Abstract
Background
High intraabdominal pressure (IAP) during laparoscopic surgery has been associated with postoperative discomfort. Effects on nausea and access have not been subjected to randomized studies. In cholecystectomy, lower IAP may cause less pain, but nausea and surgical access in RYGB surgery have not been investigated. We studied the influence of two IAP levels on surgical access, operation time, postoperative pain, and nausea.
Methods
Fifty consecutive female gastric bypass patients were randomized to intraabdominal pressure of 12 (IAP12) or 18 (IAP18) mm Hg. Surgeons and personnel were blinded to randomization; study groups were well matched for age and BMI. Operative time was noted in minutes. Visual analogue scales were used for assessing access and for patients assessing pain (abdomen-shoulder) and nausea (supine-standing) at six time points during the first 16 postoperative hours. Rescue medication was recorded.
Results
In 3/25 patients in the IAP12 group, the code was broken due to access problems vs. 0/25 in the IAP18 group (p = 0.1398). Operative time did not differ. Access was significantly better for IAP18 (92.2 ± 2.3 vs. 69.3 ± 4.2; p = 0.0001). Postoperative shoulder pain was maximal after 6 h but throughout less than in the abdomen (p < 0.0001); there were no differences in pain between IAP18 and IAP12 (p = 0.7408). Postoperative nausea was significantly greater standing than supine but without differences between groups.
Conclusion
Higher IAP gives better surgical access in laparoscopic Roux-en-Y gastric bypass with no negative effect on pain or nausea.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Postoperative pain and nausea often determine how rapidly patients can be mobilized following surgery and resume oral food intake and thus be safely discharged to their homes. Higher levels of intraabdominal pressure (IAP) during laparoscopic surgery may increase postoperative discomfort [1, 2], but other reports indicate no difference [3, 4] between high or low intraabdominal pressure during surgery. These studies have been performed with low-pressure levels and in cholecystectomy patients. The question of surgical access with different intraabdominal pressure levels has not been addressed. Since 2007, we have used a protocol for Enhanced Recovery After Surgery (ERAS) in our surgical unit, and we regularly oversee our routines for possible improvements. In this study, we investigated the influence of two different levels of IAP on surgical access, operation time, and postoperative pain (abdomen and shoulders) as well as nausea (supine and standing).
Patients and Methods
Fifty consecutive female gastric bypass patients were randomized to an intraabdominal pressure of 12 (IAP12) or 18 (IAP18) mm Hg after initiation of anesthesia. The patients did not participate in any other study, and all patients gave informed consent prior to surgery. The groups were well matched for age and BMI (Table 1). Surgeons and ward personnel were blinded. Operative time and carbon dioxide consumption were recorded. Visual analogue scales (VAS; 100 mm) were used for surgeon’s assessment of access (100 mm optimal). Patients assessed pain (abdomen-shoulder) and nausea (supine-standing) at six points in time during the first 16 postoperative hours using a visual analogue scale where 0 represented no discomfort and 100 mm worst imaginable discomfort.
Our Enhanced Recovery After Surgery (ERAS) protocol has previously been described in detail [5, 6].
Routine and On-Demand Medication Before Operation
All patients were routinely given 2 g acetaminophen oral (p.o.) (Alvedon®, GlaxoSmithKline), 8 mg betamethasone p.o. (Betapred®, SOBI), and 120 mg etoricoxib p.o. (Arcoxia®, MSD) preoperatively.
Anesthesia and Surgical Procedure
All patients were operated between 8 a.m. and 2 p.m. with identical anesthetic technique using propofol (Propofol®, Lipura, Sweden) and remifentanil (Ultiva®, GlaxoSmithKline, Sweden) in a target-controlled infusion, as previously described. Atracurium 20 mg intravenous (i.v.) (Atracurium-hameln®, Algol Pharma, Kista, Sweden) was given at the induction of anesthesia. No anesthesia gases were used and propofol infusion was maintained until 3 min before completion of surgery. At the end of the surgery, 10 mg ketobemidon (Ketogan®, Pfizer) was given i.v., and clonidine 22.5 μm i.v. (Catapresan®, Boehringer Ingelheim, Ingelheim am Rhein, Germany).
A standard Roux-Y gastric bypass with a small, completely separated pouch, a 60-cm biliopancreatic limb, and a 150-cm ante-colic, ante-gastric alimentary limb was performed as previously described [7]; all by the same surgeon (HG). The mesenterial openings were closed. The IAP throughout the procedure was either 12 or 18 mm Hg.
Routine and On-Demand Medication After Operation
All patients were allowed to sip liquids immediately after surgery. In addition, they received 1500–2000 mL of 5 % glucose solution over the study period. Patients spent 2 h in the recovery room (RR), where they usually received injections of 0.5–1 mg alfentanil (Rapifen®, Jansen Pharmaceuticals, Sollentuna, Sweden) and 0.5 mg droperidol (Dridol®, Prostrakan AB, Kista, Sweden). After recovery, the patients were transferred to the ward where they received 1 g acetaminophen p.o. (Alvedon®, GlaxoSmithKline) every 6 h and an injection of 10 mg of oxycodone (Oxycontin®, Mundifarma AB, Göteborg, Sweden) at 8 p.m. on the day of operation.
Supplementary Medication
Additional medication was offered if patients scored >30 for nausea or pain; such medication was recorded (Table 1). For nausea, we used 0.5 mg droperidol i.v. or ondansetron 2 mg i.v. (Ondansetron®, B Braun) and 10 mg ketobemidon s.c. for pain. Pain and nausea are reported as VAS score for each time point, and area-under-the-curve (AUC) calculations are used to express total amount of pain and nausea.
Statistics
All data are presented as mean (SEM). Area-under-the-curve calculations were performed using GraphPad Prism 5 (GraphPad Software, San Diego, CA). Distributions were analyzed using Kolmogorov-Smirnov testing; differences between groups were calculated with two-tailed unpaired tests using Winstat for Excel® (Kalmia, NY, USA), and differences with a p value <0.05 were considered statistically significant.
Results
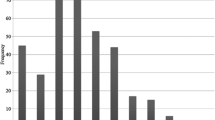
Groups were well matched for age and BMI (Table 1). In 3/25 patients in the IAP12 group, the code was broken due to access problems during the operation whereas vs. 0/25 in the IAP18 group (p = 0.1398). Operative time was short and consistent, for IAP12 29.9 (1.4) vs. IAP18 28.5 (0.9); there was no difference between groups (Fig. 1). Total amount of carbon dioxide used was significantly higher in IAP18 than in IAP12 (78.5 (6.2) vs. 52.3 (4.1); p = 0.0041). Access was assessed as significantly better in the IAP18 group (92.2 ± 2.3 vs. 69.3 ± 4.2, p = 0.0001; Fig. 2). Pain scores are illustrated in Figs. 3–5. Postoperative shoulder pain was maximal after 6 h but throughout the study period less than in the abdomen (p < 0.0001). There were no differences in pain in either location between IAP18 and IAP12 (p = 0.7408). AUC calculation showed no difference between groups, neither for abdominal pain (Fig. 4) nor for shoulder pain (p = 0.0737; Fig. 5). Postoperative nausea scores (Fig. 6) were significantly greater standing than supine (p < 0.001) but without differences between pressure groups.
VAS levels of abdominal and shoulder pain at different time points (100 mm is worst imaginable pain). There were no significant differences between pressure groups at any time point, but abdominal pain was higher than shoulder pain throughout the postoperative period, p < 0.0001. Blue = 12 and red = 18 mm Hg; solid lines indicate abdominal pain level and dashed lines indicate shoulder pain
Discussion
Postoperative pain and nausea are important factors in determining how quickly patients can be discharged from hospital. Many attempts have been made to minimize pain, such as saline washout [8, 9] or insufflation with heated gas [10] with no positive results on patients’ discomfort. In this study, we investigated whether higher intraabdominal pressure (18 vs 12 mm Hg) was associated with greater postoperative discomfort. We found no differences in postoperative discomfort between our two groups even though the gas consumption was significantly higher in IAP18. This could possibly be explained by the fact that premedication in all cases included corticosteroids to minimize peritoneal irritation. Another contributing factor could be the short and consistent operative times. In fact, the surgeon’s assessment of access was significantly higher in the IAP18 group but that did not significantly influence operative times.
Most studies on the impact of different pressure levels have been conducted on cholecystectomy patients and focused on shoulder tip pain, using IAP of 8–15 mm Hg. Results have been inconclusive with some studies reporting increased patient discomfort with higher IAP [1, 2], while other studies have not shown any connection between patient discomfort and IAP [3, 4]. To increase sensitivity, we used VAS measurements to obtain continuous data, in addition to normal PONV reporting on rescue medication. We found in the present series randomizing between 12 and 18 mm Hg no difference between pressure groups, neither for abdominal pain nor shoulder tip pain, and there were no differences in the need for extra medication between groups, neither for pain nor nausea. We also found that abdominal pain was more severe than shoulder pain at all time points in both pressure groups.
Laparoscopic surgery in the morbidly obese can be technically challenging due to limited access. Theoretically, increasing the IAP might accomplish better access, but concerns have been expressed as to a negative influence on hemodynamics and pulmonary function in RYGB even though these fears have not been substantiated [11, 12]. We found that IAP18 gave significantly better exposure than IAP12 but did not shorten operative time in our hands. This may be because our learning curve for efficiency has leveled off. Nevertheless, short operating times have been associated with less complications [13], possibly because of a surgical team of greater experience. With increasing experience of the procedure, operating times have been halved in Sweden over the last 7 years. The mean operating time for a laparoscopic gastric bypass in the Swedish registry, SOReg, [14] is now 63 min [15]. To study whether an IAP of 18 mm Hg is suitable even in longer operations calls for more studies. Importantly, the ERAS protocol and staff experience must be carefully standardized, factors which speak for a single-center study such as the present one. Furthermore, the surgical team should have passed the steep phase of the learning curve. Our data justify ethically the undertaking of such studies.
It is reasonable to believe that the net effect on patients’ discomfort is among other things, the combination of good surgical exposure facilitating a quick operation with minimal amount of manipulation and low volumes of carbon dioxide. Our findings of increased nausea when standing confirm previous findings on the importance of body position [16].
Our results underline the importance of adhering to an ERAS protocol. We set out to study the net importance of varying the IAP using surgeon’s access and patient-assessed discomfort as our primary end points. In conclusion, our data indicate that higher IAP leads to better surgical exposure without increasing the patients’ postoperative discomfort.
References
Gurusamy KS, Vaughan J, Davidson BR. Low pressure versus standard pressure pneumoperitoneum in laparoscopic cholecystectomy. Surg Endosc. 2009;23(5):1044–7.
Barczynski M, Herman RM. A prospective randomized trial on comparison of low-pressure (LP) and standard-pressure (SP) pneumoperitoneum for laparoscopic cholecystectomy. Surg Endosc. 2003;17(4):533–8.
Koc M, Ertan T, Tez M, et al. Randomized, prospective comparison of postoperative pain in low-versus high-pressure pneumoperitoneum. ANZ J Surgery. 2005;75(8):693–6.
Perrakis E, Vezakis A, Velimezis G, et al. Randomized comparison between different insufflation pressures for laparoscopic cholecystectomy. Surgical Laparoscopy Endoscopy Percutaneous Techn. 2003;13(4):245–9.
Bergland A, Gislason H, Raeder J. Fast-track surgery for bariatric laparoscopic gastric bypass with focus on anaesthesia and peri-operative care. Experience with 500 cases. Acta Anaesthesiol Scand. 2008;52(10):1394–9. doi:10.1111/j.1399-6576.2008.01782.x.
Karlsson A, Wendel K, Polits S, Gislason H, Hedenbro J. Preoperative nutrition and postoperative discomfort in an ERAS setting: a randomized study in gastric bypass surgery. Obesity Surgery, In press
Aghajani E, Jacobsen HJ, Nergaard BJ, et al. Internal hernia after gastric bypass: a new and simplified technique for laparoscopic primary closure of the mesenteric defects. J Gastrointest Surg. 2012;16:641–5.
Barczynski M, Herman RM. Low-pressure pneumoperitoneum combined with intraperitoneal saline washout for reduction of pain after laparoscopic cholecystectomy: a prospective randomized study. Surg Endosc. 2004;18(9):1368–73.
Esmat ME, Elsebae MMA, Nasr MMA, et al. Combined low pressure pneumoperitoneum and intraperitoneal infusion of normal saline for reducing shoulder tip pain following laparoscopic cholecystectomy. World J Surg. 2006;30(11):1969–73.
Manwaring JM, Readman E, Maher PJ. The effect of heated humidified carbon dioxide on postoperative pain, core temperature, and recovery times in patients having laparoscopic surgery: a randomized controlled trial. J Minim Invasive Gynecol. 2008;15(2):161–5.
Nguyen NT, Anderson JT, Budd M, et al. Effects of pneumoperitoneum on intraoperative pulmonary mechanics and gas exchange during laparoscopic gastric bypass. Surg Endosc. 2004;18(1):64–71.
Nguyen NT, Ho HS, Fleming NW, et al. Cardiac function during laparoscopic vs open gastric bypass. Surg Endosc. 2002;16(1):78–83.
Reames BN, Bacal D, Krell RW, et al. Influence of median surgeon operative duration on adverse outcomes in bariatric surgery. Surg Obes Relat Dis. 2015;11(1):207–13. doi:10.1016/j.soard.2014.03.018.
Hedenbro JL, Näslund E, Boman L, Lundegårdh G, Bylund A, Ekelund M, Ottosson J. Formation of the Scandinavian obesity surgery registry, SOReg. Obesity Surgery. 2015; 1–8.
Scandinavian Obesity Surgery Registry annual reports http://www.ucr.uu.se/soreg/index.php/arsrapporter (accessed 15 June 2015)
Nguyen NQ, Debreceni TL, Burgstad CM, et al. Effects of posture and meal volume on gastric emptying, intestinal transit, oral glucose tolerance, blood pressure and gastrointestinal symptoms after Roux-en-Y gastric bypass. Obes Surg. 2015;25(8):1392–400.
Acknowledgments
This study was approved by the Institutional Review Board and the Lund University Ethics Committee and performed after informed consent by all participants according to the principles of the Helsinki declaration.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Yvette Caesar, Ilona Sidlovskaja, Andreas Lindqvist, Hjörtur Gislason, and Jan L. Hedenbro report no conflict of interest.
Disclosure
None of the authors has anything to disclose in relation to the present article.
Additional information
Y. Caesar and I. Sidlovskaja contributed equally to this work.
Parts of this study have been reported in abstract form to the IFSO meeting in Vienna, August 2015.
Rights and permissions
About this article
Cite this article
Caesar, Y., Sidlovskaja, I., Lindqvist, A. et al. Intraabdominal Pressure and Postoperative Discomfort in Laparoscopic Roux-en-Y Gastric Bypass (RYGB) Surgery: a Randomized Study. OBES SURG 26, 2168–2172 (2016). https://doi.org/10.1007/s11695-016-2091-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-016-2091-6