Abstract
Purpose
The aim of this current study was to assess elbow ligament tears after dislocation using magnetic resonance imaging (MRI) and to correlate any pre-operative imaging with intra-operative findings of elbow ligament tears.
Methods
We prospectively included 32 patients with acute elbow dislocation investigated by MRI at a means of five days from dislocation. A simple elbow dislocation was diagnosed in 14 patients (44%); associated bone injuries were identified in 18 elbows (56%). Surgical repair of elbow ligaments was carried out in 23 patients, and nine cases were treated non-operatively. A blinded MRI evaluation of all 32 elbows was performed by an orthopaedic surgeon (rater 1) and a musculoskeletal radiologist (rater 2).
Results
Inter-rater agreement for MRI evaluation of 32 was poor for lateral ulnar collateral ligament (LUCL) tears, fair for radial collateral ligament (RCL), moderate for annular ligament (AL), and fair for ulnar collateral ligament (UCL). All tears were reported as complete by rater 1; 13/32 partial tears were identified by rater 2 (LUCL = 2, RCL = 2, UCL = 9). Correlation between surgical and MRI findings showed good inter-rater agreement for LUCL and AL tears in both raters. Agreement for RCL tear was poor for rater 1 and fair for rater 2; agreement for UCL tear was fair for rater 1 and poor for rater 2. Intra-operative findings showed ten radial head fractures (RHFs) and ten coronoid fractures (CFs). LUCL tears were found in the four cases of type II RHFs and in 3/4 cases of CFs. Bone injuries and ligament tears were not significantly associated.
Conclusion
MRI scan supported surgeons to identify soft tissue injuries and to address the most suitable surgical approach after acute elbow dislocation. Inter-observer agreement for intra-operative findings was high for LCL complex injuries and poor for UCL.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The elbow joint is the second most common site of dislocation in adults after the shoulder joint, with an annual incidence of 5.2 per 100,000 people per year [1].
Simple elbow dislocations are associated with soft tissue injury only, or minimal bone lesions and, are commonly managed conservatively when the joint stability is preserved after closed reduction. In the case of re-dislocation or persistent instability after reduction, a surgical intervention is recommended [2]. The anatomy and biomechanics of elbow ligaments and their role in joint stability have been well described [3,4,5].
The ulnar collateral ligament (UCL) complex consists of three bundles (anterior, posterior, and transverse), of which the anterior bundle acts as the main valgus stabilizer and the posterior one contributes as co-stabilizer to the valgus forces. The lateral collateral ligament (LCL) complex includes the lateral ulnar collateral ligament (LUCL), radial collateral ligament (RCL), annular ligament (AL), and when present, the accessory lateral collateral ligament (ALCL). The LUCL mainly contributes to the posterolateral rotatory stability, whereas the RCL preserves the varus stability and resists to posterolateral rotatory instability [6]; the AL acts as the primary stabilizer of the proximal radioulnar joint. Injuries of elbow ligaments after acute dislocation have been mainly attributed to the mechanism of instability suggested by O’Driscoll et al. [6]. PLRI induces injuries of collateral ligaments and overlying muscle that progress from the lateral to the medial side, involving the LUCL in all dislocations, while the involvement of UCL and overlying flexor-pronator (F-PT) muscles depend on the degree of progression of dislocation.
However, recent research findings have demonstrated an alternative mechanism of ligament injury, where a varus force can cause injury to the lateral structures of the elbow; then, the dislocation progresses postero-medially to the distal humerus causing the stripping of the UCL and F-PT muscles during the forearm external rotation (simple posteromedial instability [PM]), in addition to a continuously acting varus force. Rarely, a coronoid fracture can occur if the coronal tip is not disengaged from the trochlear notch during varus and forearm internal rotation force applying (posteromedial rotatory instability [PMRI]) [7].
Magnetic resonance imaging (MRI) is a valuable diagnostic tool to identify soft tissue injuries of the elbow, especially lateral and medial collateral ligaments tears [8,9,10]; however, it is not routinely carried out after acute elbow dislocation.
Recent research articles have analyzed the elbow ligament tears after dislocation using MRI [7, 9, 11,12,13], but none of them has evaluated the reliability of the MRI scan to detect lateral and medial elbow ligaments injuries.
The aim of this current study was to assess elbow ligament tears after dislocation using MRI and to correlate pre-operative imaging with intraoperative findings of elbow ligament tears in the elbows surgically treated.
Patients and methods
Study population and design
This was a prospective study including 32 consecutive patients with acute elbow dislocation who came to the Emergency Department from November 2013 to November 2019. The study was approved by the institutional review board (Prot. AOU0025970/19). All patients included in the study, reported a fall onto an outstretched hand during the injury. The direction of instability (PLRI or PM) was diagnosed on standard plain radiographs (anteroposterior and lateral views) performed in Emergency in line with the criteria reported by O’Driscoll et al. [1] and Rhyou et al. [14]. We identified 29 cases of PLRI and three cases of PM. An attempt of sedation-assisted closed reduction or under local and general anaesthesia was carried out on all patients; those with persistent subluxation or re-dislocation and asymmetric widening of radiocapitellar or humeroulnar joints within the range of full flexion to 40–50° of passive range of motion, were recommended for surgical treatment. All 32 elbows were also investigated with MRI at a means of five days from dislocation (range: 2–7 days). A simple elbow dislocation was diagnosed in 14 patients (44%); associated radial head and coronoid fractures (RHF and CF) were identified in 18 elbows (56%) on X-ray and classified by MRI according to Broberg-Morrey [15] and Regan-Morrey [16] classification systems. Surgical repair of elbow ligaments was performed in 23 patients, while nine cases were treated nonoperatively (the elbow was immobilized for three weeks followed by in-house hospital standard physical therapy treatment plan for another three weeks to restore active range of motion).
Demographic data of the study population is reported in Table 1. A blinded MRI evaluation of all 32 elbows was performed by a fellowship trained elbow surgeon (rater 1) and an expert upper limb musculoskeletal radiologist (rater 2). In order to provide a blindness evaluation, a resident not involved in the surgical procedure took charge of every patient, referring them to the radiologist and the orthopaedic surgeon involved in MRI assessment of the elbow. Surgery was then performed by another expert elbow surgeon, and finally intra-operative findings were used as gold standard to correlate with pre-operative MRI imaging.
Magnetic resonance imaging assessment
The elbow MRI scan was carried out on all patients using Achieva 1.5T equipment (Philips Health Care; Eindhoven, The Netherlands). Each patient was placed in the supine position, with the arm at the patient’s side, the elbow fully extended in an appropriate coil, and the forearm supinated [17].
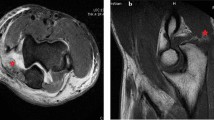
Axial, sagittal, and coronal images of 2.5-mm slice thickness and a 0.5-mm section spacing were acquired using T1-weighted and T2-weighted and proton density (PD) sequences, with and without fat suppression [18]. The protocol and parameters used in the MRI sequences are described in Table 2. The collateral ligaments of the elbow were visualized in a 20° posterior oblique coronal plane in relation to the humeral diaphysis with the elbow extended and a coronal plane aligned with the humeral diaphysis with the elbow flexed 20 to 30° (Fig. 1a–b).
Coronal images were correlated with the axial and sagittal images to confirm the suspected pathology.
UCL and LUCL alterations in signal and morphology on T1-weighted and T2-weighted imaging were suspected of ligament tear [19] (Figs. 2 and 3a–b). The UCL’s anterior bundle was evaluated in a coronal view, while the posterior bundle was well recognized and evaluated in axial view. The annular ligament of lateral collateral ligament (LCL) complexes was evaluated in axial and sagittal views; coronal and sagittal views were used for evaluation of the RCL and LUCL [20]. Protocol and parameters used in the MRI sequences of the elbow are reported in Table 2. Images were processed and elaborated using OsiriX DICOM Viewer 11.0 (Bernex, Switzerland).
a T2-weighted coronal and b sagittal PDW-SPAIR MRI showing a complete avulsion of LUCL from the humeral side (white asterisk). c, d Intraoperative view of LUCL avulsed from the humeral insertion (white asterisk). PDW, proton density weighted; SPAIR, spectral attenuated inversion recovery; MRI, magnetic resonance imaging; LUCL, lateral ulnar collateral ligament
a Coronal and b sagittal PDW-SPAIR MRI showing a partial tear of UCL (white asterisk) and complete tear of LUCL (white circle). c, d Intra-operative view showing partial tear of UCL (black asterisk), complete tear of LUCL (white circle), and integrity of RCL. PDW, proton density weighted; SPAIR, spectral attenuated inversion recovery; MRI, magnetic resonance imaging; UCL, ulnar collateral ligament; LUCL, lateral ulnar collateral ligament; RCL, radial collateral ligament
Surgical procedure
Twenty-three patients underwent surgical treatment using an ultrasound-guided axillary brachial plexus block (carbocaine 3% or naropine 7.5 ml). This procedure allows enough relax of the upper extremity to perform elbow examination before any surgical procedure. Patients were placed in the supine position with a sterile tourniquet at the arm root. Prior to any procedure and in elbows without bone injuries, the direction of instability was examined under anaesthesia to assess PLRI with lateral pivot-shift test and the PM with the varus and internal rotation test. Overall, PLRI was diagnosed in 21 elbows and PM in 4.
A single lateral approach was used in 19 elbows, a single medial approach was performed in one elbow, and a combined approach (medial and lateral) in three elbows.
The lateral side of the elbow joint was exposed through a modified Kocher approach performed by developing an intramuscular interval between the anconeus muscle and the extensor carpi ulnaris. The radial collateral ligament and the accessory LCL were incised preserving the LUCL when found intact. The integrity of the LUCL was assessed by using the tip of the pliers to pass from the anterior to posterior aspect of the capitulum humeri [21] (Fig. 2c). A stripping-type tear pattern of common extensor muscles and LCL complex with retraction from the lateral epicondyle was found in five elbows. Four unstable RHFs were fixed with two or more cannulated compression screws (diameter: 3.5-mm tip, 3.6-mm tail; Acutrak 2 [Acumed Ltd, Andover, UK]). Twenty-one deficient LUCLs were identified as complete tears and fixed on the lateral surface of the humeral condyle using a suture anchor or a double transosseous bone-tunnel (Fig. 2d). Two Fiberwire nonabsorbable sutures (Arthrex, Naples, FL, USA) were placed with a locked Krackow stitch in the RCL, LUCL, and posterior capsule. The sutures were passed through the divergent bone tunnels, anteriorly and posteriorly to the lateral column, and tied over a bone bridge in the lateral supracondylar ridge. In four elbows with UCL insufficiency after LUCL repair, an additional medial approach was performed [12]. The anterior bundle of UCL was exposed preserving the origin of flexor carpi ulnaris (FCU) tendon on the medial epicondyle (Fig. 3c); associated F-PT muscle injury was pre-operatively identified on MRI and intra-operatively found in 3 elbows (Fig. 4a–c). The proximal insertion of UCL ligament (i.e., anterior bundle) was re-attached to the humerus with bone suture (Fig. 4d–e) (No. 2 Fiberwire [Arthrex, Naples, FL, USA]). At the end of the procedure, the elbow was immobilized with an arm sling for three weeks. Three CFs were fixed with a precontoured plate using a combined approach in two elbows and a single medial approach in 1 (Fig. 4d).
a, b Coronal T2-weighted and sagittal T2-weighted SPIR MRI view, showing a complete avulsion of flexor-pronator muscle (white asterisk) and LUCL (white circle) from the humeral origin, with posterior dislocation of the radial head. c Intra-operative view showing complete avulsion of flexor-pronator muscle from the medial epicondyle. d, e Coronoid fracture fixation with plate (white apex) and site of insertion of UCL on the medial facet of the humerus (white hashtag). f Complete avulsion of LUCL from the humerus (black circle). SPIR, spectral presaturation with inversion recovery; MRI, magnetic resonance imaging; LUCL, lateral ulnar collateral ligament; UCL, ulnar collateral ligament
The lateral pivot shift test and the varus stress test were carried out once again at the end of each procedure to assess the joint stability.
Active-assisted range of motion exercises were allowed after one month and strengthening exercises after two months.
Statistical analysis
Descriptive statistics analyses (absolute and percentage frequency, mean, median, standard deviation, and range) were calculated for all variables. Cohen’s kappa was used to determine inter-rater agreement among the two MRI raters and the correlation between MRI and intra-operative findings of elbow ligaments and overlying muscle injuries. Strength of agreement was evaluated according to the criteria of Landis and Cock [22]. The possible association between MRI and intra-operative findings of elbow ligament injuries and qualitative variables (age, sex, dominance, side, body mass index, injury-to-surgery interval) was evaluated with the analysis of 휒2 test. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy of MRI in evaluating elbow ligament injuries were calculated with surgical exploration findings as the gold standard. The level of significance was set at 0.05. All analyses were carried out using Stata Intercooled 14.2 software for Windows (StataCorp LP, College Station, TX, USA).
Results
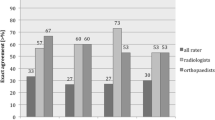
Inter-rater agreement for MRI evaluation of 32 elbows after dislocation was poor for LUCL tears, fair for RCL, moderate for AL, and fair for UCL (Table 3). Distribution of ligament tears among the two raters is described in Fig. 5. All tears were reported as complete by rater 1; 13/32 partial tears were identified by rater 2 (LUCL = 2, RCL = 2, UCL = 9).
Age, sex, side, dominance, and body mass index were not associated with intraoperative findings of elbow ligament tears. The sensitivity, specificity, PPV, NPV, and accuracy of MRI scan for surgical findings of ligament tears in 23 elbows are reported in Table 4.
MRI showed excellent accuracy for LUCL tears, with high sensitivity (100%), but low specificity (50%) in both raters; in the two cases of AL tears, we had found high accuracy (95.7%), sensitivity (100%), and specificity (95%).
Accuracy for RCL tears was higher for the rater 2, whereas low specificity was recorded by both raters; accuracy UCL tear resulted moderate for rater1 and low for the rater 2 (Table 4). Correlation between surgical and MRI findings of elbow ligament tears of the two raters is reported in Table 5; inter-rater agreement was good for LUCL and AL tears in both raters. Agreement for RCL tear (Fig. 3d) was poor for rater 1 and fair for rater 2; agreement for UCL tear was fair for rater 1 and poor for rater 2. Intra-operative findings of the 23 elbows included ten RHFs (type I in 6 and type IV in 4) and ten CFs (type I in 6 and type II in 4). LUCL tears were found in the four cases of type II RHFs and in 3/4 cases of CFs. Bone injuries and ligament tears were not significantly associated.
Discussion
The results of this study demonstrated a good reliability of MRI scan to predict LCL injuries. Accuracy and sensitivity resulted high for LUCL and AL tears and good for RCL tears. The variable value of specificity recorded for all LCL components should be interpreted with concern due to the small size of the sample. The more controversial and less reliable issue was the MRI detection of UCL tears by both raters, although the orthopedic surgeon appeared to be more accurate compared with the musculoskeletal radiologist. Regarding the reliability of UCL findings, similar considerations apply since related to the need of a larger population and a larger sample of elbows with medial side injuries. Inter-rater agreement of MRI evaluation in the 32 elbows after dislocation was weak, with the exception of the moderate agreement found in the two elbows with AL tears.
Our results are in line with other research findings [18, 20, 23] and deserve some considerations. Schnetzke et al. demonstrated weak intra- and inter-observer agreement by conventional MRI technique in the evaluation of ligaments after simple elbow dislocation and emphasized the need for new MRI quality standards with special focus on coronal oblique reconstructions [23].
Other authors have pointed out that in non-arthrographic imaging, the LUCL is completely visible in approximately 80% of patients and only partially visible over its entire course in 18% of patients [18]. The utility of MRI has remained controversial also for imaging of the AL, because it underestimated the degree of AL interposition within the radio-capitellar joint; however, the presence of effusion in the acute setting of elbow dislocation might improve the identification and evaluation of AL tears [20].
Our study also showed the lack of consistency in the interpretation of some MRI variables (partial vs complete ligament tears, overlying muscle injuries) by two raters (musculoskeletal radiologist and orthopedic surgeon) of proven experience in their own field, but with different surgical backgrounds and clinical education.
In this respect, Luokkala et al. reported a substantial agreement between radiologists for MRI analysis of soft injury pattern in simple elbow dislocation [10]. Schnetzke et al. showed fair to moderate interobserver agreement of four examiners (experienced and non-experienced radiologists and orthopaedics) for collateral ligaments; radiologists showed highest agreement strength for the UCL [23].
Literature data and our study confirm that substantial MRI agreement for all subtypes of collateral ligament injuries after elbow dislocation is rarely achieved.
Analysis of radiograms brought out a main mechanism of PLRI producing ligament and overlying muscle injuries; PM instability was reported in a few cases, thus confirming the poor frequency of this mechanism [7, 11]. Although the lateral side was the most affected in both assumed mechanisms, our results are only partially consistent with other studies exploring ligament involvement after elbow dislocation. In a previous study, conceived with a view of an occult elbow dislocation, LUCL avulsion was intra-operatively found in 60% of unstable RHFs [21]. Heo et al. reviewed 21 cases after PLRI and reported repair of LCL in all cases and UCL in 4; LCL injuries were found in all cases and UCL in ten cases on 17/21 pre-operative MRI [24]. The main involvement of LCL complex following an elbow dislocation, confirmed by surgical exploration, was reported in other studies [25, 26]. Lee et al., using MRI, reported 100% of LCL complex tears, of which 87.5% were complete, and about 50% of complete UCL tears [9]. These findings confirmed that the medial-sided disruption was more variable.
Simple PM dislocation is uncommon to find, but has been associated with severe lateral complex injuries, resulting in a high rate of surgical treatment [11].
In contrast, other researchers demonstrated a more severe damage of soft tissue at the medial side of the joint compared to the lateral side after posterolateral dislocation [13]. Schreiber et al. suggested multiple mechanisms of elbow dislocation, in which the most common injury pattern may begin with a medial-sided ligamentous disruption [13].
Recently it has been reported that LCL injuries had no significant correlation with the associated fractures after elbow dislocation, whereas UCL injuries are significantly correlated with fractures of the coronoid and radial head [9].
Our study failed to show significant correlations between bone injuries and ligament tears, even though complete LUCL disruption was found in the four elbows with displaced unstable RHFs.
Overall, MRI scan represents a valid diagnostic tool to recognize soft tissue injuries of the elbow, still with the limits of the variable agreement between observers. The difficulty in carrying out the examination in the acute setting and the cost-benefit ratio for the National Health Service should be considered. In addition, the MRI scan does not replace computed tomography (CT) scan, which still remains the most appropriate diagnostic assessment to identify any bone lesions.
This is the first prospective study in literature comparing preoperative MRI evaluation with intra-operative findings of soft tissues injuries after acute elbow dislocation.
The major limitations of this study include the following: (a) MRI raters of the study were instructed to identify elbow injuries after instability; it is possible that this lack of blinding regarding the patient case history of dislocation may have affected their evaluations; (b) the small number of some types of ligament injuries prevents reliable statistical evaluation.
In conclusion, the MRI scan is valid to diagnose LCL elbow injuries after acute elbow dislocation, but it lacks substantial agreement for medial side injuries; however, the small number of UCL tears reported in this study prevents reliable statistical evaluation. The MRI scans supported surgeons to identify soft tissue injuries and to address the most suitable surgical approach. Interobserver agreement for intra-operative findings was high for LCL complex injuries and poor for UCL tears; orthopaedic surgeons were more likely to identify complete LUCL tears. Correlations with intra-operative findings represent the best method to improve the quality of MRI assessment and the agreement between the orthopaedic surgeon and the radiologist. Overall, the decision to undertake elbow ligaments repair should be primarily based on clinical examination performed under anaesthesia. MRI is useful to identify the exact site of lateral ligament tears in unstable elbow after reduction and in those cases where joint stability is unclear and standard radiographs show widening of joint space.
References
Stoneback JW, Owens BD, Sykes J et al (2012) Incidence of elbow dislocations in the United States population. J Bone Joint Surg Am 94:240–245. https://doi.org/10.2106/JBJS.J.01663
De Haan J, Schep NW, Tuinebreijer WE et al (2010) Simple elbow dislocations: a systematic review of the literature. Arch Orthop Trauma Surg 130:241–249. https://doi.org/10.1007/s00402-009-0866-0
Camp CL, Fu M, Jahandar H, et al. (2019) The lateral collateral ligament complex of the elbow: quantitative anatomic analysis of the lateral ulnar collateral, radial collateral, and annular ligaments. J Shoulder Elbow Surg; 28: 665–670 2018/12/12. https://doi.org/10.1016/j.jse.2018.09.019
Cinque ME, Schickendantz M, Frangiamore S (2020) Review of anatomy of the medial ulnar collateral ligament complex of the elbow. Curr Rev Musculoskelet Med. https://doi.org/10.1007/s12178-020-09609-z
Morrey BF, An KN (1985) Functional anatomy of the ligaments of the elbow. Clin Orthop Relat Res:84–90
O'Driscoll SW, Bell DF, Morrey BF (1991) Posterolateral rotatory instability of the elbow. J Bone Joint Surg Am 73:440–446
Rhyou IH, Lee JH, Lee JH et al (2020) Soft tissue injury patterns in posteromedial rotatory instability with dislocation compared with posteromedial dislocation of the elbow joint. J Shoulder Elb Surg. https://doi.org/10.1016/j.jse.2019.11.002
Dewan AK, Chhabra AB, Khanna AJ et al (2013) MRI of the elbow: techniques and spectrum of disease: AAOS exhibit selection. J Bone Joint Surg Am 95(e99):91–13. https://doi.org/10.2106/JBJS.L.01621
Lee SH, Nam DJ, Yu HK et al (2020) The lateral ligament is injured preferentially in posterolateral dislocation of the elbow joint. Bone Joint J 102-B:227–231. https://doi.org/10.1302/0301-620X.102B2.BJJ-2019-0966.R1
Luokkala T, Temperley D, Basu S et al (2019) Analysis of magnetic resonance imaging-confirmed soft tissue injury pattern in simple elbow dislocations. J Shoulder Elb Surg 28:341–348. https://doi.org/10.1016/j.jse.2018.08.010
Cho CH, Kim BS, Rhyou IH et al (2018) Posteromedial elbow dislocations without relevant osseous lesions: clinical characteristics, soft-tissue injury patterns, treatments, and outcomes. J Bone Joint Surg Am 100:2066–2072. https://doi.org/10.2106/JBJS.18.00051
Lee JH, Lee JH, Kim KC et al (2019) Treatment of posteromedial and posterolateral dislocation of the acute unstable elbow joint: a strategic approach. J Shoulder Elb Surg 28:2007–2016. https://doi.org/10.1016/j.jse.2019.05.029
Schreiber JJ, Potter HG, Warren RF et al (2014) Magnetic resonance imaging findings in acute elbow dislocation: insight into mechanism. J Hand Surg Am 39:199–205. https://doi.org/10.1016/j.jhsa.2013.11.031
Rhyou IH, Kim YS (2012) New mechanism of the posterior elbow dislocation. Knee Surg Sports Traumatol Arthrosc 20:2535–2541. https://doi.org/10.1007/s00167-011-1872-7
Broberg MA, Morrey BF (1987) Results of treatment of fracture-dislocations of the elbow. Clin Orthop Relat Res:109–119
Regan W, Morrey B (1989) Fractures of the coronoid process of the ulna. J Bone Joint Surg Am 71:1348–1354
Binaghi DMR (2015) Imaging of the elbow. Magn Reson Imaging Clin N Am 23:427–440. https://doi.org/10.1016/j.mric.2015.04.005
Bucknor MD, Stevens KJ, Steinbach LS (2016) Elbow imaging in sport: sports imaging series. Radiology 280:328. https://doi.org/10.1148/radiol.2016164015
Schaeffeler C, Waldt S, Woertler K (2013) Traumatic instability of the elbow - anatomy, pathomechanisms and presentation on imaging. Eur Radiol 23:2582–2593. https://doi.org/10.1007/s00330-013-2855-5
Mak S, Beltran LS, Bencardino J et al (2014) MRI of the annular ligament of the elbow: review of anatomic considerations and pathologic findings in patients with posterolateral elbow instability. AJR Am J Roentgenol 203:1272–1279. https://doi.org/10.2214/AJR.13.12263
Tarallo L, Porcellini G, Merolla G et al (2020) Isolated displaced type II partial articular radial head fracture: correlation of preoperative imaging with intraoperative findings of lateral ulnar collateral ligament tear. J Shoulder Elb Surg 29:132–138. https://doi.org/10.1016/j.jse.2019.07.006
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Schnetzke M, Schuler S, Hoffend J et al (2017) Interobserver and intraobserver agreement of ligamentous injuries on conventional MRI after simple elbow dislocation. BMC Musculoskelet Disord 18:85. https://doi.org/10.1186/s12891-017-1451-2
Heo YM, Yi JW, Lee JB et al (2015) Unstable simple elbow dislocation treated with the repair of lateral collateral ligament complex. Clin Orthop Surg 7:241–247. https://doi.org/10.4055/cios.2015.7.2.241
Kim JW, Yi Y, Kim TK et al (2016) Arthroscopic lateral collateral ligament repair. J Bone Joint Surg Am 98:1268–1276. https://doi.org/10.2106/JBJS.15.00811
Schnetzke M, Aytac S, Keil H et al (2017) Unstable simple elbow dislocations: medium-term results after non-surgical and surgical treatment. Knee Surg Sports Traumatol Arthrosc 25:2271–2279. https://doi.org/10.1007/s00167-016-4100-7
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
IRB approval was obtained from the institutional review board (Prot. AOU0025970/19, Comitato Etico Area Vasta Emilia Nord, Modena, Italy).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(PDF 222 kb)
Rights and permissions
About this article
Cite this article
Tarallo, L., Merolla, G., Porcellini, G. et al. Acute elbow dislocation: comparison between magnetic resonance imaging and intra-operative finding of ligament injury. International Orthopaedics (SICOT) 45, 265–273 (2021). https://doi.org/10.1007/s00264-020-04875-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04875-5