Abstract
Background
Although considered a common bariatric procedure, laparoscopic adjustable gastric banding (LAGB) is associated with high rates of weight loss failure and long-term complications.
Purpose
The purpose of this study was to re-assess the safety and outcome of conversion of failed LAGB to laparoscopic sleeve gastrectomy (LSG).
Materials and Methods
One hundred and nine patients underwent conversion from LAGB to LSG (78 females, mean age 43 ± 11.3 years, mean BMI 42.4 ± 7.4 kg/m2). Patient demographics, obesity-related co-morbidities, BMI before and after the procedure, post-operative complications, and length of hospital stay were documented.
Results
All cases were completed laproscopically, with 88% (n = 96) performed in a single stage. Fourteen patients developed early post-operative complications (12.8%), including two leaks and three post-operative bleeding. There were no mortalities in this series. Average BMI at least 1-year following surgery was 33 ± 5.3 kg/m2 (excess weight loss (EWL) = 53.7%).
Conclusions
Our data suggests that conversion of failed LAGB to LSG is both safe and effective. Randomized controlled studies comparing conversion of a failed LAGB to sleeve gastrectomy versus other bariatric operations are necessary to clarify the optimal conversion procedure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery remains the most effective treatment leading to substantial long-term weight loss, improvement or resolution of co-morbidities, and even reduced mortality rates [1–3]. Laparoscopic adjustable gastric banding (LAGB) is the least invasive bariatric procedure involving the engagement of an inflatable band device around the proximal stomach to modulate the amount of food intake. At first, LAGB gained popularity due to perception of reversibility, significant and rapid weight loss, resolution of co-morbidities and low operative morbidity rates [4, 5]. However, prolonged follow-up revealed unsatisfactory weight loss in approximately 30–50% of cases. Additionally, complications such as band slippage, erosion, and pouch or esophageal dilatation necessitated revision in up to 20% of patients [6–9]. Although safe, re-banding demonstrated poor results in terms of further weight loss following surgery. Hence, the demand for other bariatric surgeries as a revision to failed LAGB is continuously increasing [10, 11].
Although revisional surgery poses a greater surgical challenge and is associated with increased complication rates compared to primary bariatric surgery [12], a number of bariatric procedures were shown to be safe and effective following failed LAGB. These include laparoscopic Roux-en-Y gastric bypass (RYGB), biliopancreatic diversion (BPD), duodenal switch (DS), and laparoscopic sleeve gastrectomy (LSG) [10, 13–16]. LSG consists of resecting the greater curvature of the stomach, forming a vertical sleeve of the residual stomach portion [17, 18]. Increasingly gaining popularity as a standalone operation, this procedure provides similar outcomes to gastric bypass with regard to weight loss and comorbidity improvement/resolution yet is less technically challenging [19, 20]. Recently, a number of studies examined the benefits of LSG as a revisional surgery following failed LAGB in comparison to RYGB [9, 21–23]. Nevertheless, the surgery of choice following removal of gastric banding is yet undetermined. In this study, we report a series of patients in whom LAGB was converted to LSG. The recent literature regarding LSG following failed LAGB is reviewed.
Patients and Methods
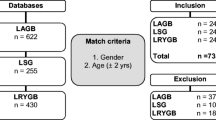
We retrospectively reviewed the charts of all patients who underwent conversion of a failed gastric band to a sleeve gastrectomy in the bariatric surgery unit of the Tel-Aviv Sourasky medical center between January 2008 and August 2013. Excluded from this study were patients under the age of 18, those who underwent surgery due to acute LAGB complications, and patients who underwent band removal with no primary intent for LSG at the time of band removal surgery. Patient demographics, obesity-related co-morbidities, body mass index (BMI) before and after the procedure, post-operative complications, and length of hospital stay were documented. This study was approved by the Tel-Aviv Sourasky Medical Center institutional review board (IRB).
Surgical Technique
The operation was performed under general anesthesia in a supine position with the table in reverse Trendelenburg. Intravenous cephalosporin and a prophylactic dose of heparin were administered prior to incision. An orogastric tube was used and the stomach was decompressed. A supraumbilical Veress needle was inserted with insufflation of the abdominal cavity to a pressure of 15 mmHg. Five laparoscopic ports were inserted. The band was then transected and removed; fundal adhesions to the left diaphragm were lysed and the gastro-gastric plication taken down to completely mobilize the stomach and prevent leaving a large gastric pouch at the level of the gastroesophageal junction. The short gastric vessels were taken down along the greater curvature of the stomach with a Harmonic® scalpel (Ethicon Endo-Surgery, Inc.) or a ligasure® (Covidien, Inc.). Dissection started 4 cm proximal to the pylorus, extending cephalad and taking the adhesions down around the fundus of the stomach. Once mobilized, a bougie was inserted following the lesser curvature. The bougie size, 32–36 Fr, was a surgeons’ preference. Once the bougie tube was placed, sequential firings of the stapler (Covidien tri-stapler or J&J Echelon), were used to transect the lateral stomach, creating a vertical sleeve gastrectomy.
Statistical Analysis
The probability that variances in categorical parameters between the groups are significantly different was calculated using Fischer test. Parametric data are presented as mean ± standard deviation (SD), and statistical analysis was performed using Student’s t test.
Results
One hundred and nine patients underwent revision of a failed LAGB to a LSG. There were 78 females (71.5%), with a mean age of 43 ± 11.3 years and a mean BMI of 42.4 ± 7.4 kg/m2. The mean time interval from LAGB surgery was 8.5 ± 3.6 years. Patient demographics including their co-morbidities are summarized in Table 1.
LAGB failed for different reasons—some patients presented with hardware failure, others failed to lose weight or presented with weight regain, and some were unhappy with their quality of life.
Ninety-six patients (88%) underwent a one-stage conversion, while the remaining 13 patients underwent a staged approach with the band being removed in the primary procedure and the sleeve gastrectomy performed several months later (average 8.7 ± 4.3 months) In 2 patients of the one-stage group, a hiatal hernia was identified and primarily repaired during surgery.
Fourteen patients (12.8%) developed early (within 30 days) post-operative complications (Clavien-Dindo classification, grades 1 and 3b). These included a sleeve stricture, 2 leaks (1.8%), 3 post-operative bleeding (2.8%), 4 intra-abdominal collections (3.7%), and 4 hematomas (3.7%) (Table 2). All post-operative complication occurred in patients that underwent a one-step procedure. Early re-operation was necessary in four patients (3.7%) that underwent a one-stage conversion. Indications for re-operation included post-operative hemorrhage in three patients, and stenosis of the sleeve necessitating conversion to gastric bypass in one patient.
The overall average length of stay was 5.4 ± 5.95 days. The average length of stay of patients that underwent one-step procedure and those that had a two-step revision was 5.6 ± 6.2 and 3.76 ± 2, respectively (P = 0.29).
Within 2 years from surgery, seven patients underwent conversion to gastric bypass (Table 2). Indications for conversion to gastric bypass included weight regain in five patients, and dysphagia due to sleeve stricture not amenable to endoscopic dilatations in two patients.
The overall average BMI at least 1-year following surgery was 33.03 ± 5.3 kg/m2 (preoperative mean BMI 42.4 ± 7.4 kg/m2, excess weight loss (EWL) = 53.7%, Total weight loss = 22.64%). Mean EWL was 53.0 and 58.3% for patients that underwent one-step and two-step procedures, respectively, 1-year following surgery.
Discussion
Although LAGB remains a popular bariatric surgery, relatively high rates of weight loss failure and long-term complications are reported [6–8, 24]. Here, we assessed the safety and effectiveness of LSG as a revision surgery in patients in whom the LAGB results were unsatisfactory. One-stage conversion was performed in the majority of patients. Patients in this series had significantly higher rates of post-operative complications, increased length of hospital stay, and 30-day re-operations when compared to published data in large series of primary sleeve gastrectomy.
Several studies addressed the benefits and drawbacks of LSG as a conversion to failed LAGB (Table 3). Post-operative complications in the presented series, mainly consisting of bleeding and hematoma formation, leak, and abdominal collections, were assessed in accordance with the Clavien-Dindo classification [25]. Large variations in rates and classification of post-operative complication are found among previously published studies (Table 3). Noel et al. (2014) [21] reported a total post-operative complication rate of 4.5% in the primary LSG group and 2% in the LAGB to LSG group. This stands in contrast to our data both in rates of complications, which may be attributed to differences in classification, and in trends between groups. Nevertheless, rates of 1–2% leaks with no differences between groups were similarly demonstrated in both studies (Table 3). Trends for increased complications in the conversion group was also reported by Guetta et al. 2015 [26] with similar rates of total complications as in the presented study. Other groups demonstrated results ranging from 2% to over 10% post-operative complications in various degrees of severity (Table 3). Of note, major complication, including leak, abdominal collections, and hematoma, as well as rates of re-operations were comparable between all studies (Table 3). Our data is consistent with the observation that surgeries performed on a previously operated stomach lead to increased risk of complications. Moreover, Guetta et al. 2015 [26] showed that the risk for early major complication is doubled with each additional previous bariatric surgery performed before the current LSG. This can be attributed to technical difficulties in performing the operation due to adhesions etc., as well as the effect of the gastric banding on the healing of the stomach following LSG. This trend was also reflected by the increased rate of early re-operations. The length of hospital stay ranged from 2 days, as reported by Khoursheed et al. 2013 [27], to almost 6 days, as was reported by Goitein et al. 2011 [28]. In our series, length of stay was within this range, reflecting either increased rates of post-operative complications or an increased concern from their development.
On the survey on LSG at the fourth international consensus summit on sleeve gastrectomy, the EWL was 59.3 at year 1, 59% at year 2, 54.7% at year 3, and 52.3% at year 4 [29]. Similar percentages were demonstrated in other large cohort studies [9, 21, 30]. In our series, the EWL was 53.7%. Noel et al. (2014) [21] reported that in a large series consisting of 300 conversions and 1060 primary LSG, the EWL was 62.2% ± 22.2 at a mean interval of 35 ± 24 months, and 75.9% ± 21.4 at a mean interval of 29 ± 19.8 months, respectively. The tendency of decreased weight loss following revisional LSG might be attributed to their inability to maintain dietary discipline, resulting in repetitive failures of restrictive procedures. Additionally, it is possible that yet unknown genetic characteristics contribute to decreased effectiveness of restrictive surgery. Finally, optimal mobilization of the stomach fundus enabling for its complete removal is a crucial part of the LSG for optimal outcomes. Adhesions around the band involving the gastric fundus and the left crus may sometimes limit mobilization resulting in sub-optimal fundus removal thus contributing to lesser outcomes. The increased failure rates in these patients are also reflected by the fact that 6.4% of them required a second conversion to a gastric bypass (Table 2).
The majority of our cohort underwent a single-stage procedure, with only 13 patients in the 2-stage group. Although not statistically significant, it is worth mentioning that all complications and re-operations occurred in patients having a one-stage operation.
Despite a relatively large series, the presented study does not lack limitations and drawbacks. This is an observational retrospective study. The follow-up time is relatively short and lacks data regarding the long-term effect of surgery on preoperative co-morbidities. The procedures were performed by four different bariatric surgeons using different bougie sizes (32-36Fr), thus contributing to some expected bias in outcomes.
We believe that these issues and others should be addressed in a large prospective randomized study aiming to establish proper guidelines for revisional bariatric surgery.
Conclusion
Our data suggests that conversion of failed LAGB to LSG is both safe and effective.
A staged approach might be safer, with a small sub-group in our series showing no complications when the sleeve was performed several months after excising the Band. Randomized controlled studies comparing conversion of a failed LAGB to Sleeve gastrectomy versus other bariatric operations are necessary to clarify the optimal conversion procedure.
References
Christou NV, Sampalis JS, Liberman M, et al. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg. 2004;240:416–23. discussion 423-414
Adams TD, Gress RE, Smith SC, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357:753–61.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37.
Cunneen SA. Review of meta-analytic comparisons of bariatric surgery with a focus on laparoscopic adjustable gastric banding. Surg Obes Relat Dis. 2008;4:S47–55.
Favretti F, Segato G, Ashton D, et al. Laparoscopic adjustable gastric banding in 1,791 consecutive obese patients: 12-year results. Obes Surg. 2007;17:168–75.
Biertho L, Steffen R, Branson R, et al. Management of failed adjustable gastric banding. Surgery. 2005;137:33–41.
Suter M, Calmes JM, Paroz A, et al. A 10-year experience with laparoscopic gastric banding for morbid obesity: high long-term complication and failure rates. Obes Surg. 2006;16:829–35.
DeMaria EJ, Sugerman HJ, Meador JG, et al. High failure rate after laparoscopic adjustable silicone gastric banding for treatment of morbid obesity. Ann Surg. 2001;233:809–18.
Elnahas A, Graybiel K, Farrokhyar F, et al. Revisional surgery after failed laparoscopic adjustable gastric banding: a systematic review. Surg Endosc. 2013;27:740–5.
Weber M, Muller MK, Michel JM, et al. Laparoscopic Roux-en-Y gastric bypass, but not rebanding, should be proposed as rescue procedure for patients with failed laparoscopic gastric banding. Ann Surg. 2003;238:827–33. discussion 833-824
Jones Jr KB. Revisional bariatric surgery—potentially safe and effective. Surg Obes Relat Dis. 2005;1:599–603.
Hallowell PT, Stellato TA, Yao DA, et al. Should bariatric revisional surgery be avoided secondary to increased morbidity and mortality? Am J Surg. 2009;197:391–6.
Spivak H, Beltran OR, Slavchev P, et al. Laparoscopic revision from LAP-BAND to gastric bypass. Surg Endosc. 2007;21:1388–92.
van Wageningen B, Berends FJ, Van Ramshorst B, et al. Revision of failed laparoscopic adjustable gastric banding to Roux-en-Y gastric bypass. Obes Surg. 2006;16:137–41.
Topart P, Becouarn G, Ritz P. Biliopancreatic diversion with duodenal switch or gastric bypass for failed gastric banding: retrospective study from two institutions with preliminary results. Surg Obes Relat Dis. 2007;3:521–5.
Iannelli A, Schneck AS, Ragot E, et al. Laparoscopic sleeve gastrectomy as revisional procedure for failed gastric banding and vertical banded gastroplasty. Obes Surg. 2009;19:1216–20.
Gill RS, Switzer N, Driedger M, et al. Laparoscopic sleeve gastrectomy with staple line buttress reinforcement in 116 consecutive morbidly obese patients. Obes Surg. 2012;22:560–4.
Frezza EE. Laparoscopic vertical sleeve gastrectomy for morbid obesity. The future procedure of choice? Surg Today. 2007;37:275–81.
Sippey M, Kasten KR, Chapman WH. 30-day readmissions after sleeve gastrectomy versus Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2016; doi:10.1016/j.soard.2016.01.036.
Osland E, Yunus RM, Khan S, et al. Postoperative early major and minor complications in laparoscopic vertical sleeve gastrectomy (LVSG) versus laparoscopic Roux-en-Y gastric bypass (LRYGB) procedures: a meta-analysis and systematic review. Obes Surg. 2016; doi:10.1007/s11695-016-2101-8.
Noel P, Schneck AS, Nedelcu M, et al. Laparoscopic sleeve gastrectomy as a revisional procedure for failed gastric banding: lessons from 300 consecutive cases. Surg Obes Relat Dis. 2014;10:1116–22.
Marin-Perez P, Betancourt A, Lamota M, et al. Outcomes after laparoscopic conversion of failed adjustable gastric banding to sleeve gastrectomy or Roux-en-Y gastric bypass. Br J Surg. 2014;101:254–60.
Moon RC, Teixeira AF, Jawad MA. Conversion of failed laparoscopic adjustable gastric banding: sleeve gastrectomy or Roux-en-Y gastric bypass? Surg Obes Relat Dis. 2013;9:901–7.
O’Brien PE. Bariatric surgery: mechanisms, indications and outcomes. J Gastroenterol Hepatol. 2010;25:1358–65.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Guetta O, Ovnat A, Shaked G, et al. Analysis of morbidity data of 308 cases of laparoscopic sleeve gastrectomy—the Soroka experience. Obes Surg. 2015; doi:10.1007/s11695-015-1665-z.
Khoursheed M, Al-Bader I, Mouzannar A, et al. Sleeve gastrectomy or gastric bypass as revisional bariatric procedures: retrospective evaluation of outcomes. Surg Endosc. 2013;27:4277–83.
Goitein D, Feigin A, Segal-Lieberman G, et al. Laparoscopic sleeve gastrectomy as a revisional option after gastric band failure. Surg Endosc. 2011;25:2626–30.
Gagner M, Deitel M, Erickson AL, et al. Survey on laparoscopic sleeve gastrectomy (LSG) at the fourth international consensus summit on sleeve gastrectomy. Obes Surg. 2013;23:2013–7.
Yazbek T, Safa N, Denis R, et al. Laparoscopic sleeve gastrectomy (LSG)—a good bariatric option for failed laparoscopic adjustable gastric banding (LAGB): a review of 90 patients. Obes Surg. 2013;23:300–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors declare that they have no conflict of interest.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Pencovich, N., Lahat, G., Goldray, O. et al. Safety and Outcome of Laparoscopic Sleeve Gastrectomy Following Removal of Adjustable Gastric Banding: Lessons from 109 Patients in a Single Center and Review of the Literature. OBES SURG 27, 1266–1270 (2017). https://doi.org/10.1007/s11695-016-2463-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-016-2463-y