Abstract
Summary
“Health-based threshold value” is used to define the optimal cutoff of vitamin D. This approach is based on the hypothesis of a secondary hyperparathyroidism associated with hypovitaminosis D. We define the optimal values in a North Algerian population. The optimal value is 25.0 ng/ml in men and 30.0 ng/ml in women.
Purpose/Introduction
There is no consensus defining the vitamin D optimal values. The aim of this study is to establish vitamin D optimal values in the Northern Algerian population, based on its skeletal effects as represented by the inverse relationship between 25-hydroxy vitamin D (25(OH) D) and parathyroid hormone (PTH).
Methods
451 healthy volunteers of both genders, aged 19 to 79 years, were enrolled in a cross-sectional study conducted at the medical analysis laboratory of the University Hospital of Blida, Algeria. 25(OH) D was assessed by a sequential competitive immuno-fluoroassay technique. Determination of vitamin D optimal values was performed based on the kinetic relationship between 25(OH) D and PTH, as explored by inverse nonlinear regression on a spline plots curve. The optimal value represents the 25(OH) D level at which PTH ceases to increase and reaches a virtual plateau.
Results
In men and women, respectively, the 25 (OH) D thresholds are estimated at 25.0 ng/ml and 30 ng/ml, above this value, PTH stabilizes in a virtual plateau, estimated at 22.3 pg/ml and 26.8 pg/ml. In warm and cold seasons, respectively, the 25 (OH) D cut-offs are estimated at 30.0 ng/ml and 25.0 ng/ml, from these values, the PTH stabilizes in a virtual plateau, estimated at 21.5 pg/ml and 27.7 pg/ml.
Conclusion
In this study, the optimal values of 25(OH) D were defined for the first time in a North Algerian adult population. The optimal value is 25.0 ng/ml in men and 30.0 ng/ml in women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
At present, a universal consensus defining an adequate or optimal vitamin D status is still lacking. If the 25-hydroxy-vitamin D (25 (OH) D) level, defining severe vitamin D deficiency is well admitted by most scientific institutions, being set at the threshold of 10 to 12 ng/ml (25 to 30 nmol/l); threshold below which the risk of bone disorders such as rickets, osteomalacia, and osteoporosis is significantly more probable [1,2,3,4], the 25(OH) D level defining vitamin D insufficiency is still a subject of discussion.
To define vitamin D insufficiency, or hypovitaminosis D, in the broad sense of the concept, two definitions are currently the most widely used. The first one is a patient-care-based guidance, proposed by the Endocrine Society Clinical Practice Guidelines (ES-CPG) Committee [5] which recommends optimal levels of at least 30 ng/ml. The second one, set at a level of at least 20 ng/ml, is a population-based guidance proposed by the North American Institute of Medicine (IOM) in order to ensure adequacy of vitamin D intake. This last definition is adopted by most researchers and scientific organizations, including the Standing Committee of Europe Doctors and even the World Health Organization (WHO) [6,7,8]. The difference in cut-off values can be explained, in part, by the population targeted by the two organizations. Indeed, the recommendations provided by the ES-CPG were established in the context of a medical practitioner offering advice to patients at high risk of vitamin D deficiency, whereas those proposed by the IOM were established to provide fairly conservative advice for public vitamin D intake, with the main goal to minimize the bone repercussions due to secondary hyperparathyroidism related to vitamin D deficiency [9, 10].
However, considering the geographic, ethnic, cultural, and culinary diversities that impact serum vitamin D concentrations, it would be appropriate to define the optimal values in each population.
In order to define vitamin D insufficiency, the reference ranges approach commonly used for most biological parameters: recruiting a healthy population, and defining the range in which 95% of observed values are found, cannot be applied to 25(OH) D [2, 4]. Instead, all the experts agree that it is more appropriate to define levels of 25(OH)D below which deleterious consequences of vitamin D deficiency may occur; hence, the terms “optimal,” “suitable,” or “recommended” values are proposed rather than “normal” or “reference” values [4, 11]. Such optimal threshold setting is known as “health-based threshold values” [2].
Hence, there is an international consensus which consists in the use of vitamin D bone effects; the most frequently used assessment criterion is based on the hypothesis of a secondary hyperparathyroidism associated with hypovitaminosis D [2, 12, 13]. Indeed, vitamin D is a key factor for bone development and remodeling, promoting calcium and phosphorus intestinal absorption [14, 15]. In case of vitamin D deficiency, the subsequent decrease of calcium and phosphorus absorption can lead to an increase in parathyroid hormone (PTH) levels, causing a secondary hyperparathyroidism and, consequently, a bone depletion of calcium in order to restore normo-calcemia [14, 16, 17].
Although, theoretically, there is a significant correlation between vitamin D and all the phosphocalcic parameters, in particular: total calcemia, ionized calcemia, and phosphoremia, they are not considered as reliable indicators of vitamin D status. In fact, their levels are regularly maintained within their reference ranges, through secondary hyperparathyroidism compensating, hence, any vitamin D insufficiency. The choice of PTH as “The” parameter to be monitored for defining optimal vitamin D values seems therefore to be the most appropriate one [1, 13, 14, 18]. Thus, defining the optimal value of 25(OH) D comes to define the level at which PTH concentrations cease to increase and stabilize in a virtual plateau form [2, 4, 12, 13]. However, it is noteworthy that despite its accessibility, this approach, based on the relationship between vitamin D and secondary hyperparathyroidism, is not the gold standard for defining optimal 25(OH) D values. In this context, the IOM has established its threshold values on the basis of the direct relationship between vitamin D levels, intestinal calcium absorption, and bone density status [9, 10].
This study is designed with the aim to define the vitamin D optimal values in the North Algerian adult population, based on its skeletal effects as depicted by the kinetic relationship between 25(OH) D and PTH.
Methods
Study design and population
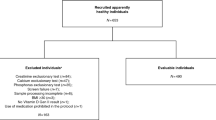
This is a cross-sectional study, with a prospective recruitment, carried out between January 2020 and September 2021, in the medical laboratory of the Frantz Fannon University Hospital of Blida, Algeria (36.5° N). The included population consisted of healthy volunteers of both sexes, aged over 18 years.
Non-inclusion criteria were carefully selected in order to avoid potential confounding factors that might influence phosphocalcic metabolism, particularly with regard to PTH. These criteria were vitamin D or calcium supplementation within 3 months prior to study enrollment, hepatocellular insufficiency, and chronic renal disease, defined by an estimated glomerular filtration rate (eGFR) < 60 ml/min/1. 73 m2, thyroid disease, tumor disease, bowel disease, pregnancy, PTH > 88 pg/ml with normocalcemia or hypercalcemia, and morbid obesity defined as body mass index (BMI) > 40 kg/m2.
A total of 451 subjects were included, and their consent was obtained. This study was conducted in accordance with the Declaration of Helsinki and approved by the local ethics committee.
Data collection and biochemical measurements:
For all enrolled subjects, demographics (age and gender) and season of blood sampling were recorded. The Fitzpatrick classification was used to define the phototype of subjects [19].
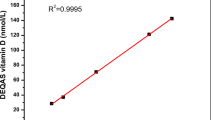
Vitamin D status was assessed by measuring the total 25(OH) D form (D2 + D3). The assay was performed by a sequential competitive immuno-fluorescent assay, on mini-VIDAS®. This method has a linearity limit of 150 ng/ml, and a variation coefficient ranging from 2.1 to 16%.
The PTH assay was performed by a sandwich enzyme-linked Immunoassay combined with final fluorescence detection (ELFA). This is a third-generation method for assaying PTH (1–84). The measurement domain is between 4.0 and 1500.0 pg/ml. Hyperparathyroidism was defined by a PTH level > 44.4 pg/ml, based on the reference values provided by the reagent kits.
Statistical analysis
Statistical analysis was performed using SPSS software, version 25.0. The Shapiro–Wilk test was used to test the distribution normality of the quantitative variables. Quantitative variables are presented as means ± standard deviations and compared by Student’s t-test or by ANOVA followed by post hoc multiple comparison. Categorical variables are presented as percentages and compared by Pearson’s χ2 test. For all parameters, a two-tailed p-value of less than 0.05 was considered as statically significant.
The definition of vitamin D optimal values was based on the kinetic relationship between 25(OH) D and PTH. The optimal value refers to the level of 25(OH) D at which PTH no longer increases and forms a virtual plateau.
In order to establish the optimal values for vitamin D, the following steps were conducted:
-
First, a spline plot was performed to estimate the shape of the relationship between serum PTH (y-axis) and 25(OH) levels (x-axis).
-
Secondly, an estimation of spline curves was carried out in order to seek significant non-linear relations between these two parameters; indeed, no thresholds could be identified by linear regressions.
-
Third, selection of the most convenient nonlinear regression model: among the nonlinear models that explain significantly the relationship between PTH and 25(OH) D, the one with the highest values of F-test and nonlinear regression coefficient (R2) is selected.
-
Fourth, the serum 25 (OH) D optimal threshold is estimated visually; it refers to the value at which PTH starts to decrease less sharply and stabilizes in a virtual plateau [20].
In the same way, the optimal values were identified in the total population and then separately according to gender and sampling season.
Results
Characteristics of the study population
The general characteristics of the study population are summarized in Table 1. Of the 451 enrolled subjects, 41% were men and 59% were women. Age ranged from 19 to 79 years, with a mean of 42.8 ± 12.1; women were significantly younger than men. The large majority of the included subjects had a matt skin (phototypes III and IV) (73.2%). A proportion had a fair skin (phototypes I and II) (22.2%), and only 4.7% had a dark skin (phototypes V and VI). The majority of blood samples were obtained during the cold season (winter and spring). eGFR values ranged from 62 to 168 ml/mn/1.73 m2, with a mean value of 85.7 ± 18.3; woman had slightly lower values of eGFR (p = 0.001)0.25(OH) D levels ranged from 5.0 to 71.9 ng/ml, with a mean of 12.7 ± 9.4 ng/ml. Women had significantly lower levels (p = 0.03). PTH levels ranged from 9.4 to 84.5 pg/ml, with a mean of 36.1 ± 0.82 pg/ml. Women had significantly higher levels (p = 0.001).
Deficiency and severe deficiency, defined respectively at the thresholds of 20 ng/ml and 10 ng/ml, were very prevalent in our population, affecting more than one-fifth of the included subjects (27.9% and 54.5%, respectively, for deficiency and severe deficiency). Only 4.9% had sufficient levels as defined by the target threshold of 30 ng/ml. Overall, women had a significantly poorer vitamin D status compared to men.
Analysis of the association shape between 25 (OH) D and PTH
In order to analyze the association shape between vitamin D status and PTH, the population was subdivided into six classes of 25(OH) levels of 5.0 ng/ml each. PTH was treated as a continuous and dichotomous variable. Accordingly, the kinetics of PTH means and hyperparathyroidism prevalence across 25(OH) D classes are shown in Fig. 1a–b, respectively.
A significant inverse relationship was observed between PTH and 25(OH) D (pANOVA < 0.0001). The highest value was found in subjects with the lowest 25(OH) D levels (< 10 ng/ml); this value decreased gradually until reaching a plateau in subjects with 25(OH) D levels > 25 ng/ml (Fig. 1a).
Similarly, the highest prevalence of hyperparathyroidism was found in subjects with a 25(OH) D level < 10 ng/ml. This prevalence decreased progressively; a plateau was also reached in subjects with a 25(OH) D level > 25 ng/ml) (pfor trend < 0.0001) (Fig. 1b).
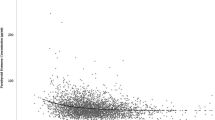
Spline plots and estimation of non-linear regression curves between PTH and 25(OH) D
The distribution of PTH values depending on 25 (OH) D values along with both linear and non-linear regression curves is presented in the spline plots depicted in Fig. 1-S. The features of the regression curves are presented in Table 2.
Considering the results of estimated curves, the inverse nonlinear regression model was selected. Indeed, it provides the highest values of both F-test and regression coefficient (F = 113.32, and R2 = 0.200, respectively). The regression coefficient interpretation (R2) implies that according to this model, 20% of the PTH variation is explained by the 25(OH) D levels.
Determination of 25(OH) D optimal value in the general population
The inverse nonlinear regression between PTH and 25(OH) D values, in the total population, is illustrated in Fig. 1.
According to this regression model, the relationship between PTH and 25(OH) D is expressed by the following equation:
In the case of this study population, this equation was formulated as follows:
The 25(OH) D cut-off point at which PTH starts to reach a plateau was visually estimated at a level of 26 ng/ml. From this value, PTH is stabilized in a virtual plateau, estimated at 26.0 pg/ml. This implies that the optimal value of 25(OH) D in our population is assumed to be around 26 ng/ml.
Determination of optimal 25(OH) D values according to gender
Similar analysis steps were performed to determine the optimal values in men and women separately. The results are shown in Fig. 2-a-S, and 2-b-S respectively.
In men: the established equation was as follows:
The 25(OH) D cut-off point at which PTH begins to reach its plateau was visually estimated at a level of 25.0 ng/ml; at this value, PTH is stabilized at a virtual plateau estimated at 22.3 pg/ml. This indicates that in men, the optimal value of 25(OH) D is estimated to be at least 25 ng/ml.
In women: the determined equation was:
The 25(OH) D cut-off point at which PTH reaches its plateau was estimated to be at 30.0 ng/ml; above this value, PTH is stabilized at a virtual plateau, estimated at 26.8 pg/ml. This signifies that in women, the optimal value of 25(OH) D is estimated to be around 30 ng/ml.
Determination of optimal 25(OH) D values according to the season
Optimal 25(OH) D values were determined by season: warm season: summer and autumn, and cold season: winter and spring. The results are presented in Fig. 2-c-S and 2-d-S, respectively.
In the warm season: the determined equation was:
The 25(OH) D cut-off point at which PTH begins to reach its plateau is estimated to be at 30.0 ng/ml, above which PTH is stabilized at a virtual plateau, estimated at 21.5 pg/ml. This means that in the warm season, the optimal value of 25(OH) D would be around 30 ng/ml.
-
In cold season: the determined equation was:
The 25(OH) D cut-off point at which PTH reaches its expected plateau is estimated to be at 25.0 ng/ml, at which point PTH is stabilized at a virtual plateau, estimated at 27.7 pg/ml. This suggests that in the cold season, the optimal value of 25(OH) D is estimated to be at least 25 ng/ml.
Discussion
To the best of our knowledge, this study is the first conducted in Algeria with the aim to define the vitamin D optimal values in the Algerian population.
On the basis of the hypothesis linking vitamin D insufficiency to secondary hyperparathyroidism, several studies around the world have been carried to determine the optimal levels of vitamin D. However, the results are highly discordant and very wide ranges have been reported [21, 22]. In this context, systematic reviews revealed that serum 25(OH) D optimal values as reported by previous studies ranged from 10 to 47 ng/ml, that nearly half of these studies provided estimations of 19 ng/ml and above, and that nearly one-third provided estimations between 15 and 19 ng/ml [23, 24].
This discrepancy could be explained in part by the heterogeneity of the vitamin D and PTH assessment techniques, the study population, the ethnic origin, the inclusion criteria, the season, the latitude, and the statistical methodologies used. Considering all these potential conditions that may influence the relationship between PTH and vitamin D, some organizations have opted for different approaches to set optimal values. In this context, the IOM has established its threshold values based on the interpretation of a series of conceptualized graphs, with panels that relate serum 25(OH)D levels directly to intestinal calcium absorption, adult bone density, and risk of osteomalacia and rickets [9, 10].
To define optimal vitamin D values en the bases of PTH levels, the first stage consists in the selection of the most accurate non-linear regression model to explain the PTH variation according to the 25(OH) D values [1, 20, 21, 25, 26]. In the previous studies, different models were used, with widely varying regression coefficients ranging from 1 to 14% [22, 27]. For example, in a large Dutch study combining data from two surveys, the Longitudinal Aging Study Amsterdam (LASA) and the Netherlands Study of Depression and Anxiety (NESDA), the authors have opted for a restricted cubic spline function model, according to which 6–7% of the PTH variation was explained by the vitamin D variation [27]. In the Korean study, KNHANES IV, the authors had opted for a segmental regression model in which two linear regression models were considered above and below the inflection point, according to this method, the obtained regression coefficient was R2 = 0.1 (11). In the Clalit Health Services (CHS) study, a large study involving more than 13,700 healthy subjects with normal renal function and serum calcium, the authors had selected a quadratic model, estimated using the non-linear least squares approach, according to which only 2.9% of the PTH variation was explained by 25(OH) D levels (1). In the US National Health and Nutrition Examination Survey, including more than 8400 adult subjects of different ethnicity, the authors used a locally weighted estimated scatterplot smoothing (LOWESS) plots to examine the shape of the relationship between serum PTH and 25(OH)D levels. In this study, a biphasic relationship race dependent was observed between this tow parameters. Indeed, whereas 25(OH)D and PTH were inversely related when 25(OH)D values were ≤ 20 ng/ml, the slope of this relationship was essentially flat above this threshold [26].
In our study, the selected model was the inverse nonlinear regression one. Considering its regression coefficient, this model had satisfying predictive abilities, in which 20% of the PTH variation was explained by the 25 (OH) D levels. This satisfactory predictive capacity could be attributed to the chosen non-linear regression curve; indeed, it has been suggested that it represents the most effective method to better describe the shape of the relationship, using more information on the quantitative data compared to the categorization of the data [20, 22]. Moreover, the implementation of very selective inclusion criteria contributes significantly to the improvement of the model. Indeed, the phosphocalcic parameters can be impacted by several bioclinical factors, independently of the vitamin D status, such as severe chronic renal failure, which is characterized by secondary hyperparathyroidism, hypocalcemia, and hyperphosphatemia [1, 28, 29]; diabetes, which can be associated with hyperphosphatemia [20, 29]; morbid obesity, which can be associated with a secondary hyperparathyroid state [1]; and bowel disease causing hypocalcemia, hypomagnesemia, and hypophosphatemia [20, 23]. In our study, all of these factors were contained at the inclusion stage. In addition, subjects with a PTH level higher than twice the upper limit value provided by the assay kit (> 88 pg/ml) and who present normocalcemia or hypercalcemia were also excluded, thus minimizing the risk of primary hyperparathyroidism, independent of vitamin D status [30].
In our study, the total data analysis led to an optimal threshold of 25(OH) D estimated at 26 ng/ml. However, this threshold value should be linked to the assay method used in the present study, i.e., the sequential competitive immuno-fluoroassay on VIDAS®. Indeed, given the lack of standardization of total 25(OH) D assay methods, inter-laboratory differences could be observed even within the same population [18, 31]. Therefore, when comparing previously reported optimal values, it is important to consider not only the ethnicity, age, gender, and geographical situation but also the used assay technique.
Our established threshold value was slightly lower than that proposed by the aforementioned “Clalit Health Services” study, in which the total 25(OH) D was measured by a LIAISON method (DiaSorin USA, Stillwater, Minn); a two-stage competitive chemiluminescence technique. In this study, the optimal value was estimated to be 30 ng/ml, which was similar to the threshold proposed by the ES-CPG [1]. However, our optimal value was much higher compared to those proposed in Asian populations. For example, in the above mentioned KNHANES IV study, total 25(OH) D was measured by radioimmunoassay (DiaSorin, Stillwater, MN); an optimal value was defined as 12.1 ng/ml [11]. The same optimal value was also proposed by a South Chinese study; The Hong Kong Osteoporosis Study, in which vitamin D was measured by a direct enzyme-linked immunosorbent assay (IDS Ltd, UK) [32].
In our study, we further stratified according to two key variables determining vitamin D status: gender and season. This stratification will provide more adapted optimal values and appropriate interpretation of vitamin D status.
When stratified by gender, the optimal value in women was higher than in men (30 ng/ml vs. 25 ng/ml), with also a PTH stabilizing in a higher plateau than that observed in men. The gender difference in optimal values could be explained by two different mechanisms: first, women have usually a lower caloric intake than men, and therefore naturally a lower calcium intake, thus requiring a higher serum 25(OH) D level to ensure more efficient intestinal calcium absorption. Second, women have physiologically a higher body fat percentage than men, and due to its liposoluble nature, 25(OH) D is more highly sequestered in adipose tissue, thus potentially leading to higher threshold levels in women [20].
Among the previous studies defining the 25 (OH) D optimal values by gender, some showed contrasting results to ours. For example, in the Longitudinal Aging Study Amsterdam (LASA), in which 25(OH) D was measured by an immunocompetitive method on Nichols Diagnostics, the authors found lower optimal values in women than in men (17 ng/ml vs. 26 ng/ml, respectively) [20]. Another study also showed contrasting results to ours, the Korean Dong-gu study, in which the authors established optimal values using a micro-particle chemiluminescence technique on ARCHITECT. The optimal value was much lower in women than in men (13.8 ng/ml vs. 21.1 ng/ml) (21).
When stratifying by season, our results suggest that the optimal value is higher during the warm season (30 ng/ml vs. 25 ng/ml). These defined optimal values had a significant impact on the plateau reached by PTH (21.5 pg/ml vs. 27.7 pg/ml, respectively). This difference is expected, and could be explained by the seasonal variability of the endogenous vitamin D synthesis, which is naturally limited by the availability of ultraviolet-B radiation during the cold season, and which leads to a physiological elevation of PTH in order to compensate the vitamin D deficit. Some authors have proposed to define optimal 25(OH) D values according to the season, rather than simply adjusting for this factor, but current data are very scarce, and no international recommendations have been proposed [4].
Our study has several limitations. First, it is a single-center study, targeting the residents of a single city in northern Algeria, which is not representative of the entire general Algerian population. Second, the method used for the measurement of total 25(OH) D, based on an enzyme immunoassay technique with fluorometric detection instead of liquid chromatography tandem mass spectroscopy (LCMS), which represents a more accurate and recognized technique for measuring vitamins. Third, this is a cross-sectional study; the vitamin D determination was performed in a single punctual manner and therefore does not reflect seasonal variability at the individual scale. Fourth, the sample size was limited during the warm season; this could affect the reliability around the cut-off point due to the sparse distribution of observed values. Further studies with a larger sample size are therefore required to validate the cut-off values set in this study. Fifth, the dietary survey could not be included in the study analysis owing to the lack of precision in reported food consumption amounts and frequencies, thus making it difficult to control for the effect of daily calcium intake. The strength of the study resides in the population diversity, including subjects of both genders, with ages ranging from 19 to 79 years, the application of rigorously designed exclusion criteria in order to control for factors that affect phosphocalcic metabolism, and finally the definition of optimal values stratified by gender and sampling season.
In conclusion, as a result of this study, we have defined, for the first time, the 25(OH)D optimal values in a North Algerian population aged between 19 and 79 years. In men, the 25(OH)D optimal value is 25.0 ng/ml for a PTH level of 22.3 pg/ml. In women, the 25 (OH) D optimal values is 30 ng/ml for a PTH concentration of 26.8 pg/ml. In addition, in the warm season (summer and autumn), the optimal value of 25(OH) D is 30 ng/ml for a PTH level of 21.5 ng/ml, and in the cold season, this value should be at least 25 ng/ml for a PTH level of 27 pg/ml.
References
Saliba W, Barnett O, Rennert HS, Lavi I, Rennert G (2011) 16.b. The relationship between serum 25(OH)D and parathyroid hormone levels. American J Med 124(12):1165–70
Annweiler C, Beauchet O. 10.b. Vitamin D in older adults: the need to specify standard values with respect to cognition. Front Aging Neurosci [Internet]. 15 avr 2014 [cité 29 mai 2021];6. Disponible sur: http://journal.frontiersin.org/article/https://doi.org/10.3389/fnagi.2014.00072/abstract
Szabó B, Tabák ÁG, Toldy E, Szekeres L, Szili B, Bakos B et al (2017) 20.b.The role of serum total and free 25-hydroxyvitamin D and PTH values in defining vitamin D status at the end of winter: a representative survey. J Bone Miner Metab 35(1):83–90
Souberbielle JC (2014) 21.a. Épidémiologie du déficit en vitamine D. Cahiers de Nutrition et de Diététique. 49(6):252–9
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP et al (2011) 28.a. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metabolism 96(7):1911–30
Deplanque X, Wullens A, Norberciak L (2017) 1.a. Prévalence et facteurs de risque de l’insuffisance en vitamine D chez l’adulte sain entre 18 et 65 ans dans le Nord de la France. La Revue de Médecine Interne 38(6):368–73
Liu X, Baylin A, Levy PD (2018) 15.a. Vitamin D deficiency and insufficiency among US adults: prevalence, predictors and clinical implications. Br J Nutr 119(8):928–36
van Schoor NM, Lips P (2011) 19.a. Worldwide vitamin D status. Best Pract Res Clin Endocrinol Metabolism. 25(4):671–80
Rosen CJ, Abrams SA, Aloia JF, Brannon PM, Clinton SK, Durazo-Arvizu RA et al (2012) IOM Committee Members Respond to Endocrine Society Vitamin D Guideline. J Clin Endocrinol Metab 97(4):1146–1152
Bouillon R, Rosen C. (2018)The IOM–Endocrine Society Controversy on Recommended Vitamin D Targets. In: Vitamin D. Elsevier; p. 1065‑89.
Hwang YC, Ahn HY, Jeong IK, Ahn KJ, Chung HY (2013) 6.b. Optimal serum concentration of 25-hydroxyvitamin D for bone health in older Korean adults. Calcif Tissue Int 92(1):68–74
Bouillon R, Van Schoor NM, Gielen E, Boonen S, Mathieu C, Vanderschueren D et al (2013) 21.b.Optimal vitamin D status: a critical analysis on the basis of evidence-based medicine. J Clin Endocrinol Metabolism 98(8):E1283-304
Malabanan A, Veronikis I, Holick M (1998) 25.b. Redefining vitamin D insufficiency. The Lancet 351(9105):805–6
Singhellakis P, Malandrinou F, Psarrou C, Danelli A, Tsalavoutas S, Constandellou E (2011) 9.b. Vitamin D deficiency in white, apparently healthy, free-living adults in a temperate region. HJ. 10(2):131–43
Lopez AG, Kerlan V, Desailloud R (2021) 31.b. Non-classical effects of vitamin D: non-bone effects of vitamin D. Annales d’Endocrinologie. 82(1):43–51
Wimalawansa SJ, Razzaque MS, Al-Daghri NM (2018) 30.b. Calcium and vitamin D in human health: hype or real? J Steroid Biochem Molecular Biol 180:4–14
Katrinaki M, Kampa M, Margioris A, Castanas E, Malliaraki N (2016) 38 a Vitamin D levels in a large Mediterranean cohort: reconsidering normal cut off values. HJ. 15(2):205–23
Sempos CT, Heijboer AC, Bikle DD, Bollerslev J, Bouillon R, Brannon PM et al (2018) 22.b. Vitamin D assays and the definition of hypovitaminosis D: results from the First International Conference on Controversies in Vitamin D: Vitamin D assays and defining hypovitaminosis D. Br J Clin Pharmacol 84(10):2194–207
Netgen. (2021) 20.a. Vitamine D : actualité et recommandations [Internet]. Revue Médicale Suisse. [cité 10 avr 2021]. Disponible sur: https://www.revmed.ch/RMS/2011/RMS-319/Vitamine-D-actualite-et-recommandations
Sohl E, de Jongh RT, Heymans MW, van Schoor NM, Lips P (2015) 1.b. Thresholds for serum 25(OH)D concentrations with respect to different outcomes. J Clin Endocrinol Metabolism 100(6):2480–8
Choi SW, Kweon SS, Choi JS, Rhee JA, Lee YH, Nam HS et al (2015) 2.b. Estimation of the cutoff value of vitamin D: the Dong-gu study. J Physiol Anthropol 34(1):10
Wright NC, Chen L, Niu J, Neogi T, Javiad K, Nevitt MA et al (2012) 13.b. Defining physiologically “normal” vitamin D in African Americans. Osteoporos Int 23(9):2283–91
Aloia JF, Chen DG, Chen H (2010) 5.b. The 25(OH)D/PTH Threshold in Black women. J Clin Endocrinol Metabolism 95(11):5069–73
Aloia JF, Talwar SA, Pollack S, Feuerman M, Yeh JK (2006) 33.b. Optimal vitamin D status and serum parathyroid hormone concentrations in African American women. American J Clin Nutrition 84(3):602–9
Touvier M, Deschasaux M, Montourcy M, Sutton A, Charnaux N, Kesse-Guyot E et al (2014) 17.b. Interpretation of plasma PTH concentrations according to 25OHD status, gender, age, weight status, and calcium intake: importance of the reference values. J Clin Endocrinol Metabolism 99(4):1196–203
Li M, Lv F, Zhang Z, Deng W, Li Y, Deng Z et al (2016) 18 b Establishment of a normal reference value of parathyroid hormone in a large healthy Chinese population and evaluation of its relation to bone turnover and bone mineral density. Osteoporos Int 27(5):1907–16
Deckers MML, de Jongh RT, Lips PTAM, Penninx BWJH, Milaneschi Y, Smit JH et al (2013) 15.b. Prevalence of vitamin D deficiency and consequences for PTH reference values. Clinica Chimica Acta 426:41–5
Gutiérrez OM, Farwell WR, Kermah D, Taylor EN (2011) 12.b. Racial differences in the relationship between vitamin D, bone mineral density, and parathyroid hormone in the National Health and Nutrition Examination Survey. Osteoporos Int 22(6):1745–53
Allgrove J. (2015) 32.b. Physiology of calcium, phosphate, magnesium and vitamin D. In: Allgrove J, Shaw NJ, éditeurs. Endocrine development [Internet]. S. Karger AG; [cité 29 mai 2021]. p. 7‑32. Disponible sur: https://www.karger.com/Article/FullText/380990
Souberbielle JC, Massart C, Brailly-Tabard S, Cormier C, Cavalier E, Delanaye P et al (2016) 19.b. Serum PTH reference values established by an automated third-generation assay in vitamin D-replete subjects with normal renal function: consequences of diagnosing primary hyperparathyroidism and the classification of dialysis patients. European J Endocrinol 174(3):315–23
Ferreira CES, Maeda SS, Batista MC, Lazaretti-Castro M, Vasconcellos LS, Madeira M, et al. (2017) 24.b. Consensus – reference ranges of vitamin D [25(OH)D] from the Brazilian medical societies. Brazilian Society of Clinical Pathology/Laboratory Medicine (SBPC/ML) and Brazilian Society of Endocrinology and Metabolism (SBEM). Jornal Brasileiro de Patologia e Medicina Laboratorial [Internet].[cité 29 mai 2021];53(6). Disponible sur: http://www.gnresearch.org/doi/https://doi.org/10.5935/1676-2444.20170060
Leung RY, Cheung BM, Nguyen US, Kung AW, Tan KC, Cheung CL (2017) 7.b. Optimal vitamin D status and its relationship with bone and mineral metabolism in Hong Kong Chinese. Bone 97:293–8
Acknowledgements
We wholeheartedly thank all subjects for their generous participation in the present study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was conducted in accordance with the Declaration of Helsinki and approved by the local ethics committee.
Informed consent
Informed consent was obtained from all subjects before enrollment in this study.
Conflict of interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bennouar, S., Bachir Cherif, A., Makrelouf, M. et al. Reconsidering vitamin D optimal values based on parathyroid hormone levels in a North Algerian cohort: stratification by gender and season. Arch Osteoporos 17, 100 (2022). https://doi.org/10.1007/s11657-022-01137-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-022-01137-2