Abstract
Background
There is a paucity of literature demonstrating which factors are associated with signs of elbow instability on magnetic resonance imaging (MRI) following simple elbow dislocations (SED).
Objectives
This study aimed to evaluate demographic variables and MRI datasets to identify factors associated with elbow instability following SEDs.
Materials and methods
This retrospective multicenter MRI study included patients who had sustained SED and presented within 21 days of trauma. Measurements included ulnohumeral angle, drop sign, and radiocapitellar and ulnohumeral incongruity. The coronoid tip (Regan Morrey type I), lateral collateral ligament (LCL), common extensor origin (CEO), medial collateral ligament (MCL,) and common flexor origin (CFO) were assessed for injuries. Simple and multiple logistic regression analyses were performed to identify factors associated with signs of elbow instability (e.g., ulnohumeral incongruity > 1 mm) on MRI.
Results
A total of 147 patients (68 women, 79 men) with a mean age of 42.9 years (range, 17–85) were included. Of those, 62 patients (42.2%) demonstrated radiocapitellar (> 2 mm) and 36 patients (25.5%) demonstrated ulnohumeral incongruity (> 1 mm); 17 patients (11.6%) had a drop sign (≥ 4 mm). All patients with elbow instability on MRI had injury to the CEO and/or CFO. In multiple logistic regression, an ulnohumeral angle of ≤ 45° (p = 0.005; OR: 4.95), injury to the CEO (p < 0.001; OR: 10.45), CFO (p < 0.001; OR: 8.38), and coronoid tip (p = 0.002; OR: 5.32) were significantly associated with signs of elbow instability on MRI.
Conclusion
Injury to the CEO, CFO, and coronoid tip as well as an ulnohumeral angle of ≤ 45° are associated with signs of elbow instability on MRI following SEDs. If the CEO or CFO is injured, the odds for instability on MRI are increased by a factor of 10 and 8, respectively.
Zusammenfassung
Hintergrund
Wenige Untersuchungen beschäftigen sich mit der Frage, welche Faktoren mit Zeichen der Instabilität in der Magnetresonanztomographie (MRT) nach akuten, einfachen Ellenbogenluxationen vergesellschaftet sind.
Ziel der Arbeit
Ziel der Arbeit war es, demografische Daten und MRT-Datensätze auszuwerten, um Faktoren zu identifizieren, die mit einer Instabilität nach akuten, einfachen Ellenbogenluxationen einhergehen.
Material und Methoden
Patienten, die eine akute, einfache Ellenbogenluxationen erlitten und innerhalb von 21 Tagen mit MRT vorstellig wurden, wurden in diese retrospektive Multizenterstudie eingeschlossen. Der ulnohumerale Winkel, das „drop sign“, radiocapitellare und ulnohumerale Inkongruenz wurden gemessen. Die Koronoidspitze (Regan-Morrey-Typ I), das laterale (LCL) und mediale Kollateralband (MCL) sowie der Extensoren- (CEO) und Flexorenansatz (CFO) wurden auf Verletzungen geprüft. Einfache und multivariate logistische Regression wurden durchgeführt, um zu identifizieren, welche Variablen mit Ellenbogeninstabilität in der MRT (ulnohumerale Inkongruenz > 1 mm) einhergehen.
Ergebnisse
Insgesamt 147 Patienten (68 Frauen, 79 Männer) mit einem Durchschnittsalter von 42,9 Jahren (17–85 Jahre) wurden in die Auswertung einbezogen. Davon zeigten 62 Patienten (42,2 %) radiocapitellare Inkongruenz (> 2 mm), 36 Patienten (25,5 %) zeigten ulnohumerale Inkongruenz (> 1 mm) und 17 Patienten (11,6 %) wiesen ein „drop sign“ (≥ 4 mm) auf. Alle Patienten mit Ellenbogeninstabilität in der MRT hatten Verletzungen des CEO und/oder CFO. Variablen, die sich in der einfachen logistischen Regression als signifikant erwiesen, wurden in ein multivariates logistisches Modell übertragen. Hier blieben ein ulnohumeraler Winkel ≤ 45° (p = 0,005; Odds Ratio, OR: 4,95), Verletzungen des CEO (p < 0,001; OR: 10,45), CFO (p < 0,001; OR: 8,38) und der Koronoidspitze (p = 0,002; OR: 5,32) signifikant mit Zeichen von Ellenbogeninstabilität in der MRT vergesellschaftet.
Schlussfolgerung
Verletzungen des CEO, CFO, der Koronoidspitze und ein ulnohumeraler Winkel von ≤ 45° sind signifikant mit Zeichen von Ellenbogeninstabilität in der MRT nach akuten, einfachen Ellenbogenluxationen vergesellschaftet. Ist der CEO oder CFO verletzt, so erhöht sich das Risiko für Instabilität in der MRT um den Faktor 10 bzw. 8.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Simple elbow dislocations (SEDs) are defined as ligamentous injuries without major bony involvement [16], as opposed to complex dislocations with concomitant fractures about the elbow [15]. Of these two entities, complex elbow dislocations are believed to be more severe, and operative treatment is usually recommended [12, 27]. On the other hand, SEDs generally respond well to nonoperative management [4, 20]. However, following initial nonoperative management, one third of patients report a mild-to-moderate decrease in range of motion [16] and 8% of patients report symptoms of persistent instability [4, 19].
Therefore, SEDs are not entirely “simple” but complex soft-tissue injuries with a broad spectrum of anatomic structures involved, namely, the lateral collateral ligament complex (LCL), the medial collateral ligament complex (MCL), anterior and posterior capsule, and musculotendinous structures such as the common extensor origin (CEO) and common flexor origin (CFO; [18, 21, 22, 28, 35]).
In order to derive optimal treatment strategies and select patients who may benefit from operative management, further classification of these multifaceted injuries is important. A common subclassification of SEDs is based on elbow stability [28]. Some authors favor dynamic fluoroscopy following initial reduction of the joint to assess elbow stability [30,31,32]; however, the results of this are not always available to the treating physician, may rely on the examiner’s experience [28], and interpretation has been shown to be somewhat challenging [32]. Plain radiographs and computed tomography may show signs of instability such as radiocapitellar and ulnohumeral incongruity (e.g., “drop sign”; [7, 13]) and are more reproducible compared to dynamic fluoroscopy, but these modalities are static in nature and soft-tissue injuries cannot be assessed. Magnetic resonance imaging (MRI) on the other hand has superior soft-tissue contrast [1], is highly-accurate for detecting injury to both static and dynamic stabilizers of the elbow [6], and has shown high concordance with intraoperative findings [12]. Numerous studies have used MRI to assess injury patterns following SEDs [6, 9, 12, 18, 33,34,35] and recently Hackl et al. [13, 14] proposed criteria on MRI that are highly suggestive of elbow instability. However, there is a paucity of literature demonstrating which structures need to be injured in order to render an SED unstable on MRI.
Therefore, the purpose of this study was to evaluate demographic variables and MRI datasets to assess factors associated with signs of elbow instability following SEDs. We hypothesized that injury to the common extensor and/or common flexor origins is associated with signs of elbow instability on MRI.
Materials and methods
In this retrospective multicenter study performed at four institutions, patients were eligible for inclusion if they had sustained an SED (e.g., no osseous injuries despite Regan and Morrey type I coronoid process avulsions) that was confirmed on plain radiographs necessitating reduction and presented with a recent MRI of their injured elbow between April 2006 and November 2020. For this purpose, databases of the participating clinics were searched for patients who had sustained an SED. Images of eligible patients were then screened for availability of plain elbow radiographs documenting dislocation and recent elbow MRIs. Exclusion criteria were
-
1.
Skeletally immature patients aged less than 16 years
-
2.
An interval from injury to MRI longer than 21 days
-
3.
Insufficient MRI quality or incomplete imaging
-
4.
A dislocated joint at the time of MRI
Demographic and radiographic variables
Patient charts were examined for demographic variables including age, sex, injured side, and time from injury until MRI. All included patients underwent MRI with scanners of minimum 1.5 T with specific elbow surface coils. Coronal, axial, and sagittal images with non-fat-saturated T1-weighted and proton density-weighted sequences as well as short tau inversion recovery (STIR) sequences or fat-saturated T2/proton density-weighted were available for all patients.
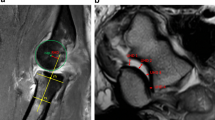
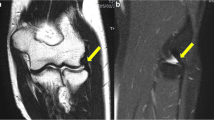
Measurements and injury assessments on MRI were performed using digital tools in Agfa IMPAX EE (Agfa Health Care, Mortsel, Belgium). Measurements included the following: ulnohumeral angle (< 45° vs. ≥ 45°) and drop sign (< 4 mm vs. ≥ 4 mm) according to Coonrad et al. [7] on sagittal images through the coronoid process (Fig. 1), radiocapitellar incongruity (in mm) on sagittal images through the center of the radial head, and ulnohumeral incongruity (in mm) on axial images through the motion axis of the distal humerus according to Hackl et al. (Fig. 2; [14]).
Magnetic resonance images in the sagittal plane following simple elbow dislocation demonstrating measurement of the ulnohumeral angle and drop sign. a Measurement of the ulnohumeral angle. The angle (asterisk) was measured between a line through the humerus (H) and the ulna (U) b Measurement of the drop sign. Distance from the trochlear joint surface to the joint surface of the olecranon in millimeters using sagittal images through the center of the coronoid (red line)
Magnetic resonance images following simple elbow dislocation demonstrating measurement of ulnohumeral and radiocapitellar incongruity. a Measurement of ulnohumeral incongruity. Distance from the trochlear joint surface to the joint surface of the olecranon was measured at the ulnar edge (A1), radial edge (A4), and two points in between (A2+A3). The difference between the largest and smallest distance was calculated and a distance greater than 1 mm was considered ulnohumeral incongruity. b Measurement of radiocapitellar incongruity. Radiocapitellar incongruity (B1) was measured from the rotational center of the capitellum (red circle) perpendicular to a line through the longitudinal axis of the radius (R)
Structures that were evaluated for injury included the coronoid process (avulsion fractures type I according to Regan and Morrey; yes vs. no; [26]), LCL (injured vs. intact), CEO (injured vs. intact), MCL (injured vs. intact), and CFO (injured vs. intact). To assess coronoid tip injuries, sagittal images were utilized; to assess LCL, CEO, MCL, and CFO injuries, mainly coronal images were used; however, sagittal and axial images were also assessed if sagittal images were ambiguous. Injury to the ligaments/muscle origins was defined as a complete or partial detachment from its respective origin. All MRIs were assessed by two orthopedic surgeons (PCN and MS). One investigator assessed the patients’ MRIs again 3 weeks following the first round to prevent recall bias.
Statistical analysis
Continuous data are presented as mean (range) and categorical values are presented as percentages. Fisher’s exact test was used to compare categorical variables. Simple logistic regression was first performed to assess potential risk factors for elbow instability. For this purpose, “elbow instability” was defined as axial ulnohumeral incongruity of more than 1 mm, as this has been shown to be highly suggestive of elbow instability [14]. Subsequently, a forward selection approach was chosen such that potential risk factors that were identified as statistically significant (p < 0.05) in univariate analysis were entered into a multiple logistic regression model. The odds ratios (OR) are presented with 95% confidence intervals (95% CI). Intraobserver agreement and interobserver agreement are presented as percentage of exact agreement using a sample of 30 randomly selected patients. The same sample was used to calculate intraobserver and interobserver agreement with Cohen’s kappa (k) and results were interpreted according to the recommendations of Landis and Koch [17]. Two-tailed p values were calculated and considered significant if p < 0.05. All statistical analyses were performed using Prism software (GraphPad, version 8.2.1, San Diego, CA, USA).
Results
Demographics
A total of 183 elbow MRIs of 183 patients that were performed between April 2006 and November 2020 were available and met the inclusion criteria. Of these, 36 patients were excluded due to an age of under 16 years (n = 12), an interval from injury to MRI of more than 21 days (n = 6), insufficient or incomplete imaging (n = 17), and a completely dislocated joint at time of MRI (n = 1). This left 147 patients (80.3%; 68 women, 79 men) with a mean age of 42.9 years (range, 17–85) at the time of MRI for final inclusion in the study (Fig. 3). The left elbow was injured in 90 patients (61.2%). Mean time from injury to MRI was 6.1 days (range, 0–21) and mean ulnohumeral angle was 46.4° (range, 7.6–100.1).
Radiographic variables
The LCL was injured in 142 patients (96.6%), the MCL in 132 patients (89.8%), the CEO in 58 patients (39.5%), the CFO in 59 patients (40.1%), and 23 patients (15.6%) had a tip fracture of the coronoid (Fig. 4). A total of 62 patients (42.2%) demonstrated radiocapitellar incongruity (> 2 mm), 36 patients (25.5%) demonstrated ulnohumeral incongruity (> 1 mm), and 17 patients (11.6%) had a drop sign (≥ 4 mm). All of the 36 patients (100%) with ulnohumeral incongruity on MRI had injuries to the CEO and/or CFO, whereas of the 111 patients without ulnohumeral incongruity, only 54 patients (48.6%) had injuries to the CEO and/or CFO (P < 0.001).
Magnetic resonance images demonstrating assessment of common extensor and flexor origin injury. a Coronal image demonstrating injury to the common extensors (blue asterisk) and common flexors (red asterisk). If coronal images were ambiguous, sagittal images of the lateral (b) and medial (c) side of the elbow were used to identify common extensor (blue asterisk) and flexor injury (red asterisk)
Simple and multiple logistic regression
The results of simple logistic regression are shown in Table 1. An ulnohumeral angle of ≤ 45° (p < 0.001), injury to the CEO (p < 0.001), CFO (p < 0.001), and a coronoid tip fracture type I according to Regan Morrey (p = 0.007) were significantly associated with elbow instability on MRI. The results of multiple logistic regression are shown in Table 2. All variables that were selected from simple logistic regression remained significantly associated with elbow instability per the study definition (p < 0.05).
Interobserver and intraobserver agreement
Kappa values and exact agreement in percentages for interobserver and intraobserver agreement are presented in Table 3. Interobserver and intraobserver agreement ranged from moderate (k = 0.41–0.60) to almost perfect agreement (k = 0.81–1.00) according to the scale proposed by Landis and Koch [17].
Discussion
There is consensus that the treatment strategy following simple elbow dislocations should be based on elbow stability after initial reduction of the joint [24, 30,31,32]. In stable elbow joints with no signs of re-dislocation within the functional arc and < 10° of joint angulation on fluoroscopy, nonoperative management can be undertaken [8, 28, 31], whereas in unstable elbow joints with tendencies for re-dislocation and > 10° of joint angulation on fluoroscopy, patients seem to benefit from operative management [10, 30, 31]. Often, however, the results of initial examination and fluoroscopy are not available to the treating physician. Instead, patients present to an elbow specialist with a recent MRI. Although MRI can provide accurate information on the injured structures, signs of elbow instability on MRI were long undefined until Hackl et al. [13, 14] demonstrated that ulnohumeral incongruity greater than 1 mm on MRI is highly suggestive of SED. Using this threshold, we aimed at identifying the pertinent structures that need to be injured in order to lead to signs of elbow instability on MRI.
The most important finding of this study was that all patients who demonstrated ulnohumeral incongruity greater than 1 mm on MRI following SEDs had injury to the CEO and/or CFO. Further, multivariate logistic regression demonstrated that injury to the CEO (OR: 10.45, p < 0.001), CFO (OR: 8.38, p < 0.001), and coronoid process avulsion (OR: 5.32, p = 0.02) as well as an ulnohumeral angle of ≤ 45° (OR: 4.95, p = 0.005) were significantly associated with ulnohumeral incongruity and were thus suggestive of elbow instability. It is important to note that injury to the LCL or MCL, both isolated or combined, did not result in signs of elbow instability. Our findings are in line with previous research emphasizing the importance of the origin of the muscles about the elbow to maintain stability [5, 11, 23, 29, 36]. The CFO has been shown to provide restraint against valgus forces, which is especially effective if the musculotendinous origin is tensed in forearm supination [23, 36]. Similarly, the CEO counteracts varus forces on the lateral side with its maximal effect when tensed in forearm pronation [11, 36]. Rehabilitation programs following SEDs have incorporated these forearm positions in order to provide additional stability [2, 25]. However, if the muscle origins are injured, their respective active or passive effect on elbow stability cannot be made use of. We postulate that this may be among the reasons for failure of nonoperative treatment. Interestingly, Adolfsson et al. [3] evaluated eight patients who sustained SEDs and were initially treated nonoperatively following closed reduction and had re-dislocated their elbow within the first week as shown on radiographs. These patients were then operated on and the authors noted that all had extensive soft-tissue injuries including both collateral ligaments and muscle origins of at least the one side [3]. Although in the current study cohort we excluded patients with a re-dislocation on MRI, all 36 patients with ulnohumeral incongruity on MRI had extensive soft-tissue injuries (e.g., injury to the CEO and/or CFO) as well, therefore corroborating the work of Adolfsson et al. [3]. In a recent review article, Robinson et al. [28] highlighted that in their opinion injury to the musculotendinous secondary stabilizers is what separates stable from unstable elbows following dislocation. Based on our own clinical experience, we completely agree with this assessment and therefore believe that the results of the current study lay an important scientific foundation for further research regarding this topic.
As mentioned earlier, elbow position is important for stability, and a flexed elbow is considered to be more stable due to compressive forces of the biceps, brachialis, and triceps muscles. For this reason, initial immobilization in the early posttraumatic phase is usually performed in a flexed position (90°). Therefore, it is somewhat logical that in this study an ulnohumeral angle of < 45° was associated with ulnohumeral incongruity (OR: 4.95, p = 0.005) as it can unmask even subtle instability that may have not been detected in higher degrees of flexion. However, injury to the CEO and/or CFO was a prerequisite for ulnohumeral incongruity in the group with an ulnohumeral angle of ≥ 45° as well with all eight patients demonstrating ulnohumeral incongruity having injured at least one of their muscle origins. Therefore, the authors of this study suggest that similarly to what has been shown for elbow instability on dynamic fluoroscopy, surgical stabilization should also be considered if there are signs of instability on MRI since nonoperative treatment of these patients may result in inferior outcomes [30]. This may be the case particularly for patients showing signs of instability on MRI with an ulnohumeral angle of ≥ 45° despite the fact that a more flexed elbow position is considered more stable. In the authors’ opinion, these elbows are highly unstable.
There are numerous MRI studies that have investigated soft-tissue injuries following SEDs [6, 9, 12, 18, 33,34,35, 37], most of which aimed at elucidating injury mechanism [18, 33, 35] or correlating MRI findings with intraoperative findings [12, 37]. However, limited evidence exists on pertinent structures that need to be injured in order to cause elbow instability on MRI. Cho et al. [6] investigated the MRIs of 30 patients who had sustained an SED and divided them into two groups based on stability following closed reduction. The authors found that the CEO was injured significantly more often in the unstable group, which is in line with our findings. In contrast to the study by Cho et al. [3], the current study’s criteria for instability were not based on radiographs and/or clinical examination, but solely on ulnohumeral incongruity on MRI.
Limitations
This study has limitations. First, we dichotomized injuries of the investigated structures (yes/no) and did not further subclassify them (partial tear/complete tear). Elbow position (e.g., ulnohumeral angle) on MRI was not standardized in this study. Therefore, there is bias regarding instability and elbow position on MRI. Patients that were allowed a higher degree of extension during MRI may have been more stable on examination, whereas patients with a higher degree of flexion on MRI may have had distinct signs of instability on examination precluding them from elbow extension during MRI because of the risk for re-dislocation. Additionally, it is known that ligamentous structures of the elbow are best visualized in extension on MRI [38]. Although inter- and intraobserver agreement was at least moderate, there were still some discrepancies in the diagnosis of injuries. Additionally, both raters were authors of the study. Further, this study was based on the findings of a single investigation demonstrating that ulnohumeral incongruity of greater than 1 mm is highly suggestive of elbow instability [14] and no clinical examination for elbow instability was performed. We acknowledge that further research is warranted on whether signs of elbow instability on MRI (e.g., ulnohumeral incongruity of > 1 mm) truly translates into elbow instability in the clinical setting. However, this study with one of the largest cohorts to date suggests that if there is ulnohumeral incongruity on MRI, the odds for CEO injury is increased by 10 (OR: 10.45) and the odds for CFO injury is increased by 8 (OR: 8.38).
Practical conclusion
-
Injury to the common extensor origin (CEO), common flexor origin (CFO), the coronoid tip, and an ulnohumeral angle of ≤ 45° are associated with signs of elbow instability on magnetic resonance imaging (MRI) following simple elbow dislocations.
-
If the CEO or CFO is injured, the odds for instability on MRI are increased by a factor of 10 and 8, respectively.
References
Acosta Batlle J, Cerezal L, López Parra MD et al (2019) The elbow: review of anatomy and common collateral ligament complex pathology using MRI. Insights Imaging 10:43
Adams JE (2020) Elbow instability: evaluation and treatment. Hand Clin 36:485–494
Adolfsson LE, Nestorson JO, Scheer JH (2017) Extensive soft tissue lesions in redislocated after simple elbow dislocations. J Shoulder Elbow Surg 26:1294–1297
Anakwe RE, Middleton SD, Jenkins PJ et al (2011) Patient-reported outcomes after simple dislocation of the elbow. J Bone Joint Surg Am 93:1220–1226
Buchanan TS, Delp SL, Solbeck JA (1998) Muscular resistance to varus and valgus loads at the elbow. J Biomech Eng 120:634–639
Cho CH, Kim BS, Yi J et al (2020) Common extensor complex is a predictor to determine the stability in simple posterolateral elbow dislocation: analysis of MR images of stable vs. Unstable dislocation. J Clin Med 9: https://doi.org/10.3390/jcm9103094
Coonrad RW, Roush TF, Major NM et al (2005) The drop sign, a radiographic warning sign of elbow instability. J Shoulder Elbow Surg 14:312–317
De Haan J, Schep NW, Tuinebreijer WE et al (2010) Simple elbow dislocations: a systematic review of the literature. Arch Orthop Trauma Surg 130:241–249
Demino C, Fowler JR (2020) Magnetic resonance imaging findings after elbow dislocation: a descriptive study. Hand. https://doi.org/10.1177/1558944720949961
Duckworth AD, Ring D, Kulijdian A et al (2008) Unstable elbow dislocations. J Shoulder Elbow Surg 17:281–286
Dunning CE, Zarzour ZD, Patterson SD et al (2001) Muscle forces and pronation stabilize the lateral ligament deficient elbow. Clin Orthop Relat Res 388:118–124
Dutto E, Artiaco S, Gallo A et al (2020) MRI in acute simple elbow dislocations: correlation of preoperative imaging and intraoperative findings of collateral ligaments and associated soft tissue injuries. Musculoskelet Surg. https://doi.org/10.1007/s12306-020-00678-4
Hackl M, Leschinger T, Müller LP et al (2016) Chronic ligamentous instability of the elbow. Orthopade 45:809–821
Hackl M, Wegmann K, Ries C et al (2015) Reliability of magnetic resonance imaging signs of posterolateral rotatory instability of the elbow. J Hand Surg Am 40:1428–1433
Hildebrand KA, Patterson SD, King GJ (1999) Acute elbow dislocations: simple and complex. Orthop Clin North Am 30:63–79
Josefsson PO, Johnell O, Gentz CF (1984) Long-term sequelae of simple dislocation of the elbow. J Bone Joint Surg Am 66:927–930
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Luokkala T, Temperley D, Basu S et al (2019) Analysis of magnetic resonance imaging-confirmed soft tissue injury pattern in simple elbow dislocations. J Shoulder Elbow Surg 28:341–348
Micic I, Kim SY, Park IH et al (2009) Surgical management of unstable elbow dislocation without intra-articular fracture. Int Orthop 33:1141–1147
Modi CS, Wasserstein D, Mayne IP et al (2015) The frequency and risk factors for subsequent surgery after a simple elbow dislocation. Injury 46:1156–1160
O’driscoll SW (1994) Elbow instability. Hand Clin 10:405–415
O’Driscoll SW, Morrey BF, Korinek S et al (1992) Elbow subluxation and dislocation. A spectrum of instability. Clin Orthop Relat Res 280:186–197
Park MC, Ahmad CS (2004) Dynamic contributions of the flexor-pronator mass to elbow valgus stability. J Bone Joint Surg Am 86:2268–2274
Pataky TC, Robinson MA, Vanrenterghem J (2013) Vector field statistical analysis of kinematic and force trajectories. J Biomech 46:2394–2401
Pipicelli JG, King GJW (2020) Rehabilitation of Elbow Instability. Hand Clin 36:511–522
Regan W, Morrey B (1989) Fractures of the coronoid process of the ulna. J Bone Joint Surg Am 71:1348–1354
Ring D, Jupiter JB (2002) Fracture-dislocation of the elbow. Hand Clin 18:55–63
Robinson PM, Griffiths E, Watts AC (2017) Simple elbow dislocation. Shoulder Elbow 9:195–204
Safran MR, Baillargeon D (2005) Soft-tissue stabilizers of the elbow. J Shoulder Elbow Surg 14:179s–185s
Schnetzke M, Aytac S, Keil H et al (2017) Unstable simple elbow dislocations: medium-term results after non-surgical and surgical treatment. Knee Surg Sports Traumatol Arthrosc 25:2271–2279
Schnetzke M, Aytac S, Studier-Fischer S et al (2015) Initial joint stability affects the outcome after conservative treatment of simple elbow dislocations: a retrospective study. J Orthop Surg Res 10:128
Schnetzke M, Bergmann M, Wegmann K et al (2018) Determination of elbow laxity in a sequential soft-tissue injury model: a cadaveric study. J Bone Joint Surg Am 100:564–571
Schnetzke M, Ellwein A, Maier D et al (2020) Injury patterns following simple elbow dislocation: radiological analysis implies existence of a pure valgus dislocation mechanism. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-020-03541-0
Schnetzke M, Schüler S, Hoffend J et al (2017) Interobserver and intraobserver agreement of ligamentous injuries on conventional MRI after simple elbow dislocation. BMC Musculoskelet Disord 18:85
Schreiber JJ, Potter HG, Warren RF et al (2014) Magnetic resonance imaging findings in acute elbow dislocation: insight into mechanism. J Hand Surg Am 39:199–205
Seiber K, Gupta R, Mcgarry MH et al (2009) The role of the elbow musculature, forearm rotation, and elbow flexion in elbow stability: an in vitro study. J Shoulder Elbow Surg 18:260–268
Tarallo L, Merolla G, Porcellini G et al (2020) Acute elbow dislocation: comparison between magnetic resonance imaging and intra-operative finding of ligament injury. Int Orthop 45:265–273. https://doi.org/10.1007/s00264-020-04875-5
Terada N, Yamada H, Toyama Y (2004) The appearance of the lateral ulnar collateral ligament on magnetic resonance imaging. J Shoulder Elbow Surg 13:214–216
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
P.-C. Nolte, D. Maier, F.C. Wagner, A. Ellwein, R.-O. DeyHazra, T. Guehring, K. Müller, P.-A. Grützner, and M. Schnetzke declare that they have no competing interests.
All procedures performed in studies involving human participants or on human tissue were in accordance with the ethical standards of the institutional and/or national research committee (Ethics Committee Rhineland-Palatinate, No. 837.084.14[9323-F]) and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Availability of data and material: data from this work are available upon reasonable request.

Scan QR code & read article online
Rights and permissions
About this article
Cite this article
Nolte, PC., Maier, D., Wagner, F.C. et al. Structural injuries correlate with radiographic signs of instability on MRI after simple elbow dislocations. Obere Extremität 16, 203–209 (2021). https://doi.org/10.1007/s11678-021-00651-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11678-021-00651-y
Keywords
- Joint instability
- Joint dislocations
- Medial collateral ligament
- Lateral collateral ligament
- Magnetic resonance imaging