Ibrahim, M. et al. Mandatory Risk Assessment Reduces Venous Thromboembolism in Bariatric Surgery Patients. OBES SURG 28, 541–547 (2018). https://doi.org/10.1007/s11695-017-2909-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2909-x