Abstract
Background
Mechanical outlet impingement is believed to be a significant factor in the pathogenesis of bursal-sided supraspinatus (SSP) tendon partial tear, a rare and poorly described entity. This relationship has not yet been confirmed.
Objective
We compared the radiological impingement parameters between complete, isolated SSP tears and bursal-sided SSP tears. The study hypothesis was that the impingement parameters in the bursal-sided SSP tear group would be significantly more pronounced.
Materials and methods
In total, 43 patients with bursal-sided SSP tendon partial tear (group 1; n = 43) and 43 patients with complete, isolated SSP tendon tear (group 2; n = 43) were included and matched for age (groups 1 and 2: 58 ± 9 years) and gender (70% male and 30% female patients). Standardized preoperative radiographs (anteroposterior; outlet view) were compared for radiological impingement parameters: critical shoulder angle (CSA), lateral acromial angle (LAA), acromiohumeral index (AHI), acromiohumeral distance (AHD), acromion type according to Bigliani (ATB).
Results
Radiological parameters did not differ significantly between groups: CSA: 36° ± 4° (group 1) and 36° ± 4° (group 2); LAA: 79° ± 6° vs. 80° ± 8°; AHD: 11 mm ± 2 mm vs. 10 mm ± 2 mm. The AHI was 0.7 ± 0.1 for both groups. Furthermore, ATB II was most common in both groups (group 1 = 74%; group 2 = 63%), followed by ATB I (group 1 = 14%; group 2 = 23%) and ATB III (group 1 = 12%; group 2 = 14%; p = 0.443).
Conclusion
We found no difference in radiological impingement parameters between bursal-sided and complete SSP tears and therefore reject the study hypothesis. Mechanical outlet impingement does not seem to play a greater role in the development of bursal-sided lesions compared to complete SSP lesions.
Zusammenfassung
Hintergrund
Das mechanische Outlet-Impingement (MOI) wird als ein bedeutender Faktor bei der Pathogenese von Partialrupturen der bursaseitigen Supraspinatussehne (SSP) betrachtet. Allerdings wurde dieser Zusammenhang bisher nicht bestätigt.
Ziel
Ziel der vorliegenden Arbeit war ein Vergleich der radiologischen Impingement-Parameter von Patienten mit vollständigen, isolierten SSP-Läsionen mit denen von Patienten mit bursaseitigen SSP-Läsionen. Die Studienhypothese bestand darin, dass die Impingement-Parameter in der Gruppe mit bursaseitigen SSP-Rupturen signifikant ausgeprägter sein würden.
Material und Methoden
In diese Studie wurden 43 Patienten mit bursaseitigen SSP-Partialläsionen (Gruppe 1; n = 43) und 43 Patienten mit vollständigen, isolierten Läsionen der SSP-Sehne (Gruppe 2; n = 43) einbezogen. Die Patienten wurden hinsichtlich des Alters (Gruppe 1 und 2: 58 ± 9 Jahre) und Geschlechts (70 % männlich, 30 % weiblich) gematcht. Die standardisierten präoperativen Röntgenaufnahmen (a.-p.- und Outlet-Aufnahme) wurden hinsichtlich folgender radiologischer Impingement-Parameter verglichen: kritischer Schulterwinkel (CSA), lateraler Akromialwinkel (LAA), Akromiohumeralindex (AHI), Akromiohumeralabstand (AHD) und Akromiontyp nach Bigliani (ATB).
Ergebnisse
Die radiologischen Parameter unterschieden sich nicht signifikant (p = 0,371): Der CSA betrug 36° ± 4° in Gruppe 1 und 36° ± 4° in Gruppe 2. Der LAA betrug 79° ± 6° vs. 80° ± 8° in Gruppe 1 und 2, der AHD betrug 11 mm ± 2 mm vs. 10 mm ± 2 mm, und der AHI lag bei 0,70 ± 0,1 in beiden Gruppen. Ein ATB II war der häufigste beobachtete Typ in beiden Gruppen (Gruppe 1 = 74 %, Gruppe 2 = 63 %), gefolgt von ATB I (Gruppe 1 = 14 %, Gruppe 2 = 23 %) und ATB III (Gruppe 1 = 12 %, Gruppe 2 = 14 %). Dieser Unterschied war statistisch nicht signifikant (p = 0,443).
Schlussfolgerung
Es fand sich kein Unterschied in den radiologischen Impingement-Parametern zwischen bursaseitigen und vollständigen SSP-Läsionen, daher verwerfen die Autoren die Studienhypothese. MOI scheint keine größere Rolle bei der Entwicklung von bursaseitigen im Vergleich zu vollständigen SSP-Läsionen zu spielen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The bursal-sided partial tear of the supraspinatus (SSP) tendon is a rare entity that has not been described in detail in the literature and its pathomechanism is still the subject of debate. A multifactorial etiology with a combination of extrinsic and intrinsic pathomechanisms is assumed.
Neer et al. suggested early on a connection between subacromial abrasion of the SSP tendon, its wear and tear, and subsequent rupture and thus they propagated the theory of the extrinsic pathomechanisms of rotator cuff tears (RCTs; [1]). This pathogenesis, initially described by Neer, is due to the so-called mechanical outlet or subacromial impingement (MOI). The MOI, also known as the “classic impingement syndrome,” is described as a mechanical narrowing of the subacromial space by extratendinous elements [2]. This structural constriction can be caused by anterolateral acromial spurs, osteophytes under the acromioclavicular joint (ACJ), or posttraumatic malpositions of the greater tubercle [1]. Neer et al. postulated that 100% of impingement syndromes and 95% of rotator cuff pathologies are the result of an MOI [1].
Codman suggested that RCTs are the consequence of degenerative intratendinous (intrinsic) changes [3]. These intrinsic mechanisms describe degenerative processes within the tendon itself that develop over time due to wear and tear, stress, or trauma. Genetic and pathological studies provide evidence that intrinsic factors play a role, but little is known about the specific extent of the involvement of these factors in RCTs [4,5,6].
It is assumed that full-thickness RCTs result from the progression of partial ruptures of the rotator cuff [6]. This hypothesis was also supported by studies using biomechanical models of impingement [7]. Yamanaka et al. showed that after 1 year, 28% of partial ruptures progressed to full-thickness ruptures and 80% increased in size [8]. Other authors also described progression, but to a lesser extent [9, 10]. However, the progression of partial ruptures to full-thickness ruptures seems to depend on the degree of rupture [9].
Subacromial impingement of the SSP tendon due to MOI and its involvement in the pathogenesis of SSP tears in general was a frequently reported occurrence in the past. However, the literature has been conflicting regarding the strength of the association between radiological parameters in the pathogenesis of SSP tears. Furthermore, to date there is only limited evidence supporting the association between bursal-sided partial tears of the SSP tendon and radiological parameters of MOI. The aim of this study was therefore to expand the previous scientific evidence on the bursal-sided partial tear of the SSP tendon in connection with the MOI.
Materials and methods
The acquisition of patient data was carried out from October 2014 to November 2020 at the ATOS Clinic Heidelberg and ATOS Clinic Munich. In total, 43 patients with a bursal-sided partial tear of the SSP tendon (group 1) were matched with 43 patients with a complete, isolated tear of the SSP tendon (group 2). Matching criteria were age and sex. The group allocation was based on rupture type (Table 1), which was classified intraoperatively.
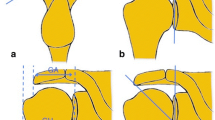
The standardized preoperative radiographs (anteroposterior and outlet view) were compared with regard to the following radiological impingement parameters (Fig. 1):
-
Critical shoulder angle (CSA)
-
Lateral acromial angle (LAA)
-
Acromial index (AI)
-
Acromiohumeral distance (AHD)
-
Acromion type according to Bigliani (ATB)
Radiographs were evaluated by a blinded examiner. To assess intrarater reliability, the same radiographs were reassessed by the same blinded person 3 months after the initial evaluation. To assess interrater reliability, the radiographs were analyzed by another blinded, independent examiner.
The CSA, LAA, and AHI were measured as described by Moor et al. [11], Banas et al. [12], and Nyffeler et al. [13], respectively, in true anteroposterior radiographs. The AHD was defined as the perpendicular distance from a line passing through the inferior border of the acromion to the most cranial point of the humeral head. Acromial shapes were assigned using the Bigliani et al. classification on outlet-view radiographs [14].
Statistical analysis
All statistical analyses were performed using SPSS version 29.0 (SPSS Inc., Chicago, IL, USA). First, all data were tested for normality using the Kolmogorov–Smirnov test. Descriptive analysis was used to evaluate various metric and nominal variables, as well as to calculate means and standard deviations. The comparison of categorical variables (acromion type) was carried out using the chi-square test. Continuous variables (CSA, LAA, AHD, AHI) were compared using the Mann–Whitney U test. Inter- and intrarater reliability was determined for continuous variables (CSA, LAA, AHD, AHI) using the intraclass correlation coefficient as well as using Cohen’s kappa for categorical variables (acromion type). Statistical significance was defined as p ≤ 0.05.
Results
Our study collective was made up of 70% male (n = 60) and 30% female (n = 26) patients. The average age of the patients at the time of surgery was 57.8 years (SD ± 9). Means of radiological impingement parameters for groups 1 and 2 with standard deviations and 95% confidence intervals are presented in Table 2. No statistically significant differences were found between groups 1 and 2 when comparing CSA, LAA, AHD, and AHI (Table 2). The distribution of the acromion types according to Bigliani is shown in Table 3. The same order of acromion type distribution was observed in group 1 and in group 2, but with a slight nonstatistically significant difference in frequency (p = 0.443).
The intra- and interrater reliability for CSA, LAA, AHD, AHI, and ATB were excellent (p < 0.001).
Discussion
In this study, the type II acromion was the most common acromion type in both groups. These results are consistent with the findings of most other studies on this subject [15,16,17]. Few studies have investigated the acromion type according to Bigliani (ATB) in partial tears. Kaur et al. found no relationship between tear type and acromion type, although they did not differentiate between bursal- and articular-sided partial lesions [18]. Only our study and the study by Pandey et al. provide information on Bigliani’s acromial type in bursal-sided partial tears of the SSP tendon [19]. Our results showed no significant difference in the frequency distribution of the ATB between group 1 and group 2. Pandey et al. also found no relationship between the ATB and tear type. Our study, as well as the work of Pandey et al., suggests that the Bigliani classification is not a parameter suitable for differentiating between the two tear types.
Since the introduction of the critical shoulder angle (CSA) in 2013, a frequent correlation has been found between an increased angle and full-thickness RCTs [11, 20,21,22,23,24,25,26,27]. Cunningham et al. showed that a large CSA was associated with full-thickness RCTs but not with partial tears [23]. Seo et al. showed in a retrospective analysis that a high CSA was more associated with full-thickness tears and articular-sided partial tears than with bursal-sided partial tears. They found a significant difference in CSA between the bursal group with 31.5° ± 4.6° compared to 34.7° ± 4.4° in the full-thickness tear group (p = 0.001; [28]). Pandey et al. found no significant difference in CSA between bursal and full-thickness RCTs [19]. Our results also showed no statistically significant difference in CSA between group 1 and group 2. The CSA of our patients was on average slightly above the cut-off value initially defined by Moor et al. Lin et al. described a CSA of 36° on average in 300 patients without RCTs. The CSA in both of our groups, as well as that in the study by Seo et al., is on average below the values described in other studies on RCTs and CSA [19, 26, 29]. This suggests that CSA is not associated with RCTs to the extent reported by other authors.
The correlation between a narrowing of the acromiohumeral distance, measured through AHD, and RCTs has been extensively described in the literature [30,31,32]. The cause of the narrowing is a traction movement of the humeral head with displacement in the glenoid, due to cranial pull by the deltoid muscle in combination with failure of the superior rotator cuff [32, 33]. Traditionally AHD has been determined primarily by X‑rays [34, 35]. However, the radiographically measured AHD is not a reliable parameter for the true acromiohumeral distance, according to a review [36]. Our results showed very good inter- and intrarater reliability. There is little information in the literature about partial tears and AHD. In a study by Kaur et al., patients with full-thickness and partial-thickness tears had a smaller AHD than the control group without tears [18]. Both groups in our study had a similar AHD with values that were higher than those previously described in tear groups and are similar to those in healthy patients [18, 30, 35]. To our knowledge, our results provide the first data on AHD in bursal-sided partial tears of the SSP tendon.
The LAA was introduced by Banas et al. in 1995, who identified a correlation between a small LAA and the risk of impingement syndrome [12]. Since then, this association has been reported by other authors as well [16, 26, 37]. In their initial study of the LAA, Banas et al. described an angle of > 80° in asymptomatic patients, with patients with impingement syndrome symptoms showing a lower angle. In this study, patients with complete and partial ruptures were examined, and all patients with an LAA < 70° had complete RCTs [12]. In a few studies, RCTs were associated with an angle of < 70°, leading some authors to present the LAA as an independent factor for RCTs [12, 16]. Our study showed no difference in the LAA between patients with partial and complete lesions. Furthermore, both groups had an average LAA of about 80° despite the presence of an RCT. Therefore, our results did not support the LAA as a factor for RCTs.
Nyffeler et al. were the first to describe the association between RCTs and an increased acromiohumeral index (AHI; [13]). Although this initial observation was made on magnetic resonance images, it has since been shown that the AHI can also be applied to X‑rays [12, 16, 38]. This association has been confirmed multiple times in the literature [39,40,41,42]. In these studies, the average AHI in patients with RCTs was 0.73, and 0.67 in the control group with an intact rotator cuff. In their comparison of patients with complete RCTs with healthy patients, Moor et al. established an AHI cut-off value of 0.68 [26]. Torrens et al. also showed an association between a large AHI and RCT in a study of 148 patients [41]. However, there is also literature that argues against the association between AHI and RCTs. Several authors found no correlation between AHI and RCT [40, 43, 44]. Lin et al. reported an increased AHI of an average of 0.77 in patients with intact rotator cuffs [44]. Other authors have examined the difference in AHI between different types of RCT. Kim et al. found a larger AHI in patients with complete RCTs than in those with articular-sided RCTs [39]. In 2016, Balke et al. described a difference in AHI between patients with degenerative and traumatic RCTs. Patients with degenerative tears had a significantly greater acromial roofing than those with traumatic tears [45]. To our knowledge, there is only one study to date that has compared AHI between complete and bursal-sided partial tears. Pandey et al. found no statistically significant difference in AHI between complete and bursal-sided partial tears [19]. Our results are in line with those of Pandey et al., as no significant difference in AHI was found between group 1 and group 2.
Interestingly, the primary hypothesis could not be confirmed. Our study showed that CSA, LAA, AHD, and AHI are not suitable parameters for differentiating between bursal-sided partial lesions and complete ruptures of the SSP tendon. This suggests a relationship between the two rupture types and supports the hypothesis of bursal-sided partial lesions as a precursor to complete supraspinatus tendon rupture. In addition, our results suggest that radiological impingement parameters are not a useful diagnostic tool for differentiating these two types of RCTs. We showed that the impingement parameters CSA, LAA, and AHD, which are frequently described in the literature, do not differ significantly from the healthy normal values described in the literature. This suggests that contrary to the often-described assumption in the literature in the past, acromion morphology and MOI are not the only primarily causative factors for supraspinatus tendon ruptures. Our results are supported by the clinical evidence of some authors in which anterior subacromial decompression did not lead to symptom relief and did not reduce the risk of re-rupture or rupture progression [46,47,48,49,50,51,52,53,54,55,56,57,58,59]. Involvement of MOI in the pathogenesis cannot be excluded, but our results support the assumption of a multifactorial pathogenesis of RCTs, with intrinsic and extrinsic factors, and reduce the importance of the influence of MOI.
Limitations
Routine radiographs were utilized in the study. Despite standardization, factors such as the positioning of the patient, the X‑ray tube, and the plate can influence the reliability of the images. Our study did not differentiate between degenerative and traumatic rotator cuff ruptures. Further, in this work, we did not distinguish between chronic, acute, or acute-on-chronic supraspinatus tendon ruptures.
Practical conclusion
-
Our study revealed no significant difference in the radiological impingement signs—critical shoulder angle, lateral acromial angle, acromiohumeral distance, acromiohumeral index, and acromion type according to Bigliani—between patients with partial tears on the bursal side and those with complete tears of the supraspinatus tendon.
-
We thus conclude that scapular anatomy alone, as assessed by radiological impingement signs, is insufficient to distinguish between the two types of ruptures.
-
Our results also suggest a reduced influence of mechanical outlet impingement on the pathogenesis of rotator cuff tears (RCTs), and thus offer supporting evidence of a multifactorial pathogenesis of RCTs involving extrinsic and intrinsic mechanisms.
-
Our findings are relevant for patient communication but they also add to a more concise understanding of factors predisposing to success/failure of rotator cuff repair in the community of sports medicine physicians and healthcare providers.
References
Neer CS (1972) Anterior acromioplasty for the chronic impingement syndrome in the shoulder: a preliminary report. J Bone Joint Surg Am. https://doi.org/10.2106/00004623-197254010-00003
Bigliani LU, Levine WN (1997) Current concepts review. Subacromial impingement syndrome. J Bone Joint Surg Am 79(12):79A. https://doi.org/10.2106/00004623-199712000-00012
Codman E (1934) Tendinitis of the short rotators. The shoulder rupture of the suprasìnatus tendon and other lesions in or about the subacromial bursa. Thomas Todd, Boston
Harvie P et al (2004) Genetic influences in the aetiology of tears of the rotator cuff. J Bone Joint Surg Br. https://doi.org/10.1302/0301-620x.86b5.14747
Hashimoto T, Nobuhara K, Hamada T (2003) Pathologic evidence of degeneration as a primary cause of rotator cuff tear. Clin Orthop Relat Res. https://doi.org/10.1097/01.blo.0000092974.12414.22
Uhthoff HK, Sano H (1997) Pathology of failure of the rotator cuff tendon. Orthop Clin North Am. https://doi.org/10.1016/S0030-5898(05)70262-5
Yang S et al (2009) Biomechanical analysis of bursal-sided partial thickness rotator cuff tears. J Shoulder Elbow Surg. https://doi.org/10.1016/j.jse.2008.12.011
Yamanaka K, Matsumoto T (1994) The joint side tear of the rotator cuff: a followup study by arthrography. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-199407000-00012
Lo IK, Denkers MR, More KD, Nelson AA, Thornton GM, Boorman RS (2018) Partial-thickness rotator cuff tears: clinical and imaging outcomes and prognostic factors of successful nonoperative treatment. Open Access J Sports Med. https://doi.org/10.2147/oajsm.s153236
Ranebo MC, Björnsson Hallgren HC, Norlin R, Adolfsson LE (2017) Clinical and structural outcome 22 years after acromioplasty without tendon repair in patients with subacromial pain and cuff tears. J Shoulder Elbow Surg. https://doi.org/10.1016/j.jse.2016.11.012
Moor BK, Bouaicha S, Rothenfluh DA, Sukthankar A, Gerber C (2013) Is there an association between the individual anatomy of the scapula and the development of rotator cuff tears or osteoarthritis of the glenohumeral joint? A radiological study of the critical shoulder angle. Bone Joint J. https://doi.org/10.1302/0301-620X.95B7.31028
Banas MP, Miller RJ, Totterman S (1995) Relationship between the lateral acromion angle and rotator cuff disease. J Shoulder Elbow Surg. https://doi.org/10.1016/S1058-2746(05)80038-2
Nyffeler RW, Werner CML, Sukthankar A, Schmid MR, Gerber C (2006) Association of a large lateral extension of the acromion with rotator cuff tears. J Bone Joint Surg Am. https://doi.org/10.2106/JBJS.D.03042
Bigliani LU, Morrison DS, April EW (1986) The morphology of the acromion and its relationship to rotator cuff tears. Ortho Trans. https://doi.org/10.7205/milmed.171.10.1035
Ames JB, Horan MP, Van der Meijden OAJ, Leake MJ, Millett PJ (2012) Association between acromial index and outcomes following arthroscopic repair of full-thickness rotator cuff tears. J Bone Joint Surg Am. https://doi.org/10.2106/JBJS.K.01500
Balke M, Schmidt C, Dedy N, Banerjee M, Bouillon B, Liem D (2013) Correlation of acromial morphology with impingement syndrome and rotator cuff tears. Acta Orthop. https://doi.org/10.3109/17453674.2013.773413
Nicholson GP, Goodman DA, Flatow EL, Bigliani LU (1996) The acromion: morphologic condition and age-related changes. A study of 420 scapulas. J Shoulder Elbow Surg. https://doi.org/10.1016/S1058-2746(96)80024-3
Kaur R, Dahuja A, Garg S, Bansal K, Garg RS, Singh P (2019) Correlation of acromial morphology in association with rotator cuff tear: a retrospective study. Pol J Radiol. https://doi.org/10.5114/pjr.2019.90277
Pandey V et al (2016) Does scapular morphology affect the integrity of the rotator cuff? J Shoulder Elbow Surg. https://doi.org/10.1016/j.jse.2015.09.016
Blonna D et al (2016) Predominance of the critical shoulder angle in the pathogenesis of degenerative diseases of the shoulder. J Shoulder Elbow Surg. https://doi.org/10.1016/j.jse.2015.11.059
Chalmers PN, Salazar D, Steger-May K, Chamberlain AM, Yamaguchi K, Keener JD (2017) Does the critical shoulder angle correlate with rotator cuff tear progression? Clin Orthop Relat Res. https://doi.org/10.1007/s11999-017-5249-1
Cherchi L, Ciornohac JF, Godet J, Clavert P, Kempf JF (2016) Critical shoulder angle: measurement reproducibility and correlation with rotator cuff tendon tears. Orthop Traumatol Surg Res. https://doi.org/10.1016/j.otsr.2016.03.017
Cunningham G, Nicodème-Paulin E, Smith MM, Holzer N, Cass B, Young AA (2018) The greater tuberosity angle: a new predictor for rotator cuff tear. J Shoulder Elbow Surg. https://doi.org/10.1016/j.jse.2018.02.051
Daggett M, Werner B, Collin P, Gauci MO, Chaoui J, Walch G (2015) Correlation between glenoid inclination and critical shoulder angle: a radiographic and computed tomography study. J Shoulder Elbow Surg. https://doi.org/10.1016/j.jse.2015.07.013
Gomide LC, do Carmo TC, Bergo GHM, Oliveira GA, Macedo IS (2017) Relationship between the critical shoulder angle and the development of rotator cuff lesions: a retrospective epidemiological study. Rev Bras Ortop (Sao Paulo). https://doi.org/10.1016/j.rboe.2017.06.002
Moor BK, Wieser K, Slankamenac K, Gerber C, Bouaicha S (2014) Relationship of individual scapular anatomy and degenerative rotator cuff tears. J Shoulder Elbow Surg. https://doi.org/10.1016/j.jse.2013.11.008
Shinagawa K et al (2018) Critical shoulder angle in an East Asian population: correlation to the incidence of rotator cuff tear and glenohumeral osteoarthritis. J Shoulder Elbow Surg. https://doi.org/10.1016/j.jse.2018.03.013
Seo J, Heo K, Kwon S, Yoo J (2019) Critical shoulder angle and greater tuberosity angle according to the partial thickness rotator cuff tear patterns. Orthop Traumatol Surg Res. https://doi.org/10.1016/j.otsr.2019.05.005
Spiegl UJ, Horan MP, Smith SW, Ho CP, Millett PJ (2016) The critical shoulder angle is associated with rotator cuff tears and shoulder osteoarthritis and is better assessed with radiographs over MRI. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-015-3587-7
Cotty P et al (1988) Rupture of the rotator cuff. Quantification of indirect signs in standard radiology and the Leclercq maneuver. J Radiol
Neer CS (1983) Impingement lesions. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-198303000-00010
Weiner DS, Macnab I (1970) Superior migration of the humeral head. J Bone Joint Surg Br 52(3):524–527. https://doi.org/10.1302/0301-620X.52B3.524
Nové-Josserand L, Boulahia A, Levigne C, Noel E, Walch G (1999) Espace coraco-humeral et rupture de la coiffe des rotateurs de l’epaule. Rev Chir Orthop Reparatrice Appar Mot. https://doi.org/10.1016/b978-2-294-71318-7.00020-4
Kum DH, Kim JH, Park KM, Lee ES, Park YB, Yoo JC (2017) Acromion index in korean population and its relationship with rotator cuff tears. Clin Orthop Surg. https://doi.org/10.4055/cios.2017.9.2.218
Saupe N, Pfirrmann CWA, Schmid MR, Jost B, Werner CML, Zanetti M (2006) Association between rotator cuff abnormalities and reduced acromiohumeral distance. AJR Am J Roentgenol. https://doi.org/10.2214/AJR.05.0435
McCreesh KM, Crotty JM, Lewis JS (2015) Acromiohumeral distance measurement in rotator cuff tendinopathy: Is there a reliable, clinically applicable method? A systematic review. Br J Sports Med. https://doi.org/10.1136/bjsports-2012-092063
Singleton N, Agius L, Andrews S (2017) The acromiohumeral centre edge angle: a new radiographic measurement and its association with rotator cuff pathology. J Orthop Surg. https://doi.org/10.1177/2309499017727950
Tétreault P, Krueger A, Zurakowski D, Gerber C (2004) Glenoid version and rotator cuff tears. J Orthop Res 22(1):202–207. https://doi.org/10.1016/S0736-0266(03)00116-5
Kim JR, Ryu KJ, Hong IT, Kim BK, Kim JH (2012) Can a high acromion index predict rotator cuff tears? Int Orthop. https://doi.org/10.1007/s00264-012-1499-4
Miyazaki AN et al (2011) Comparison between the acromion index and rotator cuff tears in the Brazilian and Japanese populations. J Shoulder Elbow Surg. https://doi.org/10.1016/j.jse.2011.04.028
Torrens C, López JM, Puente I, Cáceres E (2007) The influence of the acromial coverage index in rotator cuff tears. J Shoulder Elbow Surg. https://doi.org/10.1016/j.jse.2006.07.006
Zumstein MA, Jost B, Hempel J, Hodler J, Gerber C (2008) The clinical and structural long-term results of open repair of massive tears of the rotator cuff. J Bone Joint Surg Am. https://doi.org/10.2106/JBJS.G.00677
Hamid N, Omid R, Yamaguchi K, Steger-May K, Stobbs G, Keener JD (2012) Relationship of radiographic acromial characteristics and rotator cuff disease: a prospective investigation of clinical, radiographic, and sonographic findings. J Shoulder Elbow Surg. https://doi.org/10.1016/j.jse.2011.09.028
Lin CL, Chen YW, Lin LF, Chen CP, Liou TH, Huang SW (2020) Accuracy of the critical shoulder angle for predicting rotator cuff tears in patients with nontraumatic shoulder pain. Orthop J Sports Med. https://doi.org/10.1177/2325967120918995
Balke M, Liem D, Greshake O, Hoeher J, Bouillon B, Banerjee M (2016) Differences in acromial morphology of shoulders in patients with degenerative and traumatic supraspinatus tendon tears. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-014-3499-y
Hyvönen P, Lohi S, Jalovaara P (1998) Open acromioplasty does not prevent the progression of an impingement syndrome to a tear. Nine-year follow-up of 96 cases. J Bone Joint Surg Br. https://doi.org/10.1302/0301-620X.80B5.8533
Bond EC et al (2017) The role of acromioplasty when repairing rotator cuff tears—no difference in pain or functional outcome at 24 months in a cohort of 2,441 patients. N Z Med J. https://doi.org/10.2106/jbjs.22.01019
Chahal J et al (2012) The role of subacromial decompression in patients undergoing arthroscopic repair of full-thickness tears of the rotator cuff: a systematic review and meta-analysis. Arthroscopy. https://doi.org/10.1016/j.arthro.2011.11.022
Ketola S et al (2009) Does arthroscopic acromioplasty provide any additional value in the treatment of shoulder impingement syndrome? A two-year randomised controlled trial. J Bone Joint Surg Br. https://doi.org/10.1302/0301-620X.91B10.22094
Ketola S, Lehtinen J, Elo P, Kortelainen S, Huhtala H, Arnala I (2016) No difference in long-term development of rotator cuff rupture and muscle volumes in impingement patients with or without decompression: a randomized MRI study of 140 patients. Acta Orthop. https://doi.org/10.1080/17453674.2016.1177780
Kolk A et al (2017) Does acromioplasty result in favorable clinical and radiologic outcomes in the management of chronic subacromial pain syndrome? A double-blinded randomized clinical trial with 9 to 14 years’ follow-up. J Shoulder Elbow Surg. https://doi.org/10.1016/j.jse.2017.03.021
Mardani-Kivi M, Karimi A, Keyhani S, Hashemi-Motlagh K, Saheb-Ekhtiari K (2016) Rotator cuff repair: is there any role for acromioplasty? Phys Sportsmed. https://doi.org/10.1080/00913847.2016.1216717
Paloneva J, Lepola V, Karppinen J, Ylinen J, Äärimaa V, Mattila VM (2015) Declining incidence of acromioplasty in Finland. Acta Orthop. https://doi.org/10.3109/17453674.2014.977703
Saltychev M, Äärimaa V, Virolainen P, Laimi K (2015) Conservative treatment or surgery for shoulder impingement: systematic review and meta-analysis. Disabil Rehabil. https://doi.org/10.3109/09638288.2014.907364
Shin SJ, Oh JH, Chung SW, Song MH (2012) The efficacy of acromioplasty in the arthroscopic repair of small- to medium-sized rotator cuff tears without acromial spur: prospective comparative study. Arthroscopy. https://doi.org/10.1016/j.arthro.2011.10.016
Cordasco FA, Backer M, Craig EV, Klein D, Warren RF (2002) The partial-thickness rotator cuff tear: is acromioplasty without repair sufficient? Am J Sports Med. https://doi.org/10.1177/03635465020300021801
Ellman H (1990) Diagnosis and treatment of incomplete rotator cuff tears. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-199005000-00010
Eraghi A (2020) Acromioplasty in the surgical operations of partial-thickness rotator cuff tears: a comprehensive review. J Family Med Prim Care. https://doi.org/10.4103/jfmpc.jfmpc_870_19
Itoi E, Tabata S (1992) Incomplete rotator cuff tears: results of operative treatment. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-199211000-00016
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by SF. The first draft of the manuscript was written by SF and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
S. Fromm, S. Lichtenberg, M. Loew, P. Habermeyer and M. Schnetzke declare that they have no competing interests.
The study was in agreement with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.

Scan QR code & read article online
Rights and permissions
About this article
Cite this article
Fromm, S., Lichtenberg, S., Loew, M. et al. Are bursal-sided supraspinatus tendon lesions caused by subacromial impingement?. Obere Extremität 19, 126–132 (2024). https://doi.org/10.1007/s11678-024-00795-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11678-024-00795-7