Abstract
Summary
This paper revised the fixed intervention thresholds (ITs) based on the Sri Lankan fracture risk assessment tool (FRAX) published in 2013 and introduced new ITs, hybrid and two-tier, aiming to help clinicians in the management of postmenopausal osteoporosis. The hybrid and two-tier ITs have a better discriminatory power than age-dependent and revised fixed ITs.
Introduction
This study revised the Sri Lankan FRAX®-based intervention thresholds (ITs) previously published in 2013.
Method
Age-dependent ITs were estimated, from 50–80 years with 5-year intervals, using a Sri Lankan FRAX® algorithm for a woman with a BMI of 24.8 kg/m2 and history of prior fragility fracture without other clinical risk factors. Data of 653 postmenopausal women were used in estimating fixed, hybrid, and two-tier ITs. ITs were determined using the ROC curve and partial Youden index. New ITs were validated using data of 356 postmenopausal women who underwent DXA and 62 women who had a recent fragility fracture. Women in the two groups (n = 653 and n = 356) came from the Southern Province and had undergone DXA in our state-owned tertiary care hospital as a part of their routine clinical assessment.
Results
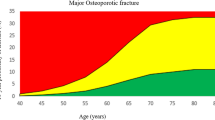
The mean (SD) age and BMI of the subjects (n = 653) were 62 (8) years and 24.8 (1.2) kg/m2, respectively. Age-dependent ITs of major osteoporotic fracture risk (MOFR) and hip fracture risk (HFR) ranged from 2.7 to 18% and from 0.4 to 7.1%. The best fixed ITs for women aged 50–80 years were 9% for MOFR and 3% for HFR. In the hybrid method, MOFR of 6% and HFR of 2% were found appropriate for women aged < 70 years. These were combined with age-dependent ITs for women aged 70 years and above. In the two-tier system, two sets of ITs were calculated (ITs of MOFR/HFR for women aged < 70 years and ≥ 70 years were 6%/2% and 12%/5%, respectively). When age-dependent ITs were considered the reference standard, sensitivities of the fixed, hybrid, and two-tier ITs were 0.63, 0.73, and 0.74, respectively. The specificities were 0.76, 0.86, and 0.80 in the same order. Sensitivities of the age-dependent, fixed, hybrid, and two-tier ITs in identifying a woman with an incident fracture were 26%, 48%, 61%, and 61%, respectively.
Conclusions
The new fixed MOFR is slightly lower than the previous value and hybrid and two-tier ITs perform better than age-dependent and fixed ITs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The fracture risk assessment tool (FRAX®) is the most extensively studied and validated tool in the management of osteoporosis [1, 2]. In 2017, FRAX® was available in 63 countries covering 79% of the world population [1]. Country-specific FRAX® tools are considered to generate more accurate information since they are based on own fracture and mortality data [3]. FRAX®-based assessments are cost effective [4] and used in baseline risk assessment in clinical trials [5].
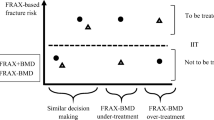
For an efficient application, FRAX® output needs to be combined with intervention thresholds (ITs) [1]. ITs help clinicians in recognizing high-risk patients and making individualized therapeutic decisions. Similar to FRAX®, ITs need to be country specific as the decision to treat a patient depends on many factors such as cost effectiveness of interventions, country health expenditure, and willingness to pay for health at the country and individual levels [6].
Although many countries have their own FRAX algorithms, only few countries have developed their own ITs. According to a systematic review published in 2016, FRAX® was included in the 120 management guidelines or scholarly recommendations but only 82 included recommendations based on ITs [1]. Country-specific ITs are limited in Asia [7,8,9] and this gap in the Asia Pacific region is a major concern [10].
Countries have adopted different principles in developing ITs and they include economic evaluations, epidemiological data, and theories based on clinical assumptions [1]. The forms of ITs also vary, and fixed, age-dependent, and hybrid ITs have been developed. Among the 120 FRAX®-based guidelines in 2016, 58 recommended fixed ITs, 22 recommended age-dependent ITs, while 2 recommended the use of both [1]. It is intuitive to consider that age-dependent ITs are more accurate than others since fracture risk and fracture incidence are age related. Other forms such as fixed and hybrid ITs [11] are, however, likely to be more user-friendly. Countries with ethnic diversity face the challenge of finding ethnic-specific ITs for the particular country. Ethnic-specific ITs for Chinese, Malay, and Indian Singaporean published recently show a wide disparity highlighting the need of separate ITs for subpopulations [9].
Some countries have revised ITs published previously. For instance, in 2014, Australia revised previous ITs based on an analysis of 213,375 men and women aged 50 years or more living in New South Wales. This is logical as accumulating epidemiological and clinical data and changes in economic indices are likely to generate more robust evaluations. ITs based on a Sri Lankan FRAX® algorithm were published in 2013 in order to bring uniformity to clinical and therapeutic decision making in the country [8]. This was based on an analysis of 350 randomly selected, community-dwelling postmenopausal women who underwent DXA. Notable changes have taken place since the last publication, and newer methods of estimating ITs such as hybrid and weighted ITs have been introduced [9, 11]. Furthermore, our database has expanded with more data, and we considered that it is important to revise the ITs published previously and also to validate them using cross-sectional analyses.
Methods
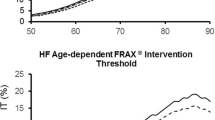
Age-dependent intervention thresholds
Age-dependent intervention thresholds, first developed by the National Osteoporosis Guideline Group (NOGG), are based on the rationale that if a woman with a prior fragility fracture is eligible for treatment, then, at any given age, a man or woman with the same fracture probability but in the absence of a previous fracture should also be eligible [12]. Based on this rationale, we calculated ITs for different ages from 50 to 80 years, with 5-year intervals, for a woman with a BMI of 24.8 kg/m2 with a previous fragility fracture sans other clinical risk factors.
Fixed intervention thresholds
We used a database of 653 postmenopausal women who underwent DXA between 2016 and 2018 for the evaluation of fracture risk. These women had been referred for the evaluation of fracture risk as a part of routine clinical management by clinicians in the Southern Province. This unit provides a DXA facility for the entire Southern Province, free of charge, and captures patients from a wide geographical area and all ethnicities. All patients had information on clinical risk factors collected using a predesigned questionnaire and DXA performed by a single technician adhering to the manufacturer’s protocols (Hologic Inc., Bedford, MA, USA). The questionnaire used included information on medication, co-morbidity, substance use, and clinical risk factors especially those included in the FRAX model. Their height and weight were measured with a stadiometer (NAGATA, Taiwan). After excluding the DXA reports with incomplete data and technical faults (n = 10), we estimated the major osteoporotic fracture risk (MOFR) and hip fracture risk (HFR) of the remaining patients using the Sri Lankan FRAX® algorithm with femoral neck BMD input. Women were divided into two groups, those requiring intervention (equal or above the age-dependent ITs) and those not requiring intervention (below the age-dependent ITs). ROC analyses were performed with the need of intervention as the dependent variable and MOFR and HFR as independent variables. AUCs were assessed and fixed ITs, for both MOFR and HFR, were determined. In determining fixed ITs, we used the Youden index (sensitivity + (1-specificity)) [13] and in a given Youden index, the point that gave the best sensitivity and specificity (partial Youden index) [14].
Hybrid intervention thresholds
We adhered to the method previously followed by Chakhtoura et al. in developing hybrid ITs [11]. In the hybrid method, a combination of ITs, age-dependent for one group and fixed for another group, is used. Chakhtoura et al. selected women aged < 70 years for fixed ITs and women aged ≥ 70 years for age-dependent ITs. Adopting this method, fixed ITs were developed for women aged < 70 years and age-dependent ITs for women aged ≥ 70 years.
Two-tier intervention thresholds
In order to give two-tier ITs, we constructed separate ROC curves for those aged < 70 years and ≥ 70 years and applied the same principles in determining the most appropriate fixed ITs.
Validity of intervention thresholds
The validity of ITs was first tested with a separate group of postmenopausal women (n = 356) who had undergone DXA evaluation. Similar to the women included in the development of ITs, women in this group had been referred by clinicians in the Southern Province for the estimation of fracture risk as a part of routine clinical evaluation. These women were categorized into two groups, high and low risk, according to the different ITs developed above. They were considered to have a high risk if they exceeded either the MOFR or the HFR of a given set of ITs. The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of the fixed ITs, hybrid ITs, and two-tier ITs were estimated considering the age-dependent ITs as the reference standard.
The sensitivities of all ITs, including the age-dependent, were tested using a group of women (n = 62) who had undergone DXA evaluation within 1 month of a fragility fracture (radiographically confirmed hip, vertebral, or distal forearm) to assess the proportion of women who could have been identified as high risk if they had undergone DXA and FRAX® evaluation the day before the fracture. MOFR and HFR were calculated incorporating clinical risk factors and femoral neck BMD but not taking the fracture into consideration [15, 16].
Results
The mean (SD) age and BMI of the women who were used to develop ITs were 62 (8) years and 24.8 (1.3) kg/m2, respectively; none had ever smoked; and only 0.1% had ever consumed alcohol. Ten were current users of prednisolone (> 5 mg per day), eight had rheumatoid arthritis, and none had diseases categorized under secondary causes of osteoporosis.
Age-dependent intervention thresholds
The age-dependent ITs of MOFR ranged from 2.7 to 18% and HFR ranged from 0.4 to 7.1% between 50 and 80 years (Table 1).
Fixed intervention thresholds
In the ROC analyses, AUCs (SE) for the MOFR and HFR were 0.77 (0.027) and 0.80 (0.024), respectively. ITs of MOFR and HFR at 9% and 3%, respectively, demonstrated the best sensitivity and specificity at the highest Youden index range. MOFR 9% was associated with sensitivity and specificity of 0.62 and 0.78, respectively. The corresponding figures for HFR were 0.63 and 0.81.
Hybrid intervention thresholds
The ROC curves constructed for those < 70 years had AUCs (SE) for MOFR and HFR of 0.81 (0.027) and 0.85 (0.024), respectively. The most appropriate fixed ITs found were MOFR 6% (0.67 sensitivity and 0.72 specificity) and HFR 2% (0.60 sensitivity and 0.87 specificity). For those ≥ 70 years, age-dependent ITs were calculated (Table 2).
Two-tier intervention thresholds
The fixed ITs found for those aged < 70 years were MOFR 6% (0.67 sensitivity and 0.72 specificity) and HFR 2% (0.60 sensitivity and 0.87 specificity). MOFR intervention threshold of 12% (sensitivity and specificity both 0.94) and HFR intervention threshold of 5% (sensitivity 0.95 and specificity 0.92) were the best cut points for those aged ≥ 70 years. The AUCs (SE) for MOFR and HFR of those aged ≥ 70 years were 0.98 (0.01) and 0.99 (0.007), respectively.
Validation of revised intervention thresholds
The mean (SD) age and BMI of the 356 postmenopausal women used for the validation were 63 (8.5) years and 24.9 (1.2) kg/m2, respectively. They all had undergone DXA and FRAX® to assess their fracture risk as a requirement of routine care. The comparison of fixed, hybrid, and two-tier ITs with the age-dependent ITs is given in Table 3.
The sensitivities of the four methods were assessed using a group of postmenopausal women who had undergone DXA within 1 month of a fragility fracture (n = 62). The age of these women ranged from 51 to 81 years and 52 of them had vertebral fracture, 4 had hip fracture, and 6 had fracture of distal forearm bones (all radiographically confirmed). All were fragility fractures and they gave no history of previous fracture or prolonged immobilization. According to the age-dependent ITs, 16 (26%) were above the threshold while on fixed ITs, this number increased to 30 (48%). Thirty-eight (61%) were found to be above the thresholds on the hybrid and two-tier ITs.
Discussion
In this study, we reassessed fixed ITs and tested new forms of ITs in order to detect postmenopausal women with a high fracture risk in Sri Lanka. While IT of HFR remained unchanged at 3%, the IT of MOFR changed from the previous value of 11% [8] to 9%. Age-dependent ITs remained unchanged, understandably, since no revisions to the Sri Lankan FRAX® model were made between the two analyses. Furthermore, hybrid and two-tier ITs were associated with a better discriminatory ability when compared with age-dependent and fixed ITs.
The previous ITs were estimated in a relatively smaller sample and a different method was used in deciding the cut point. The Youden index used in the current study is a well-accepted method in determining the cut point of the ROC curve [13], and the recent modification of the Youden index (partial Youden index) allows determining the best cut point while maintaining the sensitivity and specificity of practical interest [14]. In the previous analysis, the selection of cut points was arbitrary and based on the agreement between the two methods, i.e., the proportion of true positives and true negatives. Hence, we consider the new fixed ITs to be more scientifically robust than the previous values.
The hybrid and two-tier ITs showed higher sensitivity and specificity than fixed ITs. This is understandable since fracture risk is age dependent and any age-related adjustment is likely to improve the performance of ITs. Fixed ITs are easy to remember and are widely used. Fixed ITs are being used or have been proposed in the USA [17], Singapore [9], Sri Lanka [8], and China [7] while the UK [18], Australia [19], and Turkey [20] have proposed age-dependent ITs. Hybrid ITs were described by Chahtoura et al. for Lebanese [11] and also by NOGG in the UK [21] but we were unable to find two-tier ITs published previously. The hybrid ITs introduced by the NOGG include fixed ITs for those aged 70 years and above and age-dependent ITs for those below 70 years [21] while Chahtoura et al. used the opposite method [11]. We adopted the latter method which includes fixed ITs for those below 70 years and age-dependent ITs for those 70 years and above. This method is less likely to overtreat young women with lower fracture probabilities than the method described by the NOGG. Overtreatment of young women is a major concern as they, compared to older women, need to be treated for a longer period with medications linked with major adverse effects.
Regional and ethnic variations of ITs are well documented. Our age-dependent ITs are concordant with those observed among Chinese, Malay, and Indians in Singapore [9] but lower than those of Australians (HFR = 3%, 5%, and 7% for 50–69, 70–79, and ≥ 80 years, respectively) [19] and Japanese (ITs of MOFR 5% at 50 years and 20% at 80 years) [22]. The fixed ITs we observed were higher than those of Indians and Malays in Singapore [9] but similar to the Chinese in mainland China [7]. The hybrid ITs we observed at < 70 years were lower (IT of MOFR 6% vs 10%) than those reported by Chakhtoura et al. [11].
It is important that ITs selected are sufficiently valid before implementing in patient management. Although a trade-off between sensitivity and specificity is unavoidable, ITs chosen should have adequate sensitivity and specificity, providing sufficient discriminatory power. The fixed IT of 9.95% reported by Cheung et al. showed sensitivity of 62.3% and specificity of 73.5%. Despite a high NPV (> 90%), this cutoff value had a low PPV (10.3%) [7]. The National Osteoporosis Foundation-backed ITs in communities outside the USA are associated with low mean sensitivity but high specificity. In this analysis, with 20% MOFR cut point, a mean sensitivity of 10.25% and specificity of 97% and with 3% HFR cut point, a mean sensitivity of 45.7% and specificity of 84.7% were found [23]. We observed higher sensitivity, specificity, and predictive values especially for hybrid and two-tier ITs in our analysis.
The concept of FRAX® day-before-fracture has been used to assess the sensitivity of FRAX®-based ITs. This concept examines whether the patient presenting with a fragility fracture would have qualified for intervention, if she underwent FRAX® assessment the day before the fracture [15, 16]. We found that age-dependent ITs had a low sensitivity compared to the other three methods. In our analysis, age-dependent ITs were very high beyond 70 years and most patients were unable to reach them. If fixed ITs were used, nearly 50% patients could have been missed, and similar observations were made by Aubry-Rozier et al. [15] and Chen et al. [16] when Swiss and Chinese FRAX®-based ITs were used. Age-dependent ITs, compared to fixed ITs, tend to categorize fewer patients into the high-risk category [24]. The sensitivities of hybrid and two-tier ITs were similar and comparatively higher. We believe that clinicians will find two-tier ITs easy to remember particularly in busy clinical setups. The high sensitivity and simplicity of two-tier ITs will make it the most suitable IT to use in therapeutic decision making in Sri Lanka.
This study has a few limitations. There were only 62 women with recent fracture on whom validation could be performed. However, patients with hip or vertebral fracture are not referred for DXA evaluation soon after the fracture due to restricted mobility and pain. We could find only 62 women and they all had undergone DXA within 1 month of fracture. However, despite this limitation, our study has significant strengths including the relatively large numbers of women who were used to estimate ITs. The clinical details of all subjects included in this study were collected in the same manner using a pretested questionnaire. All DXA scans had been done on the same DXA machine and fracture risk was calculated in the same manner using the Sri Lankan FRAX® model. The two groups of women used for the development and validation of ITs came from the Southern Province and represented a wider geographical area ranging from rural to urban, all major ethnicities, and socio-economic strata. They, however, may not be the representative of the entire country.
In conclusion, we recommend replacing the existing FRAX®-based ITs in Sri Lanka with a more updated and suitable model. Although fixed ITs are easy to remember, the hybrid and two-tier ITs have a better discriminatory power. Two-tier ITs are easier to remember and would suit busy clinical setups.
References
Kanis JA, Harvey NC, Johansson H, Oden A, Leslie WD, McCloskey EV (2017) FRAX update. J Clin Densitom 20:360–367
Compston J, Cooper C, McCloskey E, Kanis JA (2012) FRAX updates 2012. Osteoporos Int 24:554–560
McCloskey EV, Harvey NC, Johansson H, Kanis JA (2016) FRAX updates 2016. Curr Opin Rheumatol 28:433–441
Lippuner K, Johansson H, Borgstrom F, Kanis JA, Rizzoli R (2012) Cost-effective intervention thresholds against osteoporotic fractures based on FRAX(R) in Switzerland. Osteoporos Int 23:2579–2589
Harvey NC, Kanis JA, Oden A, Burge RT, Mitlak BH, Johansson H, McCloskey EV (2015) FRAX and the effect of teriparatide on vertebral and non-vertebral fracture. Osteoporos Int 26:2677–2684
Paulden M, O’Mahony J, McCabe C (2017) Determinants of change in the cost-effectiveness threshold. Med Decis Mak 37:264–276
Cheung E, Cheung CL, Kung AW, Tan KC (2014) Possible FRAX-based intervention thresholds for a cohort of Chinese postmenopausal women. Osteoporos Int 25:1017–1023
Lekamwasam S (2013) Sri Lankan FRAX model and country-specific intervention thresholds. Arch Osteoporos 8:148
Chandran M, McCloskey EV, Thu WPP, Logan S, Hao Y, Tay D, Ang WC, Aung TKK, Choo KS, Ali A et al (2018) FRAX(R) based intervention thresholds for management of osteoporosis in Singaporean women. Arch Osteoporos 13:130
Wu CH, McCloskey EV, Lee JK, Itabashi A, Prince R, Yu W, Li-Yu J, Chionh SB, Zhao Y, Shin CS, Gunawan T, Tsai KS, Chieng PU, Changlai SP, Chan DC, Chen JF, Tanner SB, Hans DB, Kanis JA, Chang YF, Sun ZJ, Yang RS, Asia Pacific Panel of ISCD (2014) Consensus of official position of IOF/ISCD FRAX initiatives in Asia-Pacific region. J Clin Densitom 17:150–155
Chakhtoura M, Leslie WD, McClung M, Cheung AM, Fuleihan GE (2017) The FRAX-based Lebanese osteoporosis treatment guidelines: rationale for a hybrid model. Osteoporos Int 28:127–137
Kanis JA, Harvey NC, Cooper C, Johansson H, Oden A, McCloskey EV (2016) A systematic review of intervention thresholds based on FRAX : a report prepared for the National Osteoporosis Guideline Group and the International Osteoporosis Foundation. Arch Osteoporos 11:25
Youden WJ (1950) Index for rating diagnostic tests. Cancer 3:32–35
Li C, Chen J, Qin G (2018) Partial Youden index and its inferences. J Biopharm Stat 1–15
Aubry-Rozier B, Stoll D, Krieg MA, Lamy O, Hans D (2013) What was your fracture risk evaluated by FRAX(R) the day before your osteoporotic fracture? Clin Rheumatol 32:219–223
Chen XF, Li XL, Zhang H, Liu GJ (2014) Were you identified to be at high fracture risk by FRAX(R) before your osteoporotic fracture occurred? Clin Rheumatol 33:693–698
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, Lindsay R (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25:2359–2381
Compston J, Bowring C, Cooper A, Cooper C, Davies C, Francis R, Kanis JA, Marsh D, McCloskey EV, Reid DM, Selby P, National Osteoporosis Guideline Group (2013) Diagnosis and management of osteoporosis in postmenopausal women and older men in the UK: National Osteoporosis Guideline Group (NOGG) update 2013. Maturitas 75:392–396
Chen JS, Simpson JM, Blyth FM, March LM (2014) Managing osteoporosis with FRAX(R) in Australia: proposed new treatment thresholds from the 45&Up Study cohort. Bone 69:148–153
Tuzun S, Eskiyurt N, Akarirmak U, Saridogan M, Johansson H, McCloskey E, Kanis JA (2012) The impact of a FRAX-based intervention threshold in Turkey: the FRAX-TURK study. Arch Osteoporos 7:229–235
McCloskey E, Kanis JA, Johansson H, Harvey N, Oden A, Cooper A, Cooper C, Francis RM, Reid DM, Marsh D et al (2015) FRAX-based assessment and intervention thresholds--an exploration of thresholds in women aged 50 years and older in the UK. Osteoporos Int 26:2091–2099
Fujiwara S, Nakamura T, Orimo H, Hosoi T, Gorai I, Oden A, Johansson H, Kanis JA (2008) Development and application of a Japanese model of the WHO fracture risk assessment tool (FRAX). Osteoporos Int 19:429–435
Compston J, Cooper C, Jiang X, Gruner M, Tremollieres F, Pluskiewicz W, Sornay-Rendu E, Adamczyk P, Schnatz PF (2017) Diagnostic accuracy of FRAX in predicting the 10-year risk of osteoporotic fractures using the USA treatment thresholds: a systematic review and meta-analysis. Osteoporos Int 99:20–25
Kyriakos G, Vidal-Casariego A, Fernandez-Martinez MN, Blanco-Suarez MD, Ballesteros-Pomar MD, Cano-Rodriguez I (2015) Impact of the NOGG and NOF guidelines on the indication of bone mineral density in routine clinical practice. J Clin Densitom 18:533–538
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lekamwasam, S., Chandran, M. & Subasinghe, S. Revised FRAX®-based intervention thresholds for the management of osteoporosis among postmenopausal women in Sri Lanka. Arch Osteoporos 14, 33 (2019). https://doi.org/10.1007/s11657-019-0585-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-019-0585-2