Abstract
Summary
This study was designed to determine a FRAX intervention threshold in postmenopausal Thais, based on a history of hip fracture. The optimal FRAX thresholds for hip fracture were 4.9% (without BMD) and 4% (with BMD), while the thresholds for major osteoporotic fracture were 9.8% (without BMD) and 8.9% (with BMD).
Introduction
Fracture Risk Assessment Tool (FRAX) has been widely used as an intervention threshold for initiating osteoporosis treatment. However, there is a lack of data to validate the threshold in Thai population.
Methods
A cross-sectional study was conducted from January 2014 to February 2019. Postmenopausal women in the Northeast of Thailand whom has bone mineral density (BMD) measured using dual-energy X-ray absorptiometry (DXA) in the study period were recruited. Participants who had previously received anti-osteoporotic treatment were not eligible. FRAX score, both with and without BMD, was calculated using a Thai reference. Prevalent hip fracture was identified by reviewing the ICD-10 diagnosis from the hospital database during the study period. The receiver operating characteristic (ROC) curve and Youden index were used to determine the FRAX threshold in predicting hip fracture, based on the rationale that women with a prevalent hip fracture would be eligible for treatment.
Results
A total of 2872 postmenopausal Thai women were recruited, with 45 sustained a recent hip fracture. In association with hip fracture, the optimal FRAX thresholds for hip fracture without and with BMD were 4.9% and 4%, respectively, with 71.1% sensitivity and 83.3% specificity, and 82.2% sensitivity and 78.6% specificity, while the optimal FRAX thresholds for major osteoporotic fracture (MOF) without and with BMD were 9.8% and 8.9%, respectively, with 75.6% sensitivity and 77.0% specificity, and 86.7% sensitivity and 70.9% specificity.
Conclusion
An optimal intervention threshold based on FRAX of hip fracture and MOF in postmenopausal Thai women is slightly different from the standard recommendation, which confirmed the marked variations of thresholds across ethnicities. The proposed threshold should be considered as new cutoff for initiating osteoporosis treatment in postmenopausal Thais.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporotic fractures, particularly hip fractures and major osteoporotic fractures (MOF), are becoming a major public health concern worldwide due to their association with increased mortality and high costs [1, 2]. Anti-osteoporotic medications were generally recommended if the bone mineral density (BMD) T-score was − 2.5 or less as determined by dual-energy X-ray absorptiometry (DXA). However, previous studies have shown that using BMD alone is a low-sensitivity test. According to Wainwright et al., 54% of older women with hip fractures were not in the osteoporotic range based on BMD assessment, and several factors, such as advanced age, lack of exercise, and fall within the previous year, were associated with an increased risk of hip fracture [3]. Siris et al. found that only one-fifth of hip fracture patients had a BMD T-score of − 2.5 or less, and they proposed incorporating clinical risk factors into decision-making for postmenopausal women with low BMD [4].
The Fracture Risk Assessment Tool (FRAX) was developed in response to the limitations of BMD. This tool calculates the 10-year probability of major osteoporotic and hip fractures, based on age, gender, body mass index (BMI), and other risk factors such as smoking, rheumatoid arthritis, glucocorticoid usage, and secondary causes of osteoporosis, with femoral neck BMD as an optional input variable [5]. FRAX’s fracture prediction performance outperformed that of BMD alone [6]. Furthermore, FRAX has been included in a number of clinical practice guidelines for estimating the 10-year fracture probability and considering treatment in high-risk individuals, with intervention thresholds varying across countries [7]. According to the Thai Osteoporosis Foundation (TOPF) guideline, individuals with a 10-year risk of hip fracture of 3% or more were considered to be receiving treatment to prevent osteoporosis-related fractures [8]. This cut-off value, on the other hand, was largely determined by a consensus among field specialists using data from Europe and the USA [9]. There is a scarcity of data to confirm this intervention threshold for postmenopausal Thai women with hip fracture. Furthermore, there is no intervention threshold for MOF in the TOPF guideline [8]. The aim of this study was therefore to determine the FRAX-based intervention threshold in postmenopausal Thai women using FRAX of hip fracture and MOF in association with a recent hip fracture.
Methods
A cross-sectional study was conducted at Srinagarind Hospital, a tertiary care setting in Northeast Thailand. Postmenopausal Thai women aged 40 to 90 years old who had their BMD measured for osteoporosis between January 2014 and February 2019 were recruited. Participants who had previously received anti-osteoporotic treatment were not eligible. Following completion of the consent form, participants were evaluated using the FRAX questionnaire for demographic data and clinical risk factors. Body weight (with light indoor clothing) was measured with an electronic scale (precision 0.1 kg [kg]) and standing height (without shoes) was measured using a stadiometer (nearest 0.1 cm). Body mass index (BMI) was calculated by dividing weight in kilograms by height in square meters (m2). Femoral neck BMD (FNBMD) was measured using Lunar Prodigy densitometer (GE Healthcare, Madison, WI, USA) in all participants. The FRAX of hip fracture and MOF in each participant, without and with the inclusion of BMD, were calculated using a Thai reference (https://www.sheffield.ac.uk/FRAX/tool.aspx?country=9). FNBMD value was entered as an input variable to compute FRAX probabilities for the FRAX with BMD calculation. The receiver operating characteristic (ROC) curve and Youden index were used to determine the FRAX threshold in predicting hip fracture, with the rationale that women who sustain a hip fracture would be eligible for osteoporosis treatment. A review of the ICD-10 diagnoses from the hospital database, as well as the medical record and film X-ray between January 2014 and February 2019, identified the event of hip fracture that occurred within 1 year either before or after the BMD test. All study protocols were followed in accordance with applicable guidelines and regulations. The Khon Kaen University Human Research Ethics Committee reviewed and approved the study in accordance with the Helsinki Declaration and the Good Clinical Practice Guidelines (HE581241).
Statistical analyses
All data was computed using IBM SPSS Statistics 26, which was provided by Khon Kean University. Demographic data was computed and presented as medians and interquartile ranges (IQR). The P-value was calculated using the Mann–Whitney U test, which was used to compare variables between groups. The ROC curve of FRAX score was constructed and presented in terms of sensitivity, specificity, and false positive rate to predict a prevalent hip fracture. Youden index (Sensitivity + Specificity − 1) was used to determine the ROC data cut-off point.
Results
In this study, 2872 postmenopausal women aged 40 to 90 years were recruited. During the study period, 45 participants (1.6%) sustained a hip fracture. Women with a history of hip fracture were significantly older, had lower body weight and BMI, and lower BMD at both the lumbar spine and the femoral neck; whereas FRAX score, with or without BMD, was significantly higher in women with a history of fracture than those without a history of hip fracture (Table 1).
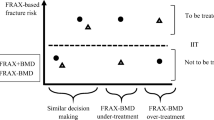
The correlations between FRAX of hip fracture with and without BMD, and FRAX of MOF with and without BMD were significant in this study (r = 0.670–0.937, p < 0.001). However, the correlations between FRAX of hip fracture and MOF with BMD (r = 0.937, p < 0.001), and FRAX of hip fracture and MOF without BMD (r = 0.923, p < 0.001) were stronger. The ROC curves for FRAX of hip fracture without BMD (solid line) and with BMD (fine dash line) were shown (Fig. 1A). The area under the curves (AUCs) of FRAX of hip fracture without BMD and with BMD were 0.838 (95% CI: 0.781 to 0.895) and 0.861 (95%CI: 0.824 to 0.899), respectively. Based on the highest Youden index, the best FRAX threshold in association with hip fracture using FRAX of hip fracture without BMD was 4.9%, with 71.1% sensitivity, 83.3% specificity, and 16.7% false positive rate. The sensitivity, specificity, and false positive rate were 77.8%, 69.7%, and 30.3%, respectively, when compared to the previous recommendation cutoff (3%). Based on the highest Youden index, the best FRAX threshold using FRAX of hip fracture with BMD was 4%, with 82.2% sensitivity, 78.6% specificity, and 21.4% false positive rate, whereas the sensitivity, specificity, and false positive rate for a 3% cutoff were 84.4%, 70.3%, and 29.7%, respectively (Table 2).
Receiver operating characteristic (ROC) curve of FRAX of hip fracture without BMD (solid line), FRAX of hip fracture with BMD (dashed line). A Receiver operating characteristic (ROC) curve of FRAX of major osteoporosis fracture without BMD (solid line), and FRAX of major osteoporosis fracture with BMD (dashed line) (B). MOF major osteoporotic fracture, BMD bone mineral density
In addition, the ROC curves of FRAX of MOF without BMD (solid line) and with BMD (fine dash line) in association with prevalent hip fracture were calculated (Fig. 1B). The AUCs of FRAX for MOF without BMD and with BMD were 0.833 (95% CI: 0.778 to 0.888) and 0.830 (95%CI: 0.776 to 0.884), respectively. The FRAX thresholds in association with prevalent hip fracture using FRAX of MOF without and with BMD were 9.8% (with 75.6% sensitivity, 77.0% specificity, and 23.0% false positive rate) and 8.9 (with 86.7% sensitivity, 70.9% specificity, and 29.1% false positive rate), respectively, based on the highest Youden index. In contrast, when the National Osteoporosis Foundation (NOF) recommended 20% cutoff for both FRAX of MOF without and with BMD [1], the sensitivity was low (15.6–17.8%), while the specificity was high (96.6–97.5%) (Table 3).
Discussion
The aim of this study was to find the intervention threshold for both FRAX of hip fracture and FRAX of MOF in postmenopausal Thai women and as an eligibility criterion for intervention, a prevalent hip fracture was used in the present study. We found that the proper intervention threshold using FRAX of hip fracture was 4.9% if BMD was not included in the calculation, and 4% if BMD was included. We also found that the optimal threshold for FRAX MOF treatment without and with BMD was 9.8% and 8.9%, respectively. According to the NOF recommendations, patients with a BMD T-score between − 1.0 and − 2.5 at the femoral neck or lumbar spine and a 10-year probability of hip fracture of ≥ 3% or a 10-year probability of MOF of ≥ 20% as assessed by FRAX should be treated [1]. This 3% intervention threshold recommendation was derived from the cost-effective analysis in the USA, which found that osteoporosis treatment was cost-effective when the 10-year probability of hip fracture reached 3% [10]. However, there is debate about the sensitivity and specificity of this FRAX intervention threshold across ethnicities [9]. Several Asian studies suggest that different thresholds exist for Asian people [11,12,13,14]. In our study, the FRAX of hip fracture was slightly higher than the NOF and TOPF recommendation (FRAX of hip fracture threshold of 4% with BMD, and 4.9% without BMD). Similarly, the study in Sri Lanka by Lekamwasem S et al. found that the intervention threshold of hip fracture probabilities 3.5%, which provided the lowest misclassification and the highest agreement, was higher than the standard recommendation. [11]. However, some studies have found a lower cutoff for the intervention. In postmenopausal Singaporean women, Chandran et al. reported a fixed (age-independent) threshold for hip fracture probabilities of 1% [12]. In addition, Zhang et al. observed that a fixed intervention threshold for hip fracture probabilities in central south postmenopausal Chinese women was only 1.3% [13]. The disparity in cut-off levels could be explained by ethnic differences as well as differences in the gold standard of intervention threshold in each report. Many studies, included those in Sri Lanka [15], Singapore [12], and India [16], used a previous fragility fracture as the gold standard in developing age-dependent intervention thresholds, while the intervention threshold has been established based on economic analyses in Taiwan [17], Australia [18], and Japan [19].
In Thailand, the prevalence of osteoporosis in postmenopausal women using BMD T-score ≤ − 2.5 is estimated to be between 13 and 19% [20, 21]. According to a study conducted between 2010 and 2018, the FRAX score has been wildly used in Thailand [22]. Using the new threshold of 4% (FRAX of hip fracture with BMD) and 4.9% (FRAX of hip fracture without BMD) thresholds, our study found that 643 patients (22.4%) and 504 patients (17.5%) in this population would be eligible for treatment. As a result, our proposed cutoff should allow for adequate intervention in high-risk patients for better osteoporosis fracture prevention.
This study also demonstrated a ROC curve in relation with prevalent hip fracture in order to determine the best cut-off point for FRAX of MOF. According to the NOF [1], the recommended cut-off value of 20% has high specificity but very low sensitivity. In our study, a lower threshold of 8.9% for FRAX of MOF with BMD and 9.8% for FRAX of MOF without BMD performed better in terms of sensitivity. This finding was consistent with a previous study in the Vietnamese population using Thai FRAX as a reference, which reported that only 1% and 0.1% of women and men had 10-year risk of MOF ≥ 20%, respectively [23]. Because the FRAX of MOF intervention threshold was not included in the current Thai guideline, we believed that the FRAX of MOF cutoff derived from our study should be considered as an intervention threshold for Thais, based on the rationale that this threshold performed best in association with hip fracture probabilities that would also be eligible for treatment.
Our study is the first to define the optimal intervention threshold of hip fracture probabilities in postmenopausal Thai women using a large sample size and comprehensive data from a hospital database. However, there are some limitations to our study that should be mentioned. First, our study was a cross-sectional observational study. Because DXA scans are not available in every hospital in Thailand, many participants experienced fractures and were later transferred to a tertiary hospital for DXA scans. It is possible that our results were influenced by the difference in the patients’ characteristics between fracture and non-fracture group, and we lacked long-term follow-up data on the incidence of hip fractures that occurred after the study period. This might affect our cut-off point for FRAX of hip fracture and since we used only hip fracture as the event, it may cause our cut-off point for FRAX of MOF to be lower than usual. Second, we lacked information on other osteoporosis fractures, such as vertebral or wrist fractures, resulting in an underestimation of participants who would be eligible for osteoporosis treatment. In addition, there could have been some recall bias when the participants completed the FRAX questionnaire, which could have influenced the results. Third, our participants are mostly from the Thailand’s north-eastern region, which may not representative of the entire Thai population. Finally, we did not conduct a cost-effectiveness analysis. More research into the cost-effectiveness of selecting theses thresholds in Thailand should be expected.
In conclusion, the FRAX-based intervention threshold for FRAX of hip fracture with BMD of 4% provides satisfied accuracy as an osteoporosis treatment threshold for fracture prevention in postmenopausal Thai women. However, if the BMD measurement was unavailable, the intervention threshold should be 4.9% without BMD should be considered. In addition, FRAX of MOF with and without BMD of 8.9% and 9.8%, respectively, should be considered as an alternative intervention threshold in postmenopausal Thais.
References
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S et al (2014) Clinician’s Guide to prevention and treatment of osteoporosis. Osteoporos Int 25(10):2359–2381
Harvey N, Dennison E, Cooper C (2010) Osteoporosis: impact on health and economics. Nat Rev Rheumatol 6(2):99–105
Wainwright SA, Marshall LM, Ensrud KE, Cauley JA, Black DM, Hillier TA et al (2005) Hip Fracture in women without osteoporosis. J Clin Endocrinol Metab 90(5):2787–2793
Siris ES, Brenneman SK, Miller PD, Barrett-Connor E, Chen Y-T, Sherwood LM et al (2004) Predictive value of low BMD for 1-year fracture outcomes is similar for postmenopausal women ages 50–64 and 65 and older: Results from the National Osteoporosis Risk Assessment (NORA). J Bone Miner Res 19(8):1215–1220
FRAX ® FRAX – Fracture Risk Assessment Tool [Internet]. [cited 2021 Jan 25]. Available from: https://www.sheffield.ac.uk/FRAX/tool.aspx?lang=th
Kanis JA, Oden A, Johnell O, Johansson H, De Laet C, Brown J et al (2007) The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int 18(8):1033–1046
Johansson H. FRAX- vs. T-score-based intervention thresholds for osteoporosis. Osteoporos Int. 2017 Nov;28(11):3099–105.
Songpatanasilp T, Sritara C, Kittisomprayoonkul W, Chaiumnuay S, Nimitphong H, Charatcharoenwitthaya N et al (2016) Thai Osteoporosis Foundation (TOPF) position statements on management of osteoporosis. Osteoporos Sarcopenia 2(4):191–207
Kanis JA, Harvey NC, Cooper C, Johansson H, Odén A, McCloskey EV. A systematic review of intervention thresholds based on FRAX : a report prepared for the National Osteoporosis Guideline Group and the International Osteoporosis Foundation. 2017;101.
Tosteson ANA, Melton LJ, Dawson-Hughes B, Baim S, Favus MJ, Khosla S et al (2008) Cost-effective osteoporosis treatment thresholds: the United States perspective. Osteoporos Int 19(4):437–447
Lekamwasam S (2013) Sri Lankan FRAX model and country-specific intervention thresholds. Arch Osteoporos 8(1–2):148
Chandran M (2018) FRAX® based intervention thresholds for management of osteoporosis in Singaporean women. Arch Osteoporos 13(1):130
Zhang Z, Ou Y, Sheng Z, Liao E (2014) How to decide intervention thresholds based on FRAX in central south Chinese postmenopausal women. Endocrine 45(2):195–197
Fujiwara S, Nakamura T, Orimo H, Hosoi T, Gorai I, Oden A, et al. Development and application of a Japanese model of the WHO fracture risk assessment tool (FRAXTM). Osteoporos Int. 2008;7.
Lekamwasam S, Chandran M, Subasinghe S (2019) Revised FRAX®-based intervention thresholds for the management of osteoporosis among postmenopausal women in Sri Lanka. Arch Osteoporos 14(1):33
Kanis J (2013) Commentary on guidelines on postmenopausal osteoporosis - Indian Menopause Society. J -Life Health 4(2):129–131
Chan D-C, McCloskey EV, Chang C-B, Lin K-P, Lim LC, Tsai K-S et al (2017) Establishing and evaluating FRAX® probability thresholds in Taiwan. J Formos Med Assoc Taiwan Yi Zhi 116(3):161–168
Chen JS, Simpson JM, Blyth FM, March LM (2014) Managing osteoporosis with FRAX® in Australia: proposed new treatment thresholds from the 45&Up Study cohort. Bone 69:148–153
Kanis JA, Johansson H, Oden A, McCloskey EV. The distribution of FRAXÒ-based probabilities in women from Japan. J Bone Min Metab. 2012;6.
Pongchaiyakul C, Songpattanasilp T, Taechakraichana N (2008) Burden of osteoporosis in Thailand. Int J Rheum Dis 11(4):335–340
Pongchaiyakul C, Leerapun T, Wongsiri S, Songpattanasilp T, Taechakraichana N (2012) Value and validation of RCOST and TOPF clinical practice guideline for osteoporosis treatment 95(12):8
Chotiyarnwong P, Harvey NC, Johansson H, Liu E, Lorentzen M, Kanis JA et al (2019) Temporal changes in access to FRAX® in Thailand between 2010 and 2018. Arch Osteoporos 14(1):66
Hoang DK, Doan MC, Mai LD, Ho-Le TP, Ho-Pham LT. Burden of osteoporosis in Vietnam: an analysis of population risk. PLos One. 2021;16(6):e0252592.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sribenjalak, D., Charoensri, S. & Pongchaiyakul, C. An optimal intervention threshold of FRAX in postmenopausal Thai women. Arch Osteoporos 17, 21 (2022). https://doi.org/10.1007/s11657-022-01058-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-022-01058-0