Abstract
Summary
As osteoporosis relies largely on self-managed prevention and adherence to long-term treatment regimens, it is imperative that those at risk understand the disease that they are attempting to prevent. Ambiguity regarding osteoporosis and reluctance to take anti-osteoporosis medication (AOM) as well as calcium was noted in Australian post-menopausal women. This may lead to underestimating women’s own risk of osteoporosis and fracture.
Introduction
Fragility fractures caused by osteoporosis have been known to inflict significant personal and financial burden on individuals and society. As treatment of osteoporosis relies largely on self-managed prevention and adherence to long-term AOM regimens, it is imperative that women have a sound understanding of the disease that they are attempting to prevent. Much can also be gained from qualitatively exploring the level of osteoporosis knowledge particularly in post-menopausal women who are at greater risk of osteoporosis and fractures. This study thus aims to determine what post-menopausal Australian women know about osteoporosis and osteoporosis prevention.
Method
Six focus group sessions, using purposive sampling, were conducted with 23 female participants (mean age 68 years (range 62–83)). Women responded to a series of open-ended questions regarding their knowledge about osteoporosis. The audiotaped focus groups were transcribed verbatim and analysed using a thematic analysis framework.
Results
Three key themes were identified: ambiguity about the nature of osteoporosis, ambiguity about osteoporosis prevention and reluctance to take AOM and calcium.
Conclusion
Ambiguity associated with risk and prevention may provide women with a false sense of security that they are adequately acting to prevent the disease. Underestimation of their risk of osteoporosis and fracture as well as reluctance associated with AOM may be barriers to osteoporotic fracture prevention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The impact of osteoporosis is apparent primarily in the fragility fractures that occur as a result of the disease. The financial and personal burdens that osteoporosis-related fractures inflict on individuals and society have been previously described [1,2,3,4,5,6,7,8,9]. In the USA, it is estimated that 54 million Americans have low bone density or osteoporosis with US $19 billion spent on associated bone fractures [10]. By 2025, it is estimated that this cost will increase to US $25.3 billion [10]. By 2022, an estimated 6.2 million Australians over 50 years of age will have osteopenia or osteoporosis, with the total cost increasing to AU $3.84 billion associated with the disease from $2.75 billion in 2012 [11]. As having a first osteoporosis-related fracture increases the risk of future fractures, the burden described will likely be exacerbated in ageing populations worldwide.
Conditions such as osteoporosis rely largely on self-managed prevention so it is imperative that women have a sound understanding of the disease that they are attempting to prevent. Previous studies have found insufficient levels of knowledge about osteoporosis in various populations worldwide [12,13,14,15,16,17,18,19,20,21,22,23,24]. Those who have qualitatively studied the levels of osteoporosis knowledge in differing populations have found that although participants may have heard of the condition, limited knowledge was evident about the characteristics of osteoporosis (e.g. distinction between osteoporosis and other bone and joint conditions) [19, 21], the preventability of the disease [18, 22, 24] as well as measures needed to reduce their risk of osteoporosis and fracture [17, 20, 23]. Although these studies have shed much light on osteoporosis knowledge worldwide, past literature has not been focused on at-risk Australian populations, particularly post-menopausal women. Therefore, much can be gained from qualitatively exploring the level of osteoporosis knowledge particularly in post-menopausal Australian women who are at greater risk of osteoporosis and fractures. This study thus aimed to determine what post-menopausal Australian women know about osteoporosis and osteoporosis prevention.
Methods
Sample population
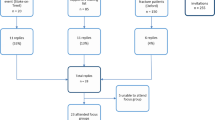
A purposeful sample of women (n = 127) taken from the Australian participant cohort from the Global Longitudinal Study of Osteoporosis in Women (GLOW study) [25] was invited to participate in one of six focus group sessions. Selection of possible focus group participants was informed by participant risk perception ratings to osteoporosis and fracture obtained in the quantitative phase of the GLOW Study. Participants with a discordant risk perception (those who perceived high osteoporosis risk but low fracture risk) in at least three questionnaires (n = 80), as well as those who perceived both low osteoporosis risk and low fracture risk (n = 25) or those who perceived both high osteoporosis risk and high fracture risk (n = 22), were identified and composed the focus group study population.
Those identified as prospective focus group participants were sent mailed invitations to participate in the focus groups. Once purposeful sampling was completed, consenting participants were contacted by telephone and booked at random into a focus group session. This allowed for a potentially diverse dialogue within each focus group.
Instrument and procedures
The development of the semi-structured focus group questions was informed by current literature at the time [26,27,28,29,30] and the quantitative findings of the GLOW study [31]. The questions were evaluated by a panel consisting of osteoporosis and/or qualitative researchers with at least 10 years’ experience. Another qualitative expert (MF) was consulted to discuss the flow and appropriateness of the question schedule. To test the instrument, a pilot focus group was conducted with four consenting participants of the GLOW study, enabling further refinement of the questions in an actual focus group setting.
The final list of 12 questions with accompanying prompts was divided into sections (Appendix 1). The first section consisted of two questions exploring participant understanding of osteoporosis and the value participants place on the disease. Section two contained three open-ended questions that asked participants to define the word “concern”. Participants were then asked how concerned they were about both osteoporosis and fractures in light of their definition. Section three comprised of two questions examining participant risk perception to both osteoporosis and fracture. Section four explored participant access to osteoporosis information. Section five examined participant perception of preventability of osteoporosis. Sections 6–8 explored anti-osteoporosis behaviours, with accompanying prompts. Demographic data for these participants were available from the GLOW study database.
The focus groups were conducted at a metropolitan tertiary hospital in Sydney, NSW, Australia, and consisted of between four and six participants [32, 33]. Each session was digitally recorded and moderated by one researcher (ABW). Another researcher experienced in focus groups acted as the scribe (MJC). Respondent validation [34] was achieved at the end of each session with the moderator verbally summarizing the main points that arose (Sections 9 and 10 of the interview schedule Appendix 1). Participants were then encouraged to confirm and if needed, further add to points summarized by the researcher. Debriefing meetings were held between the moderator (ABW) and the scribe (MJC) to evaluate each session. This also facilitated preliminary team-based analysis through the discussion of concepts that had arisen.
Data analysis
The collection, analysis and interpretation of data were an iterative process. Gibb’s framework [35] was used to guide analysis and began with the transcription of focus groups and an analysis processes including coding and categorizing patterns for theme development. Each focus group was transcribed verbatim by a single researcher (ABW) within 72 h of each session. The same transcriber then simultaneously rereads the corresponding transcripts while listening to an audio recording of each focus group session to check for accuracy and to allow the researcher to be immersed in the data [35]. All identifiable data was removed from transcripts, and each participant was assigned a code.
Coding was performed independently by two researchers (ABW and MJC) with consensus on analysis and interpretation achieved. Both researchers convened and conducted inter-rater checks to compare and discuss their independent findings on the manual coding of all transcripts. Coded transcripts were entered into a computerized data management program (NVivo 10™) where further refinement of codes and thematic analysis continued [35]. As a result, developed themes were agreed upon by the two independent researchers.
Results
Participant demographics
The characteristics of participants are shown in Table 1. Twenty-three post-menopausal women took part in one of six focus groups. The mean age of participants was 67 years. Eighty-three percent (13/23) completed at least a higher school certificate (12 years of education) with all participants having private health cover. Twenty-six percent (6/23) reported being told previously that they had osteoporosis by a doctor or health care provider. Thirteen out of 23 (57%) women had reported being told that they had osteopenia and were at risk of osteoporosis. Eighteen of the 23 participants were currently on anti-osteoporosis medication (AOM) (including bisphosphonates, hormone replacement therapy, and calcium and vitamin D).
Fourteen out of the 23 participants (61%) had a discordant risk perception (those who perceived high osteoporosis risk but low fracture risk in at least three questionnaires). The duration of the focus groups ranged from 48 min to 1 h and 52 min in length, with the average time of 1 h and 24 min.
Osteoporosis risk factors
Eight of the 23 women (35%) reported having a fracture after 45 years of age. Seven participants (30%) reported a maternal osteoporosis diagnosis while 2/23 (9%) reported previous maternal hip fracture. All were non-smokers and 12/23 (52%) reported having greater than or equal to 7 alcoholic drinks per week. Ten women (43%) in the study population were either underweight (BMI < 18.5) or overweight/obese (BMI > 25.0).
Thematic findings: Ambiguity and the nature of osteoporosis
Three key themes were developed from the analysis and were related to ambiguity and the nature of osteoporosis: ambiguity about the nature of osteoporosis, ambiguity about osteoporosis prevention and reluctance to take anti-osteoporosis medications.
Ambiguity about the nature of osteoporosis
In this study, women voiced ambiguity regarding the preventability of osteoporosis. Although most women had heard of osteoporosis and some thought it to be a preventable disease (7/23), half of the sample (12/23) were either uncertain or doubted the preventability of the condition. The uncertainty about the nature of osteoporosis was evident in all women in the sample regardless of whether they were currently on treatment or if they sustained a previous fracture after the age of 45 years.
The belief that genetics played a greater role in one’s propensity to develop the condition was held particularly by participants who were touched by the disease through family history. Such participants would give examples of their grandmother, mother or aunt suffering from the condition:
#FG3JM “I didn’t think it was preventable as such…I don’t think you can prevent it because that’s your genes.”
Others believed that developing osteoporosis was an inevitable part of the ageing process that affects people as they age:
#FG1ST “It’s always been a thing as you get older, isn’t it? Most people know that as you get older your bones become brittle.”
and
#FG6HC “I think that…nothing is necessarily going to stop you from getting osteopenia or osteoporosis…I mean if you’re gonna get it, you’re gonna get it.”
These beliefs suggest that some women perceived a lack of control over developing the disease. This perception is exemplified with women exclaiming that they “…can’t stop what’s going to happen…” (#FG6CF) in relation to osteoporosis.
Ambiguity about osteoporosis prevention methods
Although most women reported at least one prevention strategy against osteoporosis, there was a high level of uncertainty regarding preventive methods to decrease one’s risk of developing the disease. This uncertainty was marked in most women in the study, irrespective of current treatment status or previous fracture history.
In the current sample of post-menopausal women, 12 (52%) voiced uncertainty regarding dietary calcium, vitamin D and supplementation. While women were able to name “milk”, “yoghurt” and “cheese” as sources of calcium, many were unaware of other sources of calcium apart from dairy products:
#FG5BB “I don’t really know other than the milk products where you can get calcium…we eat quite a lot of vegetables so if they come from vegetables, I guess we do.”
Women also expressed uncertainty regarding the amount of calcium and vitamin D they needed each day or questioned whether they currently were getting the correct amounts of both. When probed further, women commonly asked the question back to the moderator: “So how much calcium and vitamin D do you need?”
A high level of ambiguity was also found in women who were taking supplementation. During the focus groups, many women were unaware of whether supplementation use had an effect on increasing their calcium and vitamin D levels. In this study, ambiguity in women’s understanding of supplementation has been shown to affect preventive behaviour. To illustrate, one woman explained how her doctor placed her on a vitamin D tablet only to cease supplementation after 1 year for no apparent reason:
“My doctor [put me] on a vitamin D tablet. But I don’t know what’s happening…I’m not taking them anymore.” (#FG1MCE)
When probing further as to the reason behind the cessation of the tablet, the woman was asked whether she had a test to determine an improvement in her vitamin D levels. In response, she replied that she had not taken any tests. She also noted that she had not increased her sun exposure to compensate for ceasing supplementation. As illustrated with this woman, uncertainty about the effectiveness of supplementation may influence higher levels of non-adherence to supplementation.
Women also expressed confusion regarding exercises needed for bone health. Although women placed value on performing weight-bearing exercises to decrease their risk of osteoporosis and fracture, a level of uncertainty on the exact exercises required was evident. This was particularly noted when swimming and aqua aerobics were mentioned by five (22%) women as forms of weight-bearing exercises to prevent osteoporosis:
#FG1MP “Because of the swimming…because it’s the weight bearing exercise.”
and
#FG6CH “I’ve just started aqua-aerobics…I’m going to continue with that because I can see it’s another way of doing weight bearing exercise. You know the resistance of the water...”
Reluctance to take anti-osteoporosis medications
Several women also expressed their reluctance towards taking AOM (including bisphosphonates and hormone replacement therapy (HRT)) and in some cases, even calcium tablets. This reluctance was expressed by women irrespective of whether or not they were at high risk of future fracture (had low bone density and/or previous fracture after the age of 45 years). Instead, there was a general preference to “...just continue on as I am.” (#FG4RR) in regard to their current forms of osteoporosis prevention in the absence of treatment. In this study, women’s reluctance towards AOM was mostly attributed to the fear of side effects associated with the use of certain medications. Symptoms which were most commonly mentioned during the focus group sessions included osteonecrosis of the jaw associated with the use of bisphosphonates such as Fosamax:
#FG4AD “I took [Fosamax] for about 6 years and then I decided that that was enough and I didn’t like it. I had to have a tooth extracted and the dentist wouldn’t do it because I hadn’t been off it for 10 years…so I had to go find a surgeon who would do it…the local dentist wouldn’t do it because it can actually deteriorate the bone and as soon as I found that out, mine went in the garbage bin.”
Others alluded to the heightened breast cancer risk associated with HRT:
#FG6DK “And I do worry a bit with the questions about HRT…and I also was on [HRT] until a good friend got breast cancer. I went straight off it and put up with the hot flushes.”
And, heart disease links to calcium:
#FG6GT “I’m very much reluctant to take any medications at all even the calcium tablets worry me now that there’s been links to heart disease.”
A sense of reluctance in adhering to or restarting treatment of certain AOM, such as Fosamax, was also reported in two women who were at higher risk of fracture (i.e. had low bone density and a previous fracture after the age of 45 years). The reluctance towards certain AOM in high-risk women still persisted despite experiencing improvements in their BMD as a result of taking AOM in the past. In these women, the risks of side effects played a greater role in their decision to cease treatment over the benefit of improved bone health and reduced risk of fractures:
#FB3JM “I was put on Fosamax and mine definitely improved noticeably and after a while I got a bit worried about taking drugs and Fosamax got a bit of bad press and I went off it.”
Discussion
This qualitative study aimed to determine what post-menopausal Australian women know about osteoporosis and osteoporosis prevention. In this study, there was a certain amount of ambiguity expressed regarding appropriate bone health exercises. Similar to the recent findings by Wright et al. [36], some women in the current study mentioned certain weight-bearing exercises and walking for bone health. However, non-weight-bearing activities such as swimming and aqua aerobics were also mentioned by numerous women as examples of exercises promoting bone health. These results are consistent with the past findings from Baheiraei et al. who reported how the majority of Iranian-Australian men and women aged 35–70 years considered swimming an effective form of exercise to reduce the risk of osteoporosis [17]. A quantitative study conducted by Gerend et al. [37] also found that a proportion of women aged 40–86 years perceived themselves to be reducing their osteoporosis risk through swimming [37], while Noel et al. reported that although participants agreed that exercise was needed for bone health, there was uncertainty about how or why this was beneficial [19]. In addition, women in the current study were unable to identify other more impactful exercises such as jogging, jumping, skipping, and dancing which have been found to be more beneficial to bone health compared with walking [38,39,40,41,42]. This ambiguity regarding exercises may inadvertently give women a false sense of security that they are doing exercises to increase bone health when in fact, these types of exercises have little weight-bearing benefits.
This study also highlighted a reluctance associated with taking certain AOM such as bisphosphonates and hormone therapy. This reluctance was marked in women irrespective of whether or not they were at high risk of future fracture (had low bone density and/or previous fracture after the age of 45 years). Women in this study placed great value on the presence of side effects when assessing their willingness to adhere to these types of medications. Even in those with a higher risk to future fracture, there was still hesitation to adhere to or restart treatment despite marked improvements to their BMD results. The current study found the anticipation of adverse effects of osteoporosis treatment to be a significant barrier to AOM adherence and is in line with previous quantitative and qualitative literature [18, 21, 23, 43,44,45,46]. A recent qualitative study by Merle et al. [18] found that French men and women aged 50–85 years were also suspicious in taking pharmacological treatments for osteoporosis due to their associated side effects [18]. Similarly, concerns over AOM-related side effects were also found to affect treatment adherence in older Americans [21, 43] and even in female English sufferers of osteoporosis and osteopenia. [23]. When considering the potential harmful side effects associated with treatment, women in this study had a stronger preference towards continuing with other preventive methods for osteoporosis over AOM. The actual risk of AOM-related side effects such as osteonecrosis of the jaw, however, has been found to be quite low [47]. It has been previously estimated that the risk of osteonecrosis of the jaw associated with bisphosphonate treatment was between one in 10,000 and less than one in 100,000 patient-treatment years. The risk in cancer patients was, however, found to be higher (1–10 per 100 patients) due to the use of increased doses of bisphosphonates as an adjunctive therapy to cancer treatment. Reluctance in taking AOM has detrimental implications on fracture risk prevention, particularly when women are not confident in effectively performing other forms of osteo-protective behaviours. Community knowledge of the benefits of medication for preventing subsequent fractures is required to counterbalance the fears of potential rare side effects. This is particularly important as community perceptions of the safety of AOM (which are often influenced by adverse media) have previously been shown to potentially impact treatment rates [48,49,50] and the incidence of fracture and fracture-related deaths [37, 49]. In addition, community perception may also be influenced by consultations with dentists who may advise women to cease potentially beneficial bone treatment prior to dental procedures [49].
In this current study, post-menopausal women also expressed ambiguity regarding vitamin and mineral supplementation to prevent osteoporosis. This included the recommended daily calcium intake, sources of calcium besides dairy products and the amount of beneficial sunlight exposure needed to provide bone health benefits. This uncertainty is in line with previous reports from Australia, Canada, Israel and the USA [17, 20, 43, 51, 52]. In the study by Baheiraei et al., Iranian-Australia men and women failed to correctly identify calcium-rich foods and were unaware of the recommended amount of calcium intake. This is despite the majority of participants recognizing the importance of calcium intake to bone health [17]. Another study of Canadian participants aged 47–80 years by Sale and colleagues also reported a level of uncertainty in the majority of participants regarding recommended supplement dosage and duration of treatment [20]. Uncertainty about dietary sources of vitamin D was also noted by Noel et al. [19] in Caribbean Hispanic/Latino adults over 50 years [19]. Uncertainty about vitamin and mineral supplementation may lead post-menopausal women to have suboptimal amounts of calcium and vitamin D required for bone health. In addition, insufficient knowledge of dietary calcium sources apart from dairy products can result in women limiting the range of food they consume to increase their dietary calcium. This can be particularly detrimental to women who have an intolerance or aversion to dairy products and are also unable or unwilling to take supplementation. As demonstrated in this study and supported in the literature [20, 43, 51], uncertainty about the effectiveness of supplementation may also cause higher levels of non-adherence to supplementation.
This study has limitations which should be considered. Sample bias may be present as the women in this study were taken from a larger study cohort of Australian women from the GLOW study. Participants were predominantly from a geographic region that may be considered to be within a higher socio-economic background. The majority of the women in the study reported to have attained at least a higher school certificate (12 years of study) as well as having private health insurance cover. Eighty-two percent of women in this study attained at least a high school certificate contrasted to the 65% of those attaining a similar level of education in the greater Sydney area [53, 54]. All the women in this study had private health insurance, and this is also contrasted with the 52% private health insurance coverage of women aged ≥ 55 years in the Australian population [55, 56]. In spite of this, the findings of this study illustrated the presence of uncertainty regarding various aspects of osteoporosis even in women from relatively privileged well-educated backgrounds in an area well-serviced by medical services. Additional sample bias may have also been present due to the low response rate (18%) with 23 individuals agreeing to participate in the focus groups out of 127 invited individuals.
This study has demonstrated how ambiguity can influence self-management and osteoporotic prevention behaviours in post-menopausal Australian women. Yet, ambiguity may provide post-menopausal women with a false sense of security that they are adequately acting to prevent osteoporotic disease. Further, within the community, there is a reluctance associated with AOM which may lead to an increased risk of osteoporosis and future fracture particularly in highly susceptible individuals. This study has illustrated the need for future patient/consumer education to emphasize effective osteo-protective behaviours regarding calcium, vitamin D and appropriate bone health exercises. Such emphasis on alternate and effective methods of disease and fracture prevention would prove especially vital for women reluctant to take pharmacotherapy for osteoporotic re-fracture prevention.
References
Abimanyi-Ochom J, Watts JJ, Borgström F, Nicholson GC, Shore-Lorenti C, Stuart AL, Zhang Y, Iuliano S, Seeman E, Prince R, March L, Cross M, Winzenberg T, Laslett LL, Duque G, Ebeling PR, Sanders KM (2015) Changes in quality of life associated with fragility fractures: Australian arm of the International Cost and Utility Related to Osteoporotic Fractures Study (AusICUROS). Osteoporos Int 26(6):1781–1790
Adachi J, et al (2010) Impact of prevalent fractures on quality of life: baseline results from the global longitudinal study of osteoporosis in women. Mayo Clinic proceedings Mayo Clinic. 85: p. 806–13
Bertram M et al (2011) Review of the long-term disability associated with hip fractures. Inj Prev 17:365–370
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res 22(3):465–475
Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA (1999) Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet 353(9156):878–882
Kado DM, Duong T, Stone KL, Ensrud KE, Nevitt MC, Greendale GA, Cummings SR (2003) Incident vertebral fractures and mortality in older women: a prospective study. Osteoporos Int 14(7):589–594
Pasco JA, Sanders KM, Hoekstra FM, Henry MJ, Nicholson GC, Kotowicz MA (2005) The human cost of fracture. Osteoporos Int 16(12):2046–2052
Rostom S et al (2012) The prevalence of vertebral fractures and health-related quality of life in postmenopausal women. Rheumatol Int 32(4):971–980
Svedbom A et al (2013) Osteoporosis in the European Union: a compendium of country-specific reports. Arch Osteoporos 8:137
National Osteoporosis Foundation. National Osteoporosis Foundation: What is osteoporosis and what causes it? [Accessed: February 2019]. Available at https://www.nof.org/patients/what-isosteoporosis/
Osteoporosis Australia. Osteoporosis costing all Australians. A new burden of disease analysis – 2012 to 2022. [Accessed March 2019] Available at: www.osteoporosis.org.au
Chan CY et al (2018) A review of knowledge, belief and practice regarding osteoporosis among adolescents and young adults. Int J Environ Res Public Health 15(8):12
Nguyen NV, Dinh TA, Ngo QV, Tran VD, Breitkopf CR (2015) Awareness and knowledge of osteoporosis in Vietnamese women. Asia Pac J Public Health 27(2):NP95–N105
Levinson MR, Leeuwrik T, Oldroyd JC, Staples M (2012) A cohort study of osteoporosis health knowledge and medication use in older adults with minimal trauma fracture. Arch Osteoporos 7:87–92
Wong CP, Lok MK, Wun YT, Pang SM (2014) Chinese men’s knowledge and risk factors of osteoporosis: compared with women’s. Am J Mens Health 8(2):159–166
Babatunde OT, Marquez S, Taylor A (2017) Osteoporosis knowledge and health beliefs among men in midlife years. J Nutr Educ Behav 49(9):759–763
Baheiraei A, Ritchie JE, Eisman JA, Nguyen TV (2006) Exploring factors influencing osteoporosis prevention and control: a qualitative study of Iranian men and women in Australia. Maturitas 54(2):127–134
Merle B, Dupraz C, Haesebaert J, Barraud L, Aussedat M, Motteau C, Simon V, Schott AM, Flori M (2019) Osteoporosis prevention: where are the barriers to improvement in a French general population? A qualitative study. Osteoporos Int 30(1):177–185
Noel SE, Arevalo SP, Mena NZ, Mangano K, Velez M, Dawson-Hughes B, Tucker KL (2019) Knowledge, attitudes, beliefs, and health behaviors of bone health among Caribbean Hispanic/Latino adults. Arch Osteoporos 14(1):14
Sale JE, Beaton DE, Sujic R, Bogoch ER (2010) ‘If it was osteoporosis, I would have really hurt myself.’ Ambiguity about osteoporosis and osteoporosis care despite a screening programme to educate fragility fracture patients. J Eval Clin Pract 16(3):590–596
Burgener M, Arnold M, Katz JN, Polinski JM, Cabral D, Avorn J, Solomon DH (2005) Older adults’ knowledge and beliefs about osteoporosis: results of semistructured interviews used for the development of educational materials. J Rheumatol 32(4):673–677
Rothmann MJ et al (2014) Women’s perspectives and experiences on screening for osteoporosis (Risk-stratified Osteoporosis Strategy Evaluation, ROSE). Arch Osteoporos 9(1):192
Besser SJ, Anderson JE, Weinman J (2012) How do osteoporosis patients perceive their illness and treatment? Implications for clinical practice. Arch Osteoporos 7(1):115–124
Reventlow S, Bang H (2006) Brittle bones: ageing or threat of disease exploring women’s cultural models of osteoporosis. Scand J Public Health 34(3):320–326
Barcenilla-Wong AL, Chen JS, March LM (2013) Concern and risk perception of osteoporosis and fracture among post-menopausal Australian women: results from the Global Longitudinal Study of Osteoporosis in Women (GLOW) cohort. Arch Osteoporos 8(1):155
Williams B, Cullen L, Barlow JH (2002) “I never realised how little I knew!”: a pilot study of osteoporosis knowledge, beliefs, and behaviours. Health Care Women Int 23(4):344–350
Siris ES et al (2011) Failure to perceive increased risk of fracture in women 55 years and older: the Global Longitudinal Study of Osteoporosis in Women (GLOW). Osteoporo Int 22(1):27–35
Hvas L, Reventlow S, Jensen HL, Malterud K (2005) Awareness of risk of osteoporosis may cause uncertainty and worry in menopausal women. Scand J Public Health 33(3):203–207
Chang S-F (2006) A cross-sectional survey of calcium intake in relation to knowledge of osteoporosis and beliefs in young women. Int J Nurs Pract 12:21–27
Estok PJ, Sedlak CA, Doheny MO, Hall R (2007) Structural model for osteoporosis preventing behavior in postmenopausal women. Nurs Res 56(3):148–158
Barcenilla-Wong A, Chen JS, March L (2014) Concern and risk perception: effects on osteoprotective behaviour. J Osteoporos. https://doi.org/10.1155/2014/142546
Lichtman, M. (2010) Qualitative research in education: a user’s guide. SAGE Publications
Morgan DL (1997) Focus groups as qualitative research. SAGE Publications
Creswell JWaVPC (2011) Designing and conducting mixed methods research second edition. SAGE Publications, Thousand Oaks
Gibbs GR (2007) Analyzing qualitative data. SAGE Publications, Thousand Oaks
Wright NC, Melton ME, Sohail M, Herbey I, Davies S, Levitan EB, Saag KG, Ivankova NV (2019) Race plays a role in the knowledge, attitudes, and beliefs of women with osteoporosis. J Racial Ethn Health Disparities 6(4):707–718
Gerend MA, Erchull MJ, Aiken LS, Maner JK (2006) Reasons and risk: factors underlying women’s perceptions of susceptibility to osteoporosis. Maturitas 55(3):227–237
Heinonen A, Kannus P, Sievänen H, Oja P, Pasanen M, Rinne M, Uusi-Rasi K, Vuori I (1996) Randomised controlled trial of effect of high-impact exercise on selected risk factors for osteoporotic fractures. Lancet 348(9038):1343–1347
Hinton PS, Nigh P, Thyfault J (2015) Effectiveness of resistance training or jumping-exercise to increase bone mineral density in men with low bone mass: a 12-month randomized, clinical trial. Bone 79:203–212
Kemmler W, Engelke K, von Stengel S, Weineck J, Lauber D, Kalender WA (2007) Long-term four-year exercise has a positive effect on menopausal risk factors: the Erlangen Fitness Osteoporosis Prevention Study. J Strength Cond Res 21(1):232–239
Kemmler W, von Stengel S, Weineck J, Lauber D, Kalender W, Engelke K (2005) Exercise effects on menopausal risk factors of early postmenopausal women: 3-yr Erlangen fitness osteoporosis prevention study results. Med Sci Sports Exerc 37(2):194–203
Vainionpää A et al (2006) Intensity of exercise is associated with bone density change in premenopausal women. Osteoporo Int 17(3):455–463
Iversen MD, Vora RR, Servi A, Solomon DH (2011) Factors affecting adherence to osteoporosis medications: a focus group approach examining viewpoints of patients and providers. J Geriatr Phys Ther 34(2):72–81
Papaioannou A, Kennedy CC, Dolovich L, Lau E, Adachi JD (2007) Patient adherence to osteoporosis medications. Drugs Aging 24(1):37–55
Rossini M, Bianchi G, di Munno O, Giannini S, Minisola S, Sinigaglia L, Adami S, Treatment of Osteoporosis in clinical Practice (TOP) Study Group (2006) Determinants of adherence to osteoporosis treatment in clinical practice. Osteoporos Int 17(6):914–921
Weiss TW, Gold DT, Silverman SL, McHorney C (2006) An evaluation of patient preferences for osteoporosis medication attributes: results from the PREFER-US study. Curr Med Res Opin 22(5):949–960
Khosla S, Burr D, Cauley J, Dempster DW, Ebeling PR, Felsenberg D, Gagel RF, Gilsanz V, Guise T, Koka S, McCauley L, McGowan J, McKee M, Mohla S, Pendrys DG, Raisz LG, Ruggiero SL, Shafer DM, Shum L, Silverman SL, van Poznak C, Watts N, Woo SB, Shane E, American Society for Bone and Mineral Research (2007) Bisphosphonate-associated osteonecrosis of the jaw: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 22(10):1479–1491
Peeters G, Tett SE, Duncan EL, Mishra GD, Dobson AJ (2014) Osteoporosis medication dispensing for older Australian women from 2002 to 2010: influences of publications, guidelines, marketing activities and policy. Pharmacoepidemiol Drug Saf 23(12):1303–1311
Sambrook PN, Chen JS, Simpson JM, March LM (2010) Impact of adverse news media on prescriptions for osteoporosis: effect on fractures and mortality. Med J Aust 193(3):154–156
Cipriani C, Pepe J, Minisola S, Lewiecki EM (2018) Adverse effects of media reports on the treatment of osteoporosis. J Endocrinol Investig 41(12):1359–1364
Ribeiro V, Blakeley J, Laryea M (2000) Women’s knowledge and practices regarding the prevention and treatment of osteoporosis. Health Care Women Int 21(4):347–353
Werner P (2005) Knowledge about osteoporosis: assessment, correlates and outcomes. Osteoporo Int 16(2):115–127
Australian Bureau of Statistics. Census of Population and Housing. Greater Sydney Community Profile. Table B16—Highest Year of School Completed by Age by Sex, Australian Bureau of Statistics, Canberra, Australia, 2011. http://www.abs.gov.au/. Accessed 08 March 2019
Australian Bureau of Statistics, Census of Population and Housing. Greater Sydney Community Profile. B40 Non-School Qualification: Level of Education(a) by Age by Sex (1 of 2), Australian Bureau of Statistics, Canberra, Australia, 2011. http://www.abs.gov.au/. Accessed 08 March 2019
Australian Bureau of Statistics, Australian Demographic Statistics, March 2014. ‘Table 7: Estimated resident population by age and sex—at 30 June 2012’, Data Cube: Excel Spreadsheet. Australian Bureau of Statistics, Canberra, Australia, 2014. http://www.abs.gov.au/. Accessed 08 March 2019
Private Health Insurance Administration Council (2013) Quarterly Statistics June 2013. Private Health Insurance Administration Council, Canberra
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The GLOW study was funded by The Alliance for Better Bone Health (Procter & Gamble Pharmaceuticals and Sanofi-Aventis). Annica Barcenilla-Wong received funding for preparation of this manuscript from the Institute of Bone and Joint Research Rheumatology Research fund but they had no role in the development of this manuscript. Ethical approval was obtained from the local Human Research Ethics Committee, and informed consent was obtained from all participants of the study.
Conflicts of interest
Marita Cross, Margaret Fry and Lyn March declare no conflicts of interest. Annica Barcenilla-Wong was in receipt of support for preparation of this manuscript from the Institute of Bone and Joint Research Rheumatology Research fund.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Barcenilla-Wong, A.L., Cross, M., Fry, M. et al. Ambiguity hindering self-management and prevention of osteoporosis in post-menopausal women. Arch Osteoporos 15, 73 (2020). https://doi.org/10.1007/s11657-020-0683-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-020-0683-1