Abstract
Background
Roux-en-Y gastric bypass (RYGB) is an effective treatment for patients with type 2 diabetes mellitus (T2D) with obesity. However, T2D remission after surgery has not been adequately studied in Chinese patients with different obesity classes. The purpose of this study is to evaluate the medium-term metabolic results of RYGB in T2D patients with body mass index (BMI) >25 kg/m2 compared by obesity class.
Methods
We retrospectively divided 120 Chinese patients with T2D and BMI >25 kg/m2 into four groups from overweight to obesity class III and reviewed their medical records for metabolic outcomes 36 months after RYGB. T2D remission was defined as glycated hemoglobin <6.0 % and no current medications. Hypertension, dyslipidemia, cardiovascular risk, and medications were also evaluated.
Results
Sixty-two patients (62/120, 51.6 %) were female. All surgeries were performed laparoscopically without mortality or major complications. Mean follow-up duration was 38.7 ± 9.1 months and follow-up compliance was 86.7 %. Patients with BMI ≥28 kg/m2 benefitted more from weight loss following RYGB. Medication and remission results for hypertension and dyslipidemia did not differ significantly between groups. There was a significant reduction in the need for oral medication or insulin in all four groups. T2D remission occurred in 44–66.7 % of all patients at 36 months with no significant difference between groups. Initial BMI was correlated with A1C 36 months after surgery (r = −0.217, P = 0.027).
Conclusions
RYGB effectively treated T2D patients in our study, even in low-BMI patients, and resulted in diabetes remission and metabolic disorder control, reducing cardiovascular risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric and metabolic surgery is a successful treatment for type 2 diabetes mellitus (T2D) with Roux-en-Y gastric bypass (RYGB) being the most popular surgical procedure [1, 2]. Body mass index (BMI) is the most important index for obesity classification, and when elevated, it is also considered a key indication for bariatric and metabolic surgery for T2D treatment [3]. Recent statements from the Diabetic Surgery Summit indicate that surgery should be considered in T2D patients with BMI >35 kg/m2 or an optional choice for T2D patients with BMI 30–35 kg/m2 and major co-morbidities [4]. Evidence suggests that RYGB can lead to T2D remission, especially in morbidly obese patients. Lee and colleagues showed that elevated BMI could be a predictor of remission following bariatric surgery in T2D patients [5]. However, several other studies support RYGB’s efficacy in low- or even normal-BMI patients [6, 7]. Research shows that the most probable mechanism for the antidiabetic effects of bariatric surgery is related to changes in the release of gut hormones, which leads to improved insulin secretion and sensitivity, [8] rather than being related to weight loss or BMI.
In Asian populations, the definition of obesity includes a BMI ≥28 kg/m2. Most Chinese T2D patients have a BMI below 35 kg/m2 and impaired islet function during the early stages of the disease [9]. Our previous research indicated that T2D remission after metabolic surgery was influenced by several factors including T2D duration, BMI, and visceral fat area in Chinese patients [10]. Therefore, adopting a strictly BMI-based criterion for metabolic surgery may be inadequate for Chinese patients. Our study evaluated the results of T2D remission following RYGB in Chinese patients with elevated BMI, comparing different obesity class.
Materials and Methods
We retrospectively reviewed the medical records of 120 patients who met the inclusion criteria and who were treated between February 2011 and October 2013. The human research review board of our institution approved the study and all patients provided written informed consent.
Following the latest guidelines for metabolic surgery from the Chinese Society for Metabolic and Bariatric Surgery, the inclusion criteria were as follows: (1) T2D duration ≤15 years with adequate islet function defined as fasting C-peptide by the oral glucose tolerance test >1 ng/mL and a ratio of peak to fasting value >2 ng/mL; (2) age 16–65 years; and (3) BMI 25–27.5 kg/m2 with poorly controlled T2D and more than two symptoms of metabolic syndrome or T2D complications; and (4) BMI > 27.5 kg/m2 with poorly controlled T2D.
The laparoscopic gastric bypass procedure included a 25-mL gastric pouch, a 100–120-cm biliopancreatic limb, and a 100–120-cm alimentary limb; mesentery defects and Petersen’s place were closed at time of surgery [10].
Definitions of Obesity and Diabetes
The diagnosis of T2D was based on the 1999 WHO criteria: fasting plasma glucose ≥7.0 mmol/L and/or a 2-h plasma glucose ≥11.1 mmol/L.
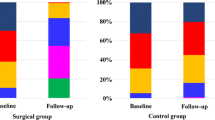
BMI was categorized according to Chinese standard guidelines [11] as follows: normal weight: BMI ≥18.5 kg/m2 and <24 kg/m2; overweight: BMI ≥24 kg/m2 and <28 kg/m2; obesity class I: BMI≥28 kg/m2 and <32 kg/m2; obesity class II: BMI ≥32 kg/m2 and <37 kg/m2; and obesity class III: BMI≥37 kg/m2 (Fig. 1).
Patients were divided into four groups: group I (G I): BMI ≥37 kg/m2; group II (G II): BMI ≥32 kg/m2 and <37 kg/m2; group III (G III): BMI ≥ 28 kg/m2 and <32 kg/m2; group IV (G IV): BMI >25 kg/m2 and <28 kg/m2.
Remission of Diabetes, Hypertension, and Dyslipidemia
Based on the 2015 outcome reporting standards for the ASMBS [12], diabetes complete remission was defined as glycated hemoglobin (A1C) level <6.0 % with a fasting glucose concentration <5.6 mmol/L for 1 year or more without active pharmacological intervention. Hypertension complete remission was defined as BP <120/80 mmHg without antihypertensive medication. Dyslipidemia remission was defined as normal lipid serum levels without medication.
Anthropometric Evaluations and Medical History
Anthropometric evaluations including weight, BMI, heart rate, blood pressure, body fat ratio, and waist and hip circumference were recorded before and after bypass surgery. Medical history and current medications for diabetes, hypertension, and dyslipidemia were also recorded.
Biochemical Examinations
Biochemical parameters were evaluated by obtaining serum samples after an overnight fast and included fasting glucose, postprandial glucose followed by an oral glucose tolerance test, fasting C-peptide, A1C, serum total cholesterol, triglyceride, high-density lipoprotein cholesterol and low-density lipoprotein cholesterol, and serum hypersensitive C-reactive protein (hsCRP) levels. Cardiovascular risk was calculated as the total cholesterol to high-density lipoprotein cholesterol ratio. Insulin resistance level and β-cell function were measured by the homeostasis model assessment of insulin resistance (HOMA-IR) using the formula, mIU/mmol/L2 = fasting insulin (mIU/L) × fasting glucose (mmol/L)/22.5, and the homeostasis model assessment of β-cell function (HOMA-β) using % = 20 × fasting insulin (mIU/L)/fasting glucose (mmol/L) − 3.5) (%).
Statistical Analysis
All statistics were calculated using SPSS statistical software (version 20.0; SPSS Inc., Armonk, NY, USA). Continuous variables in the different groups were tested for normal distribution using the Kruskal–Wallis normality test. The one-way analysis of variance test was used to compare variables before and after the study. Contingency tables of categorical variables were analyzed by the Kruskal–Wallis test. Data are presented as the mean ± SD or median [interquartile range (IQR)]. Correlations between the initial various variables and A1C parameters 36 months after surgery were analyzed using Pearson’s correlation test. Parameters that might influence the effect of RYGB surgery on A1C were evaluated by linear regression analysis. Post-hoc power analysis was performed in 12 months. Statistical significance was defined as P < 0.05.
Results
Patients
There were 120 patients involved in this study and 62 (51.6 %) were female. All surgeries were performed under laparoscopy without mortality or major complications. No severe malnutrition or vitamin or mineral deficiencies were observed during follow-up with two cases of intestinal obstruction. One case at 2 weeks after surgery was diagnosed with adhesion by CT scan while another one at 6 months after surgery was with over-eating history, both relieved by conservative treatment as fast and gastrointestinal decompression for 1 week. The mean follow-up duration was 38.7 ± 9.1 months and follow-up compliance was 86.7 % at 36 months. Baseline characteristics are shown in Table 1. Systolic and diastolic blood pressure in group I patients were significantly higher than in the other groups.
Glycemic Control
There was a significant reduction in oral medication or insulin used for glycemic control in all four groups (Table 2). Diabetes complete remission results are shown in Table 2, and no significant difference was found among the four groups (P = 0.063). Furthermore, the T2D remission in each group between the 12 and 36 months follow-up showed no statistically significant. However, there was a relapse back into diabetes for 8.3, 14.2, 21.5, and 23.4 % within 2 years in groups I to IV separately.
Mean levels of A1C, fasting and postprandial glucose, fasting C-peptide and insulin levels, hsCRP, and HOMA-IR were significantly decreased at 12 and 36 months with no significant difference among the groups. HOMA-β level showed no significant change after surgery (Table 4). Changes in A1C are shown in Fig. 2 with no significant difference between the groups.
Weight Loss
At 12 months, body weight, BMI, waist and hip circumference, waist to hip ratio, and body fat ratio were significantly reduced compared with baseline (Table 3). Changes in body weight (P < 0.01) and BMI (P < 0.01) in group I were greater than in other groups (Fig. 1 and Table 3). The difference between the 12 and 36 months was not statistically significant (Table 3).
Blood Pressure
Blood pressure decreased significantly in Group II and Group III comparing values 12 months after surgery vs. baseline, respectively, as follows: in Group II (121.0 ± 12.3 vs. 132.1 ± 11.9, P < 0.01) and group III (119.6 ± 14.2 vs. 129.7 ± 11.6, P < 0.05). Comparing diastolic blood pressure 12 months after surgery vs. baseline, respectively, in group II (76.3 ± 9.1 vs. 83.7 ± 8.5, P < 0.01), group III (75.3 ± 10.1 vs. 81.0 ± 8.9, P < 0.05), and group IV (73.9 ± 8.1 vs. 80.7 ± 9.8, P < 0.05), values also decreased significantly.
Thirty-six months after surgery, systolic blood pressure in group II (114.7 ± 13.6 vs. 132.1 ± 11.9, P < 0.01) was significantly decreased, diastolic blood pressure in all groups, group I (72.7 ± 9.8 vs. 90.2 ± 16.4 (baseline), P < 0.05), group II (75.3 ± 9.5 vs. 83.7 ± 8.5, P < 0.01), group III (74.1 ± 4.6 vs. 81.0 ± 8.9 (baseline), P < 0.05), and group IV (78.9 ± 7.3 vs. 80.7 ± 9.8 (baseline), P < 0.05) were significantly decreased (Table 3).
Medication and remission results regarding hypertension are shown in Table 2. Thirty-six months after surgery, all patients were no longer taking antihypertensive medication. There was no significant difference between the four groups.
Dyslipidemia
Medication and remission results regarding dyslipidemia before and after surgery are shown in Table 2. At baseline, 6/6 (100 %) patients in group I, 23/30 (76.7 %) in Ggoup II, 11/13 (84.6 %) in group III, and 11/14 (78.6 %) in group IV experienced hypertriglyceridemia. All dyslipidemia patients were no longer taking medication as of 12 months after surgery. The serum lipid profiles before and after surgery are shown in Table 4. Cardiovascular risk scores decreased significantly in all groups after surgery (Table 2).
Baseline Parameters and Diabetes Remission
Table 5 shows the significantly parameters which correlated with A1C value 36 months after surgery. We compared the parameters between the remission and non-remission groups, and only the initial BMI was significantly different between the two groups (P = 0.043). Although A1C after surgery showed a downward trend according to increasing initial BMI, further linear regression analysis showed no significant result.
Post-Hoc Power Analysis
The retro-power results by post-hoc power analysis at 12 and 36 months after surgery, are shown in Tables 3 and 4. The observed power <0.7 suggested the risk of a type 2 error.
Discussion
The effectiveness of RYGB is well-known for resolving T2D combined with obesity. Currently, BMI is considered to be an important factor in T2D remission, and strong evidence supports metabolic surgery, especially RYGB, in morbidly obese T2D patients [13]. The surgical indications are based on BMI and several studies have reported positive surgical outcomes in patients with non-obese BMIs, supporting the efficacy of RYGB in overweight patients or even those with normal BMI [6, 7]. Huang and colleagues demonstrated that RYGB was well tolerated and feasible with good T2D remission rates in patients with BMI ranging from 25 to 35 kg/m2 [14].
In East Asia and especially China, the predominant factor for developing T2D in patients with low or normal BMI is β-cell dysfunction while insulin resistance is the predominant factor in obesity [9]. Most patients have central obesity rather than morbid obesity with a high BMI level, and the study of RYGB in different obesity grades may not only provide T2D remission data but also provide evidence for BMI-based patient selection and a deeper understanding of the surgical mechanisms leading to remission.
To the best of our knowledge, few studies have focused on RYGB results in Chinese T2D patients with different obesity classes. Our study group assignment was based on Chinese obesity guidelines, which differ slightly from the World Health Organization standards. The reason for choosing these guidelines is that the Chinese guidelines better represent Chinese patients’ obesity status. The latest surgical criteria from the Chinese Society for Metabolic and Bariatric Surgery are also based on these guidelines.
All patients achieved significant weight loss while avoiding malnutrition and excessive weight loss. Patients with baseline BMI <32 kg/m2 stabilized within their normal weight range and others in groups I and II reached the overweight standard. Our results showed that change in BMI increased with increased baseline BMI, which means that patients achieved greater weight loss following RYGB in higher BMI groups especially in BMI ≥37 kg/m2.
Previous studies have supported age, T2D duration, C-peptide levels (which indicate β-cell function) and initial BMI as predictors for T2D remission [5, 15, 16]. A recent controversial but interesting argument arose from surgical results in T2D patients with low BMI in Asia [14, 16]. After 12 months of follow-up, there was a significant improvement in DM status, including a significant reduction in the use of diabetes-related medications and insulin. Significant reduction in C-peptide levels, insulin, and HOMA-IR showed improved insulin resistance; however, there was no significant improvement in β-cell function based on the HOMA-%β result. Our current study showed no significant difference among the different BMI-grade patients regarding T2D remission, the need for T2D medication, or improved insulin resistance. On the other hand, the A1C after surgery, which represent a major factor for diabetes remission, showed a downward trend according to increasing initial BMI. This trend is not significant because of the small numbers in each group, further study with larger numbers of patients was necessary to confirm the role of initial BMI in diabetes remission. Our remission results were similar to those reported by Huang et al. [14] in patients with BMI 25–35 kg/m2, but higher than those reported by Malapan et al. [7] in non-obese T2D patients. Such discrepancies show the importance of appropriate patient selection in low-BMI T2D patients.
The T2D remission rate in our study decreased with rising A1C levels continuously to 36 months, although it showed no significant difference between 12 and 36 months. In contrast, the need for diabetes medications including insulin did not change after surgery over time. Observational studies have shown a similar decreasing remission rate in several middle- to long-term studies [17, 18].
To reduce microvascular complications and cardiovascular disease, the major cause of death in individuals with diabetes, hypertension, and dyslipidemia play important roles. In T2D patients, lipid abnormalities are thought to be secondary to obesity, insulin resistance, and decreased insulin production [19]. Analysis of blood pressure measurements and serum lipid profiles showed favorable results in all four groups, in our study. Patients in each group had a significant reduction in the use of antihypertensive and antihyperlipidemia agents, compared with baseline. The results were maintained for the 36-month follow-up, and metabolic outcomes were generally similar among the four groups. RYGB more effectively lowered diastolic blood pressure than systolic blood pressure. The most significant improvement in serum lipid profiles was seen in total triglyceride levels. Serum total cholesterol, high-density lipoprotein cholesterol, and low-density lipoprotein cholesterol remained within normal ranges. This could be explained by the fact that most dyslipidemia patients in this study experienced hypertriglyceridemia. Cardiovascular risk, calculated as the total cholesterol to HDL ratio, and low-degree inflammation, measured by hsCRP levels, both decreased substantially.
Although we found significant improvement in metabolic outcomes, there was a trend for weight regain and unsuccessful diabetes control. Vidal et al. [20] showed that non-adherence after surgery was associated with poor surgical results, especially in the first year. Furthermore, irregular life and diet style may also be important reasons for long-term surgical failure [20]. We emphasize the importance of improving follow-up rates and postoperative education to reduce the incidence of unsuccessful diabetes control.
Most guidelines and insurance coverage for metabolic surgery limit access to patients with BMI ≥35 kg/m2, presumably because of insufficient studies evaluating outcomes in patients with BMI <35 kg/m2. In our medium-term study, patients in different BMI classes had great improvement in diabetes control and other metabolic outcomes, similar to other studies [15, 16], which was encouraging. But, we also realized that the relapse rate of T2D remission in low-BMI group was higher than in high-BMI group, which remind us to perform RYGB in low-BMI patients very carefully. These results also suggest the hypothesis that T2D remission after RYGB may depend not only on the initial BMI but also other important factors such as duration, age, or β-cell function.
Important limitations of our study include the retrospective design and an inadequate sample size and duration to detect differences in long-term efficacy and safety; the low numbers per group may be permitting a type 2 error. Therefore, our results should be regarded as preliminary. Second, we did not investigate patients’ quality of life as an additional assessment, and BMI grouping was based on Chinese standards, which are different than for Western patients.
Conclusions
Despite the limitations in our study, we conclude that RYGB represents an effective procedure to treat T2D patients in Chinese patients. Our patients achieved diabetes remission and metabolic disorder control and reduced their cardiovascular risk. The initial BMI was related to A1C and might influence the diabetes remission as well. We should select appropriate T2D patients with low BMI carefully. Furthermore, there was a trend for weight regain and unsuccessful diabetes control in long-term outcomes.
References
Buchwald H, Estok R, Fahrbach K, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122(3):248–56.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes—3-year outcomes. N Engl J Med. 2014;370(21):2002–13.
Dixon JB, Zimmet P, Alberti KG, et al. Bariatric surgery: an IDF statement for obese type 2 diabetes. International Diabetes Federation Taskforce on Epidemiology and Prevention. Surg Obes Relat Dis. 2011;7(4):433–47.
Rubino F, Kaplan LM, Schauer PR, et al. The Diabetes Surgery Summit consensus conference: recommendations for the evaluation and use of gastrointestinal surgery to treat type 2 diabetes mellitus. Ann Surg. 2010;251(3):399–405.
Lee WJ, Hur KY, Lakadawala M, et al. Predicting success of metabolic surgery: age, body mass index, C-peptide, and duration score. Surg Obes Relat Dis. 2013;9(3):379–84.
Cohen RV, Pinheiro JC, Schiavon CA, et al. Effects of gastric bypass surgery in patients with type2 diabetes and only mild obesity. Diabetes Care. 2012;35(7):1420–8.
Malapan K, Goel R, Tai CM, et al. Laparoscopic Roux-en-Y gastric bypass for nonobese type II diabetes mellitus in Asian patients. Surg Obes Relat Dis. 2014;10(5):834–40.
Vetter ML, Cardillo S, Rickels MR, et al. Narrative review: effect of bariatric surgery on type 2 diabetes mellitus. Ann Intern Med. 2009;150(2):94–103.
Xu Y, Wang L, He J, et al. Prevalence and control of diabetes in Chinese adults. J Am Med Assoc. 2013;310(9):948–59.
Yu H, Di J, Bao Y, et al. Visceral fat area as a new predictor of short-term diabetes remission after Roux-en-Y gastric bypass surgery in Chinese patients with a body mass index less than 35 kg/m2. Surg Obes Relat Dis. 2015;11(1):6–11.
Chen C, Lu FC. The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed Environ Sci. 2004;17(Suppl):1–36.
Brethauer SA, Kim J, el Chaar M, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Surg Obes Relat Dis. 2015;11(3):489–506.
Sjöström L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351(26):2683–93.
Huang CK, Shabbir A, Lo CH, et al. Laparoscopic Roux-en-Y gastric bypass for the treatment of type II diabetes mellitus in Chinese patients with body mass index of 25–35. Obes Surg. 2011;21(9):1344–9.
Dixon JB, Chuang LM, Chong K, et al. Predicting the glycemic response to gastric bypass surgery in patients with type 2 diabetes. Diabetes Care. 2013;36:20–6.
Lee WJ, Chong K, Chen JC, et al. Predictors of diabetes remission after bariatric surgery in Asia. Asian J Surg. 2012;35(2):67–73.
Puzziferri N, Roshek 3rd TB, Mayo HG, et al. Long-term follow-up after bariatric surgery: a systematic review. J Am Med Assoc. 2014;312(9):934–42.
Ribaric G, Buchwald JN, McGlennon TW. Diabetes and weight in comparative studies of bariatric surgery vs conventional medical therapy: a systematic review and meta-analysis. Obes Surg. 2014;24(3):437–55.
Alberti KG, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–5.
Vidal P, Ramón JM, Goday A, et al. Lack of adherence to follow-up visits after bariatric surgery: reasons and outcome. Obes Surg. 2014;24(2):179–83.
Acknowledgments
This study was supported by grants from scientific research funds of the Shanghai Jiao Tong University Affiliated Sixth People’s Hospital (1642), the Chinese Society of Endocrinology, Key Program of the Shanghai Municipality for Basic Research (11 JC1409600), 973 program (2011 CB504001), and the National Major Scientific and Technological Special Project for “Significant New Drugs Development” (2011 ZX09307–001–02).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
For this type of study, formal consent is not required.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Hongwei Zhang and Xiaodong Han contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zhang, H., Han, X., Yu, H. et al. Effect of Roux-en-Y Gastric Bypass on Remission of T2D: Medium-Term Follow-up in Chinese Patients with Different BMI Obesity Class. OBES SURG 27, 134–142 (2017). https://doi.org/10.1007/s11695-016-2262-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-016-2262-5