Abstract
Post-traumatic stress disorder (PTSD) is a debilitating condition which has been related to problems in emotional regulation, memory and cognitive control. Psychotherapy has a non-response rate of around 50% and understanding the neurobiological working mechanisms might help improve treatment. To integrate findings from multiple smaller studies, we performed the first meta-analysis of changes in brain activation with a specific focus on emotional processing after psychotherapy in PTSD patients. We performed a meta-analysis of brain activation changes after treatment during emotional processing for PTSD with seed-based d mapping using a pre-registered protocol (PROSPERO CRD42020211039). We analyzed twelve studies with 191 PTSD patients after screening 3700 studies. We performed systematic quality assessment both for the therapeutic interventions and neuroimaging methods. Analyses were done in the full sample and in a subset of studies that reported whole-brain results. We found decreased activation after psychotherapy in the left amygdala, (para)hippocampus, medial temporal lobe, inferior frontal gyrus, ventrolateral prefrontal cortex, right pallidum, anterior cingulate cortex, bilateral putamen, and insula. Decreased activation in the left amygdala and left ventrolateral PFC was also found in eight studies that reported whole-brain findings. Results did not survive correction for multiple comparisons. There is tentative support for decreased activation in the fear and cognitive control networks during emotional processing after psychotherapy for PTSD. Future studies would benefit from adopting a larger sample size, using designs that control for confounding variables, and investigating heterogeneity in symptom profiles and treatment response.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many people experience a traumatic event during their lifetime (around 70%), and around 5% subsequently develop post-traumatic stress disorder (PTSD; Koenen et al., 2017). Patients with PTSD suffer from re-experiencing symptoms, hypervigilance to possible threats, avoidance of trauma-related situations and feelings, negative alterations in cognitions and mood, as well as alterations in arousal and reactivity (American Psychiatric Association, 2013). PTSD is a debilitating condition which has been related to problems in emotion regulation and cognitive control and this is reflected in recent neuroimaging studies. Meta-analyses on fMRI studies using paradigms that elicit fear or other aversive emotions (such as the emotional faces task, conditioned fear paradigm or symptom provocation) have shown altered activation in PTSD patients compared to healthy controls in the amygdala, insula, striatum, and temporal gyrus (Schulze et al., 2019; Suarez-Jimenez et al., 2020). The level of activation was also partly found to be positively associated with PTSD severity (Thome et al., 2020).
Neurobiological models of emotion dysregulation in PTSD have evolved over time. Rauch et al. (2006) based the first model on fear conditioning models, where amygdala hyperactivation fails to be regulated by (medial) prefrontal regions and the hippocampus, while hippocampus overaction leads to impairments in fear contextualization/generalization. Lanius et al. (2010) later described two subtypes of PTSD with their own model of emotion dysregulation. The original re-experiencing/hyperarousal subtype, with failing inhibition of limbic areas such as the amygdala accompanied by the lower activation in medial prefrontal regions (e.g. the ventromedial prefrontal cortex (vmPFC) and rostral anterior cingulate cortex (rACC)) is specified as the “undermodulation” of emotions (Lanius et al., 2010). The dissociative subtype, on the other hand, shows an unusually high activation in emotion regulation areas such as the dorsal ACC and medial PFC, and is specified as the “overmodulation” of limbic areas (Lanius et al., 2010).
Later neurocircuitry models of PTSD and have been extended to include the salience and central executive networks as well as the fronto-limbic circuit (Patel et al., 2012). The salience network is involved in emotion regulation, conflict management and reward processing and is overactive in PTSD (Patel et al., 2012). Important regions in the salience network are the amygdala, insula and dorsal ACC. Conceptually the salience network overlaps partly with the fear network (LeDoux & Daw, 2018; LeDoux & Pine, 2016). The central executive network is involved in attentional control and working memory and has been found to be hypoactive in patients with PTSD (Patel et al., 2012). The central executive network overlap with the cognitive control network (LeDoux & Daw, 2018; LeDoux & Pine, 2016). Important brain regions involved in this network are the dorsolateral PFC and lateral parietal cortices. Patients with PTSD show less activation in the default mode network, which includes areas such as the medial PFC, posterior cingulate cortex and parahippocampal gyrus and is involved in internal processes such as self-referential thinking (Patel et al., 2012).
There is some evidence that the altered activation in areas in the salience, central executive and default mode networks might be normalized by psychological treatment. Current first-line psychological treatments for PTSD includes trauma-focused psychotherapies such as prolonged exposure therapy, eye-movement desensitization and reprocessing (EMDR), and cognitive processing therapy (Merz et al., 2019). Common elements in al therapies are exposure to the memory of the traumatic event, cognitive processing, targeting of emotions and emotion regulation skills (Schnyder et al., 2015). Trauma-focused psychological treatment for PTSD generally has clinically relevant positive effect (Lewis et al., 2020) with large effect sizes (Weber et al., 2021), but nonresponse rates can go up to 50% (Schottenbauer et al., 2008). Understanding how activation in the brain changes after therapy might help to improve treatment response, e.g. through transcranial magnetic stimulation (Harris & Reece, 2021).
So far, three systematic reviews have been published on the effect of psychotherapy on the brain in PTSD, both structural and functional. Thomaes et al. (2014) conclude that studies show a decrease in amygdala activation and an increase in dlPFC activation after therapy. Malejko et al. (2017) also conclude a decrease in amygdala activation after successful therapy, next to a decrease in the insula, and an increase in dorsal ACC and hippocampus activation. Manthey et al. (2021), on the other hand, conclude that change in amygdala activation is unclear and that there is some evidence of increased activation in the mPFC, albeit in different areas across studies and not in all studies. These diverging conclusions highlight the importance of meta-analysis for quantitatively assessing how robust the reported findings are (Button et al., 2013). A possible reason for the diverse conclusions from these reviews is the heterogeneity of included studies, which included a range of scanning paradigms and both pharmacological and psychotherapeutic interventions.
To overcome some of the limitations of the previous reviews, we performed a pre-registered coordinate-based meta-analysis of functional neuroimaging studies to identify the most consistent findings of change in brain activation patterns after trauma-focused psychotherapy for PTSD (PROSPERO CRD42020211039). As impaired negative emotion processing is a core symptom of PTSD and to improve homogeneity between the studies, we limited the inclusion of studies to those that probed emotional processing by directly comparing negative emotional and neutral stimuli using a pre- to post-treatment design.
Method
Study selection
A systematic literature search was conducted in PubMed, APA PsycInfo (EBSCO), Embase (Embase.com), and Web of Science (Clarivate), from inception until December 14th, 2021. Search terms were a combination of various forms of the terms: “PTSD” and “Imaging” (see supplementary materials for the full list of search terms). To be as inclusive as possible, we chose not to include ‘psychotherapy’ as a search term but manually select the intervention studies during the screening procedure. To increase homogeneity between studies, we only included studies that used a negative versus neutral contrast. Inclusion criteria were that the studies: 1) included a sample of patients with PTSD according to the Diagnostic and Statistical Manual of Mental Disorders (DSM) or the International Classification of Diseases (ICD); 2) used an emotional paradigm with a negative emotional and a neutral condition during functional neuroimaging (functional magnetic resonance imaging (fMRI), single-photon emission computed tomography (SPECT) or positron emission tomography (PET); 3) used this paradigm before and after trauma-focused psychotherapy; 4) reported activation data for a contrast of a negative emotional condition versus a neutral condition. We did not have any exclusion criteria.
After removing all duplicates, two authors (IA and ALT) independently screened all titles and abstracts through Rayyan (https://rayyan.qcri.org) followed by all remaining full texts. Disagreements were solved by consensus. This study was preregistered in PROSPERO (CRD42020211039).
Data extraction and quality assessment
Data were extracted from the papers by two authors (IA and ALT). We extracted information about patient demographics (age, sex), diagnosis (PTSD severity before and after treatment, type of trauma, comorbidity), treatment (type of treatment, number of sessions), and medication use in patients. We also extracted data on time between scans, type of scanner, scanning sequence parameters, software used to analyze the data, statistical methods and thresholds, coordinates of significant peak voxels where patients showed changes in brain activation during a negative versus neutral emotional condition, as well as the corresponding t-value. Finally, we extracted data about task design, stimuli presentation, and timing, as well as the contrasts being used.
All included papers were independently assessed for methodological quality (by IA and ALT), using a 22-item rating scale developed for psychotherapy studies (range: 0–44, Öst, 2008) and 15 items from the COBIDAS checklist for neuroimaging studies (See Supplemental Materials; range: 0–15, Nichols et al., 2017)). We determined the intraclass correlation between the raters with a two-way random model with absolute agreement while the final quality ratings were settled through consensus.
Statistical analyses
Preprocessing and meta-analysis of significant peak coordinates from the included studies was performed using seed-based d mapping (SDM; https://www.sdmproject.com; Radua et al., 2012). SDM handles both positive and negative peak coordinates using reported t-values in a single map per study, leading to more nuanced statistical parametric maps. Hedge’s g effect size was estimated per voxel, and the map was smoothed by an anisotropic Gaussian kernel using a gray-matter-specific template (Radua et al., 2014). The statistical parametric maps were then included in a random-effects meta-analysis weighted by sample size and within- and between-study heterogeneity. This resulted in a whole-brain map of changes in brain activation from pre- to post-treatment. First, we investigated changes in brain activation after psychotherapy using all available data, including studies with whole-brain analyses and those using regions of interest (ROIs, see Supplementary materials for full list of ROIs included in the studies). We included as a covariate whether a study included ROI findings (yes/no). To further ensure that findings were not driven by ROI-based studies with less stringent statistical thresholds we re-ran the analyses by including only whole-brain studies. We used a meta-regression to investigate the relationship between changes in activation after psychotherapy and the effect size of the treatment on clinical symptoms (Cohen’s d), calculated as [PTSD severity pre-treatment—PTSD severity post-treatment)/SD pre-treatment]. We report results at an uncorrected statistical level (two-tailed p < 0.05 for the overall change in activation after therapy and p < 0.005 for the meta-regression) and corrected for multiple comparisons using threshold-free cluster enhancement (TFCE) correction (p < 0.05). Publication bias was assessed using Egger’s test and I2 as a measure of the heterogeneity.
Results
Characteristics of the included studies
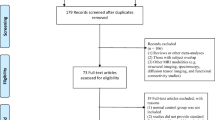
Our search identified 3700 unique records. After title/abstract screening, 39 studies remained for full-text screening. We excluded 27 studies for the following reasons: absence of post-treatment scan (n = 2), absence of relevant negative emotional vs. neutral contrast (n = 11), absence of activation data (n = 5), patients not receiving treatment (n = 4), no PTSD sample (n = 1), or insufficient details e.g., on the statistics (n = 4). Attempts were made to contact the corresponding authors in cases where information was missing or ambiguous. Eleven fMRI studies and one PET study were included in the final analyses, where eight included data from whole-brain analyses (see Fig. 1 for the full flow chart). Four of the twelve studies did not report a t-value or statistics that could be converted to a t-value (Aupperle et al., 2013; Garrett et al., 2019; King et al., 2016; Simmons et al., 2013). We, therefore, coded peaks of increased activation from pre- to post-treatment as “positive” and decreased activation as “negative”, as is standard practice in SDM.
The 12 included studies included a total sample of 191 patients with PTSD with both pre- and post-treatment scans (See Table 1 for full information about the samples). Of the included studies, 11 included an adult sample (> 18 years) while one included an adolescent sample (Garrett et al., 2019). Since activation patterns for adolescents can be similar to adults (Herringa, 2017) we have included this study in our meta-analysis. Most studies used the Clinician-Administered PTSD Scale–DSM IV (CAPS-IV) as the main PTSD severity measure, while two studies (Garrett et al., 2019; Rousseau et al., 2019) used the self-reported UCLA PTSD Reaction Index for DSM-IV (PTSD-RI) or PTSD Checklist Scale (PCL-S), respectively. Two studies included patients with partial PTSD who did not all fulfill the full diagnostic criteria (Aupperle et al., 2013; Peres et al., 2011). In one study, 79% of patients had full PTSD but analyses were not reported separately for full and partial PTSD (Aupperle et al., 2013). In another study of working police officers all patients fulfilled the re-experiencing and hyperarousal criteria but not the numbing or avoidance criteria (Peres et al., 2011). Treatment duration ranged from a mean of 2.5 to 20 sessions. Eight studies used cognitive behavioral therapy/prolonged exposure (Aupperle et al., 2013; Felmingham et al., 2007; Fonzo et al., 2017; Garrett et al., 2019; Helpman et al., 2016; Peres et al., 2011; Simmons et al., 2013; Thomaes et al., 2012), two used mindfulness-based therapies (Bremner et al., 2017; King et al., 2016), and two used either EMDR or a mix of EMDR and cognitive behavioral therapy (Rousseau et al., 2019; van Rooij et al., 2016). (See Table 2 for estimated standardized mean difference changes in symptom severity after psychotherapy). Five studies used an emotional faces task (Felmingham et al., 2007; Fonzo et al., 2017; Garrett et al., 2019; King et al., 2016; Rousseau et al., 2019), three used symptom provocation (Bremner et al., 2017; Peres et al., 2011; van Rooij et al., 2016), one used fear extinction (Helpman et al., 2016), and three used cognitive tasks with emotional stimuli (Aupperle et al., 2013; Simmons et al., 2013; Thomaes et al., 2012).
Changes in brain activation after therapy
The main meta-analysis of all 12 studies found six significant clusters of decreased activation after psychotherapy at an uncorrected threshold (p < 0.05, two-tailed, see Table 3 and Fig. 2). The largest cluster (Fig. 2A) encompassed the left amygdala, putamen, hippocampus, parahippocampus, and medial temporal lobe. The second cluster (2B) included the right putamen, pallidum and posterior insula, the third cluster (2C) included the inferior frontal gyrus (pars orbitalis), the fourth cluster (2D) the right anterior cingulate cortex, the fifth cluster (2E) the left ventrolateral PFC, and the sixth cluster (2F) included the left anterior insula. No cluster survived TFCE correction for multiple comparisons. There were no brain areas that showed a significant increase in activation after psychotherapy. A meta-regression showed no significant relationship between change in symptom severity and change in brain activation after treatment. We also found no evidence for publication bias based on Egger’s tests or funnel plots, and the I2 suggested little to moderate heterogeneity in the findings.
Changes in brain activation after psychotherapy. Results show a decrease of activation after psychotherapy in the A) left amygdala, (para)hippocampus, putamen, and medial temporal lobe; B) left and right right putamen; C) left inferior frontal gyrus (pars orbitalis); D) right anterior cingulate; E) left ventrolateral prefrontal cortex; F) left insula
Decreased activation in the left amygdala, medial temporal lobe cortex and left ventrolateral PFC after psychotherapy was also found when the meta-analysis was restricted to the eight studies that reported whole-brain results, but these were not significant after TFCE-correction for multiple comparisons.
Methodological quality
As shown by the psychotherapy methodology rating scales (see Supplementary Table 2), most studies used reliable and specific outcome measures in a well described and representative sample. Four studies (33%) were randomized controlled trials, while 8 studies (66%) did not include a treatment control group. Many studies did not use blinded evaluators, only measuring symptoms and/or brain function at two time points, while also not providing information about the therapist training and competence. Most studies did not perform a power analysis and did not describe how concominant psychological and pharmacological treatments were controlled.
With regard to neuroimaging information as assessed by an adaptation of the COBIDAS checklist, most studies reported the basic parameters about the type of scanner, scanning parameters and preprocessing pipeline. Most studies also provided an adequate description of the task parameters. However, not all studies provided information about the characteristics of the scan session, summary statistics for the task or information about randomization of the stimuli within the task. The intra-class correlation coefficient for the quality ratings between the two raters was high (0.88; 95% CI 0.55–0.97). The final consensus ratings can be found in Supplementary Table 2.
Discussion
We conducted the first coordinate-based meta-analysis on trauma-focused psychotherapy-induced changes in brain activation during emotional processing in PTSD. Our findings tentatively suggest that PTSD patients show decreased activation in several regions of the fear and cognitive control networks after therapy, including the amygdala, (para)hippocampus, putamen, pallidum, insula, inferior frontal gyrus, anterior cingulate cortex, and ventrolateral PFC, although these findings did not survive correction for multiple comparisons. Decreased activation in the left amygdala and ventrolateral PFC was also found when only studies assessing the whole-brain were included, but these findings were not significant after correction for multiple comparisons.
The emotional tasks used in the included studies are designed to induce distress, fear and trauma memories. A core component of trauma-focused psychotherapy is to learn how to manage distress and intrusive memories, address negative trauma-related cognitions, and discriminate traumatic memories from the present (Olff et al., 2020). In general, patients in the included studies responded well to treatment and showed improvement in PTSD symptoms. These symptoms include hyper responsivity to threats and avoidance. We theorize that this is associated with the reduced activation we found in regions of the fear network after successful therapy due to the reduced need for detecting threats and engaging in defensive behaviors. This is supported by previous research highlighting the role of the amygdala in the processing of immediate threats and intrusive memories and the putamen in the preparation and execution of defensive behaviors (Jahanshahi et al., 2015; LeDoux & Daw, 2018; LeDoux & Pine, 2016). Reduced activation in regions of the cognitive control network after therapy may reflect a decreased demand for processes such as the conscious evaluation of threat using working memory and integration with previous experiences mediated by the regions of the PFC and hippocampus (Belyk et al., 2017; Brohawn et al., 2010; LeDoux & Daw, 2018; LeDoux & Pine, 2016), or the integration of body signals involving the insula (Critchley et al., 2004; LeDoux & Daw, 2018; LeDoux & Pine, 2016). Despite the common elements of the different types of treatment, precise working mechanisms differ. For example, EMDR works through taxing working memory and prolonged exposure through reevaluation of negative cognitions (Schnyder et al., 2015; Shapiro, 2001). This might result in different changes in brain activation and might therefore lead to our current non-significant result. Because some studies compared responders to non-responders (for these studies we could not include the whole sample in our analyses) and other studies reported data for all patients (responders and non-responders together), it is unclear how change in activation pattern is related to clinical improvement. Our metaregression did not give an indication for an association between treatment effect size and change in brain activation.
An important limitation of the current meta-analysis is that only twelve studies could be included, which limits the power and generalizability of the findings. Our results should therefore be seen as preliminary evidence of changes in brain activation after treatment. The patient samples in the included studies differed on many clinical characteristics, including type and duration of traumatic events, comorbidity, medication status, and type and duration of treatment. Although the variation in these clinical characteristics reflects the diversity in the causes, presentations, and consequences of having PTSD, it likely also leads to less consistent patterns of altered brain activation at the group level (Benfer et al., 2018; Guina et al., 2018). Dissociation was not assessed in most of the studies, while dissociative symptoms in PTSD have been linked to less amygdala activation and more anterior cingulate and medial PFC activation (Roydeva & Reinders, 2021).
There were also some important methodological differences and shortcomings in the included studies, which should be taken into account when interpreting the results from the meta-analysis. The studies used different emotional processing tasks such as symptom provocation, cognitive tasks with emotional stimuli or fear extinction. While all studies were designed to elicit a negative emotional response, the tasks might invoke slightly different circuits in the brain. Unfortunately, we do not know of any studies that compare these different task directly. Most studies were small, which makes it unlikely to detect moderate to small changes in brain activation. A minority of studies also did not report data at the whole-brain level but only for specific ROIs, which may increase the probability of both false positive and negative findings (Müller et al., 2018). Less statistical power due to more stringent thresholds in studies using whole-brain contrasts likely resulted in the difference between our results when including all studies versus when only including studies assessing the whole-brain.
We recommend researchers to report not only ROI results but include whole-brain analysis in their studies, to aid future meta-analyses. The majority of studies used a non-randomized pre-post treatment design without a control group or with only a healthy control group to adjust for the passage of time or repetition effects in task-related distress and brain activation. Furthermore, many studies did not report on essential elements of the training of therapists and raters which makes it hard to properly rate the quality of the treatments. The few available studies make it difficult to run meaningful meta-regressions investigating the impact of comorbidity, medication, task paradigms, or specific treatments. Future studies should include information about these clinical characteristics to aid interpretation and comparison of results.
Conclusion
Studying the neural correlates of effective treatment for PTSD is vital to identify the brain regions and mechanisms of recovery. The present meta-analysis suggests that there is tentative support for decreased activation in the fear and cognitive control networks during emotional processing after psychotherapy for PTSD. Our findings are in line with prevailing models highlighting the role of normalized threat detection, monitoring, and action preparation in clinical recovery, but fail to provide evidence for increased prefrontal activation related to cognitive control and emotion regulation (LeDoux & Daw, 2018; LeDoux & Pine, 2016; Wen et al., 2022). There are several limitations in the studies that influence the interpretability of these findings, the most important one the limited number of includable studies. Future studies would be strengthened by adopting a larger sample size, using designs that control for confounding variables, and investigating heterogeneity in symptom profiles and treatment response.
Data Availability
Data is available from the corresponding author upon request.
Code availability
Not applicable
References
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.).
Aupperle, R. L., Allard, C. B., Simmons, A. N., Flagan, T., Thorp, S. R., Norman, S. B., Paulus, M. P., & Stein, M. B. (2013). Neural responses during emotional processing before and after cognitive trauma therapy for battered women. Psychiatry Research: Neuroimaging, 214(1), 48–55. https://doi.org/10.1016/j.pscychresns.2013.05.001
Belyk, M., Brown, S., Lim, J., & Kotz, S. A. (2017). Convergence of semantics and emotional expression within the IFG pars orbitalis. NeuroImage, 156, 240–248. https://doi.org/10.1016/j.neuroimage.2017.04.020
Benfer, N., Bardeen, J. R., Cero, I., Kramer, L. B., Whiteman, S. E., Rogers, T. A., Silverstein, M. W., & Weathers, F. W. (2018). Network models of posttraumatic stress symptoms across trauma types. Journal of Anxiety Disorders, 58, 70–77. https://doi.org/10.1016/j.janxdis.2018.07.004
Bremner, J. D., Mishra, S., Campanella, C., Shah, M., Kasher, N., Evans, S., Fani, N., Shah, A. J., Reiff, C., Davis, L. L., Vaccarino, V., & Carmody, J. (2017). A pilot study of the effects of mindfulness-based stress reduction on post-traumatic stress disorder symptoms and brain response to traumatic reminders of combat in operation enduring freedom/operation Iraqi Freedom combat veterans with post-traumatic stress disorder. Frontiers in Psychiatry, 8, 157. https://doi.org/10.3389/fpsyt.2017.00157
Brohawn, K. H., Offringa, R., Pfaff, D. L., Hughes, K. C., & Shin, L. M. (2010). The neural correlates of emotional memory in posttraumatic stress disorder. Biological Psychiatry, 68(11), 1023–1030. https://doi.org/10.1016/j.biopsych.2010.07.018
Button, K. S., Ioannidis, J. P., Mokrysz, C., Nosek, B. A., Flint, J., Robinson, E. S., & Munafò, M. R. (2013). Power failure: Why small sample size undermines the reliability of neuroscience. Nature Reviews Neuroscience, 14(5), 365. https://doi.org/10.1038/nrn3475
Critchley, H. D., Wiens, S., Rotshtein, P., Öhman, A., & Dolan, R. J. (2004). Neural systems supporting interoceptive awareness. Nature Neuroscience, 7(2), 189–195. https://doi.org/10.1038/nn1176
Felmingham, K., Kemp, A., Williams, L., Das, P., Hughes, G., Peduto, A., & Bryant, R. (2007). Changes in anterior cingulate and amygdala after cognitive behavior therapy of posttraumatic stress disorder. Psychological Science, 18(2), 127–129. https://doi.org/10.1111/j.1467-9280.2007.01860.x
Fonzo, G. A., Goodkind, M. S., Oathes, D. J., Zaiko, Y. V., Harvey, M., Peng, K. K., Weiss, M. E., Thompson, A. L., Zack, S. E., Mills-Finnerty, C. E., Rosenberg, B. M., Edelstein, R., Wright, R. N., Kole, C. A., Lindley, S. E., Arnow, B. A., Jo, B., Gross, J. J., Rothbaum, B. O., & Etkin, A. (2017). Selective effects of psychotherapy on frontopolar cortical function in PTSD. American Journal of Psychiatry, 174(12), 1175–1184. https://doi.org/10.1176/appi.ajp.2017.16091073
Garrett, A., Cohen, J. A., Zack, S., Carrion, V., Jo, B., Blader, J., Rodriguez, A., Vanasse, T. J., Reiss, A. L., & Agras, W. S. (2019). Longitudinal changes in brain function associated with symptom improvement in youth with PTSD. Journal of Psychiatric Research, 114, 161–169. https://doi.org/10.1016/j.jpsychires.2019.04.021
Guina, J., Nahhas, R. W., Sutton, P., & Farnsworth, S. (2018). The influence of trauma type and timing on PTSD symptoms. Journal of Nervous & Mental Disease, 206(1), 72–76. https://doi.org/10.1097/NMD.0000000000000730
Harris, A., & Reece, J. (2021). Transcranial magnetic stimulation as a treatment for posttraumatic stress disorder: A meta-analysis. Journal of Affective Disorders, 289, 55–65.
Helpman, L., Marin, M.-F., Papini, S., Zhu, X., Sullivan, G. M., Schneier, F., Neria, M., Shvil, E., Malaga Aragon, M. J., Markowitz, J. C., Lindquist, M. A., Wager, T. D., Milad, M. R., & Neria, Y. (2016). Neural changes in extinction recall following prolonged exposure treatment for PTSD: A longitudinal fMRI study. Neuroimage Clinical, 12, 715–723. https://doi.org/10.1016/j.nicl.2016.10.007
Herringa, R. J. (2017). Trauma, PTSD, and the developing brain. Current Psychiatry Reports, 19, 1–9.
Jahanshahi, M., Obeso, I., Rothwell, J. C., & Obeso, J. A. (2015). A fronto-striato-subthalamic-pallidal network for goal-directed and habitual inhibition. Nature Reviews Neuroscience, 16(12), 719–732. https://doi.org/10.1038/nrn4038
King, A. P., Block, S. R., Sripada, R. K., Rauch, S. A., Porter, K. E., Favorite, T. K., Giardino, N., & Liberzon, I. (2016). A pilot study of mindfulness-based exposure therapy in OEF/OIF combat veterans with PTSD: Altered medial frontal cortex and amygdala responses in social-emotional processing. Front Psychiatry, 7, 154. https://doi.org/10.3389/fpsyt.2016.00154
Koenen, K., Ratanatharathorn, A., Ng, L., McLaughlin, K., Bromet, E., Stein, D., Karam, E., Ruscio, A. M., Benjet, C., & Scott, K. (2017). Posttraumatic stress disorder in the world mental health surveys. Psychological Medicine, 47(13), 2260–2274. https://doi.org/10.1017/S0033291717000708
Lanius, R. A., Vermetten, E., Loewenstein, R. J., Brand, B., Schmahl, C., Bremner, J. D., & Spiegel, D. (2010). Emotion modulation in PTSD: Clinical and neurobiological evidence for a dissociative subtype. American Journal of Psychiatry, 167(6), 640–647. https://doi.org/10.1176/appi.ajp.2009.09081168
LeDoux, J. E., & Daw, N. D. (2018). Surviving threats: Neural circuit and computational implications of a new taxonomy of defensive behaviour. Nature Reviews Neuroscience, 19(5), 269–282. https://doi.org/10.1038/nrn.2018.22
LeDoux, J. E., & Pine, D. S. (2016). Using neuroscience to help understand fear and anxiety: A two-system framework. American Journal of Psychiatry, 173(11), 1083–1093. https://doi.org/10.1176/appi.ajp.2016.16030353
Lewis, C., Roberts, N. P., Andrew, M., Starling, E., & Bisson, J. I. (2020). Psychological therapies for post-traumatic stress disorder in adults: Systematic review and meta-analysis. European Journal of Psychotraumatology, 11(1), 1729633. https://doi.org/10.1080/20008198.2020.1729633
Malejko, K., Abler, B., Plener, P. L., & Straub, J. (2017). Neural correlates of psychotherapeutic treatment of post-traumatic stress disorder: A systematic literature review. Frontiers in Psychiatry, 8(85). https://doi.org/10.3389/fpsyt.2017.00085
Manthey, A., Sierk, A., Brakemeier, E.-L., Walter, H., & Daniels, J. K. (2021). Does trauma-focused psychotherapy change the brain? A systematic review of neural correlates of therapeutic gains in PTSD. European Journal of Psychotraumatology, 12(1), 1929025. https://doi.org/10.1080/20008198.2021.1929025
Merz, J., Schwarzer, G., & Gerger, H. (2019). Comparative efficacy and acceptability of pharmacological, psychotherapeutic, and combination treatments in adults with posttraumatic stress disorder: A network meta-analysis. JAMA Psychiatry, 76(9), 904–913. https://doi.org/10.1001/jamapsychiatry.2019.0951
Müller, V. I., Cieslik, E. C., Laird, A. R., Fox, P. T., Radua, J., Mataix-Cols, D., Tench, C. R., Yarkoni, T., Nichols, T. E., Turkeltaub, P. E., Wager, T. D., & Eickhoff, S. B. (2018). Ten simple rules for neuroimaging meta-analysis. Neuroscience and Biobehavioral Reviews, 84, 151–161. https://doi.org/10.1016/j.neubiorev.2017.11.012
Nichols, T. E., Das, S., Eickhoff, S. B., Evans, A. C., Glatard, T., Hanke, M., Kriegeskorte, N., Milham, M. P., Poldrack, R. A., Poline, J. B., Proal, E., Thirion, B., Van Essen, D. C., White, T., & Yeo, B. T. (2017). Best practices in data analysis and sharing in neuroimaging using MRI. Nature Neuroscience, 20(3), 299–303. https://doi.org/10.1038/nn.4500
Olff, M., Monson, C. M., Riggs, D. S., Lee, C., Ehlers, A., & Forbes, D. (2020). Psychological treatments: Core and common elements of effectiveness. In D. Forbes, J. I. Bisson, C. M. Monson, & L. Berliner (Eds.), Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies. Guildford Press.
Öst, L.-G. (2008). Efficacy of the third wave of behavioral therapies: A systematic review and meta-analysis. Behaviour Research and Therapy, 46(3), 296–321. https://doi.org/10.1016/j.brat.2007.12.005
Patel, R., Spreng, R. N., Shin, L. M., & Girard, T. A. (2012). Neurocircuitry models of posttraumatic stress disorder and beyond: A meta-analysis of functional neuroimaging studies. Neuroscience & Biobehavioral Reviews, 36(9), 2130–2142. https://doi.org/10.1016/j.neubiorev.2012.06.003
Peres, J. F., Foerster, B., Santana, L. G., Fereira, M. D., Nasello, A. G., Savoia, M., Moreira-Almeida, A., & Lederman, H. (2011). Police officers under attack: Resilience implications of an fMRI study. Journal of Psychiatric Research, 45(6), 727–734. https://doi.org/10.1016/j.jpsychires.2010.11.004
Radua, J., Mataix-Cols, D., Phillips, M. L., El-Hage, W., Kronhaus, D. M., Cardoner, N., & Surguladze, S. (2012). A new meta-analytic method for neuroimaging studies that combines reported peak coordinates and statistical parametric maps. European Psychiatry, 27(8), 605–611. https://doi.org/10.1016/j.eurpsy.2011.04.001
Radua, J., Rubia, K., Canales, E., Pomarol-Clotet, E., Fusar-Poli, P., & Mataix-Cols, D. (2014). Anisotropic kernels for coordinate-based meta-analyses of neuroimaging studies. Frontiers in Psychiatry, 5, 13. https://doi.org/10.3389/fpsyt.2014.00013
Rauch, S. L., Shin, L. M., & Phelps, E. A. (2006). Neurocircuitry models of posttraumatic stress disorder and extinction: Human neuroimaging research—past, present, and future. Biological Psychiatry, 60(4), 376–382. https://doi.org/10.1016/j.biopsych.2006.06.004
Rousseau, P. F., El Khoury-Malhame, M., Reynaud, E., Zendjidjian, X., Samuelian, J. C., & Khalfa, S. (2019). Neurobiological correlates of EMDR therapy effect in PTSD. European Journal of Trauma & Dissociation, 3(2), 103–111. https://doi.org/10.1016/j.ejtd.2018.07.001
Roydeva, M. I., & Reinders, A. (2021). Biomarkers of pathological dissociation: A systematic review. Neuroscience and Biobehavioral Reviews, 123, 120–202. https://doi.org/10.1016/j.neubiorev.2020.11.019
Schnyder, U., Ehlers, A., Elbert, T., Foa, E. B., Gersons, B. P. R., Resick, P. A., Shapiro, F., & Cloitre, M. (2015). Psychotherapies for PTSD: What do they have in common? European Journal of Psychotraumatology, 6(1), 28186. https://doi.org/10.3402/ejpt.v6.28186
Schottenbauer, M. A., Glass, C. R., Arnkoff, D. B., Tendick, V., & Gray, S. H. (2008). Nonresponse and dropout rates in outcome studies on PTSD: Review and methodological considerations. Psychiatry: Interpersonal and Biological Processes, 71(2), 134–168. https://doi.org/10.1521/psyc.2008.71.2.134
Schulze, L., Schulze, A., Renneberg, B., Schmahl, C., & Niedtfeld, I. (2019). Neural correlates of affective disturbances: A comparative meta-analysis of negative affect processing in borderline personality disorder, major depressive disorder, and posttraumatic stress disorder. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 4(3), 220–232. https://doi.org/10.1016/j.bpsc.2018.11.004
Shapiro, F. (2001). Eye movement desensitization and reprocessing (EMDR): Basic principles, protocols, and procedures. Guilford Press.
Simmons, A. N., Norman, S. B., Spadoni, A. D., & Strigo, I. A. (2013). Neurosubstrates of remission following prolonged exposure therapy in veterans with posttraumatic stress disorder. Psychotherapy and Psychosomatics, 82(6), 382–389. https://doi.org/10.1159/000348867
Suarez-Jimenez, B., Albajes-Eizagirre, A., Lazarov, A., Zhu, X., Harrison, B. J., Radua, J., Neria, Y., & Fullana, M. A. (2020). Neural signatures of conditioning, extinction learning, and extinction recall in posttraumatic stress disorder: A meta-analysis of functional magnetic resonance imaging studies. Psychological Medicine, 50(9), 1442–1451. https://doi.org/10.1017/S0033291719001387
Thomaes, K., Dorrepaal, E., Draijer, N., De Ruiter, M., Elzinga, B., Van Balkom, A., Smit, J., & Veltman, D. (2012). Treatment effects on insular and anterior cingulate cortex activation during classic and emotional Stroop interference in child abuse-related complex post-traumatic stress disorder. Psychological Medicine, 42(11), 2337–2349. https://doi.org/10.1017/S0033291712000499
Thomaes, K., Dorrepaal, E., Draijer, N., Jansma, E. P., Veltman, D. J., & van Balkom, A. J. (2014). Can pharmacological and psychological treatment change brain structure and function in PTSD? A systematic review. Journal of Psychiatric Research, 50, 1–15.
Thome, J., Terpou, B. A., McKinnon, M. C., & Lanius, R. A. (2020). The neural correlates of trauma-related autobiographical memory in posttraumatic stress disorder: A meta-analysis. Depression and Anxiety, 37(4), 321–345. https://doi.org/10.1002/da.22977
van Rooij, S. J. H., Kennis, M., Vink, M., & Geuze, E. (2016). Predicting Treatment Outcome in PTSD: A longitudinal functional MRI study on trauma-unrelated emotional processing. Neuropsychopharmacology, 41(4), 1156–1165. https://doi.org/10.1038/npp.2015.257
Weber, M., Schumacher, S., Hannig, W., Barth, J., Lotzin, A., Schäfer, I., Ehring, T., & Kleim, B. (2021). Long-term outcomes of psychological treatment for posttraumatic stress disorder: A systematic review and meta-analysis. Psychological Medicine, 51(9), 1420–1430. https://doi.org/10.1017/S003329172100163X
Wen, Z., Seo, J., Pace-Schott, E. F., & Milad, M. R. (2022). Abnormal dynamic functional connectivity during fear extinction learning in PTSD and anxiety disorders. Molecular Psychiatry. https://doi.org/10.1038/s41380-022-01462-5
Acknowledgements
This work was supported by the Stichting Steunfonds Joodse GGZ and Sinai Centrum, The Netherlands, as well as the Western Norway Regional Health Authority, Norway. We would like to thank Sophie M.D.D. Fitzsimmons for proofreading the manuscript.
Funding
This work was supported by the Stichting Steunfonds Joodse GGZ and Sinai Centrum, The Netherlands.
Author information
Authors and Affiliations
Contributions
Author contributions included conception and study design (all authors), literature search (CP and IA), deduplication of the search results (CP), study selection, data extraction and analyses (IA and ALT), interpretation of results (IA, ALT, CV, OAvdH, KT), drafting the manuscript work (IA and ALT), revising it critically for important intellectual content and approval of final version to be published and agreement to be accountable for the integrity and accuracy of all aspects of the work (all authors).
Corresponding author
Ethics declarations
Ethics approval
Not applicable
Consent to participate
Not applicable.
Consent for publication
Not applicable
Competing interests
The authors declare no competing interests.
Conflicts of interest
None of the authors have a conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
I. Aarts and A. L. Thorsen shared first authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Aarts, I., Thorsen, A.L., Vriend, C. et al. Effects of psychotherapy on brain activation during negative emotional processing in patients with posttraumatic stress disorder: a systematic review and meta-analysis. Brain Imaging and Behavior 18, 444–455 (2024). https://doi.org/10.1007/s11682-023-00831-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-023-00831-0