Abstract
Summary
We conducted a qualitative study with French men and women in order to provide insight into individuals’ experiences, behaviors, and perceptions about osteoporosis (OP) and OP care. The data showed that both sexes, but especially men, were unfamiliar with OP, did not always feel concerned, and mistrusted pharmacological treatments.
Introduction
To engage actively in osteoporosis (OP) prevention, people need to have basic knowledge about the disease. The aim of this qualitative study was to explore knowledge and representations of OP care and prevention among both men and women.
Methods
Focus groups were conducted in the Rhône-Alpes Region, France, with women aged 50–85 years and men aged 60–85 years, with or without a history of fragility fracture and/or an OP diagnosis (respectively referred to as “aware” or “unaware”). A total of 45 women (23 “aware” and 22 “unaware” in 5 and 4 focus groups, respectively) and 53 men (19 “aware” and 34 “unaware” in 3 and 4 focus groups, respectively) were included. A thematic analysis of transcripts was performed to explore knowledge and representations about OP, risk factors, prevention, and treatment.
Results
The data showed that both sexes, but especially men, had limited knowledge of OP and considered it as a natural aging process not related to fragility fractures. They generally did not feel concerned by OP and no important difference was observed between “aware” and “unaware” patients. Women expressed their fear of the disease, associated with aging and the end of life, while men considered it to be a women’s disease only. Both sexes were aware of OP risk factors, but were suspicious towards treatments because of the associated side effects.
Conclusion
Understanding people’s representation of OP might help to provide patients with relevant information in order to optimize their preventive behavior and decrease the burden of the disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Osteoporosis (OP) is a skeletal disease characterized by low bone density and alterations in bone micro-architecture, leading to increased bone fragility concerning predominantly postmenopausal women but also men [1]. OP is responsible for fragility fractures associated with morbidity, loss of independence, and mortality. Although two thirds of the fractures occurred in women, half of all deaths concerned men [2]. With the aging of the population, OP is becoming a major public health issue worldwide with increasing human and financial costs. In France, reports estimated that in 2010, nearly 25% of women and 7% of men over 50 years of age were concerned by OP, with 4300 deaths directly attributed to OP fractures [3, 4]. The financial cost of OP for pharmacological prevention and fracture care is significant and has been estimated in 2010 at 3.5 billion euros and 1.3 billion euros for French women and men, respectively, mostly for hip fractures [2, 4, 5].
Various national and international guidelines have been developed to assess bone status and improve OP management and fracture prevention in an evidence-based and cost-effective manner [6, 7]. New models of care have proved their efficacy for primary but also secondary prevention with fracture liaison services (FLS) developed to improve OP management and prevent the fracture cascade [8,9,10].
However, these recommendations are not implemented in routine practice. Thus, OP is under-diagnosed and under-treated despite the availability of effective treatments: less than 20% of patients experiencing a fragility fracture worldwide received appropriate OP management despite the high risk of fracture recurrence [11, 12]. The situation is worse for men than for women, as only 4.5% of the former being treated for OP after a fragility fracture (versus 27% of women) [13].
This care gap may be explained by the asymptomatic nature of the disease and by barriers related to both the healthcare system and the patients [6, 7]. Studies show that patients often do not know a great deal about OP and have difficulties in perceiving its existence in the absence of symptoms. The question of OP as natural bone deterioration rather than a disease has been raised [14,15,16,17,18]. A greater understanding of the reasons for the failures in reducing the OP care gap is crucial in order to develop more effective prevention and information strategies. However, qualitative research on healthcare providers’ and patients’ perceptions, personal experiences, and behaviors regarding OP is currently lacking. The first step to designing effective programs for OP prevention and care is to obtain an in-depth understanding of patients’ representations and concerns about the disease.
We therefore aimed to explore the knowledge and representations of French men and women regarding OP and its prevention and their ideas for improvement. This study is part of a program aiming to acquire a better understanding of the reasons impeding the implementation of current OP guidelines in France in order to define effective strategies to improve OP management and lower its social and human cost.
Methods
A descriptive qualitative study was implemented using focus group interviews to explore representations of OP in a French population. The focus group methodology uses interactions between participants to explore and stimulate different points of view through guided open discussion [19].
Participants
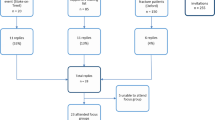
Four types of participants were recruited to attend four types of focus groups: women aged 50 to 85 years and men aged 60 to 85 years, a priori “aware” about OP (referred to as Wa and Ma, respectively), or a priori “unaware” about OP (referred to as Wun and Mun, respectively). To be “aware” was defined as having a personal history of fragility fracture, an OP diagnosis, a pharmacological treatment, and/or a medical follow-up concerning OP. Patients who were “unaware” did not have a personal history of fragility fracture, an OP diagnosis, a treatment, and/or a medical follow-up for OP. Unaware patients were recruited through the members of a French health insurance company Association de Prévoyance Interprofessionnelle des Cadres et Ingénieurs de la région Lyonnaise (APICIL) in Lyon and its vicinity. Aware patients were recruited among the participants of two studies conducted by our group (the Prevost study for women [20] and the Strambo study for men [21]) and through APICIL. Patients were invited to participate by a letter explaining the study objectives, the focus-group process, and the confidentiality of the data collected. Sample size was determined by similar qualitative previous studies on osteoporosis prevention [15, 19]. The study was approved by the local ethics committee (Institutional Review Board: IORG0007394. Ref: IRBN092014/CHUSTE).
Procedures and data collection
Focus groups were conducted by a moderator (general practitioner (GP), trained for focus-group-based research) and audio-recorded. Two assistants independent from the research team (residents in general practice trained for focus-group-based research) noted the non-verbal interactions. A semi-structured interview guide covering five topics (disease representation, risk factors, consequences, prevention, patient expectations) was developed by the authors, based on the existing literature (Table 1). It was enriched and validated by the study steering group, composed of GPs, public health researchers, and rheumatologists and through pilot interviews. The guide was the thread of the interviews and allowed debate and interactions between participants around different aspects of the main theme. The frame allowed both to make sure that all the preset themes were addressed and to prompt participants in case the answer was not developed enough. Four types of focus group were used, composed of either aware or unaware men, or aware or unaware women.
Before the beginning of the discussion, participants completed a short sociodemographic questionnaire. Each discussion started with a word association task by the question: “If I say osteoporosis, what words come to mind.” At the end of each focus group, participants were free to ask questions to the moderator and all patients received an information booklet on OP and fragility fractures. Groups were performed until data saturation but a minimum of three focus groups were planned for each type of participant to have enough data to analyze similarities and differences between the different types of groups. Saturation was raised when no new information emerged during focus groups.
Data analysis
The audio recordings of interviews were comprehensively transcribed and linked with field notes of the assistants. A thematic analysis of the transcribed corpus of interviews was performed by the assistants with Nvivo 10 software (NVivo QSR International). Participants’ responses were coded and categorized into themes and subthemes, based on the similarity of content in each focus group and across the different groups; the analysis was performed both at the individual and group level and allowed the identification of the opinions of the majority of the participants and selection of the most representative quotes [22]. Each idea was coded in order to consolidate occurrences. The interviews and transcription were conducted in French. The quotes chosen to be mentioned in this paper were translated into English and reviewed by a native English scientific and medical writer for consistency.
Results
The participants
A total of 45 women and 53 men were included in focus groups, each with 4 to 8 participants: 23 “aware” women in 5 focus groups and 22 “unaware” women in 4 focus groups and 19 “aware” men in 3 groups and 34 “unaware” men in 4 groups (Table 2). Men have been recruited older than women to reflect the fact that the age-associated bone loss and osteoporosis starts later in men than in women. Participation was effective only after the written consent was signed. Three to five groups were necessary to obtain saturation in each population.
General representations of OP
Little is known about OP
Each focus group started with a word association task by the question: “If I say osteoporosis, what words come to mind?” OP was defined as bone fragility by most of the participants; women generally associated it with aging and fractures secondary to mild trauma, whereas men, particularly the “unaware,” considered it was a women’s disease for which they had never expressed any concern.
Wun3A: I suppose that the bone is eroding away like a stone at the seaside.
Wun2C: the bones break… spontaneously, I believe .
MunD3: … a hole in the bone.
The fracture was considered as the consequence of OP by both aware and unaware women and by some men. But many of the men wondered if OP could be responsible for fractures.
Wun1A: OP often leads to hip fracture.
However, most participants had limited and sometimes inaccurate knowledge of OP; they frequently confused it or associated it with other pathologies, particularly osteoarticular diseases such as arthritis or osteoarthritis, and associated OP with pain.
Wun2F: …It’s the joints wearing away… so OP…. you get it mostly in the joints.
MaES2: … I wonder whether OP can lead to bone cancer?
MunA4: I don’t believe there’s any link between height loss and OP. In OP, it breaks, and that’s that.
Considering the diagnosis, bone densitometry (BMD) was mentioned in all focus groups composed of women but only by few men and with difficulties. Generally, participants were not certain about the objective of the test and the meaning of its results.
Wun4D: Your bones are weighted to say if it’s good or not. Thus you know what density is.
OP risk factors were generally known by most “aware” and “unaware” women, less frequently by men and with some confusion sometimes. Age, female sex, menopause, family history of OP, calcium/vitamin D deficiency, loss of height, and physical inactivity, but also hard physical occupation were mentioned as OP risk factors. To have suffered a first fragility fracture, a corticoid treatment, tobacco were quoted as potential risk factors by “aware” women only.
On the whole, the level of knowledge on OP was quite similar between aware and unaware participants. However, some points, as OP risk factors, were mentioned only by aware women.
Is OP a disease?
Participants consider OP as asymptomatic and silent.
The question of OP as a disease or a natural bone deterioration was raised in all groups, aware or unaware. It was generally considered as an inevitable consequence of aging, although certain men did describe it as a disease.
Wa5B …it is as the white hair … it can be a consequence of ageing … it is not really a pathology.
MunE4: ... maybe it’s not a disease, it’s just a deficiency that needs to be filled.
Wun4D: ...I’ve never seen someone having an OP being ill...
For men, OP is a women’s problem only
In all focus groups composed of men, OP was considered as a women’s problem, which did not concern them. Most did not have any experience of men with OP among their relatives; they could only report experiences of women suffering from OP.
MunB4: ...I did not even know that OP existed in men.
“Unaware” but also some “aware” men said they had never received any information about it from their GP, even after a fracture. Some “aware” men expressed their surprise and felt embarrassed when they received the diagnosis of OP.
MaR3: “I was surprised with the diagnosis,” said a man with a low BMD T-score.
An osteoporotic participant even spoke of his distress, feeling that his masculine identity was questioned as he had never heard of male OP.
MaES1: “When I discovered this OP in 1993, there was no statistics on men. All the papers that I was given concerned women. For a while I changed sex!” he said, smiling.
Difficulties to associate fragility fractures and OP
There was an interesting paradox in that even if participants considered that a fracture could be a consequence of an underlying OP, they did not feel concerned themselves. Many aware participants who experienced a fragility fracture considered it was an isolated event, an accident due to the fall or the violence of the impact. Men more frequently than women did not connect their fracture with bone fragility or bone health.
Wa5A: I had 2 fractures; at first the elbow, because I had a fall. Then the wrist….it’s beginning to frighten me! But I thought, no: it is because I had a very violent impact, anyone would have fractured.
MunD1: There must be accidents apparently not serious, but resulting in a fracture because of the presence of OP ... I had 2 fractures. Both times it was an accident, very clearly. The first time, I slipped .... And the second time, in the street, my hands were in my pockets, I fell and it’s there that it broke.
Men and women, “aware” or not, did not feel concerned by OP
Participants often under-estimated their personal risk of fracture, mostly those who never had a fracture but also those who had one, as the fracture was often considered as a “traumatic” event. They did not feel concerned even when they had received an OP diagnosis and benefited from information about OP. OP was often minimized and not considered as serious compared to cancer or heart disease.
Wun3A: …OP concerns people who are thin and fragile, who are 90 years old.
MaR3 who knew he was osteoporotic: I do not feel anything. Perhaps if something happens, a fracture, so that I would change my mind.
Wun1: I think about it from time to time ... I go swimming, do gymnastics and hiking. I would not want at all to be forced to give up this because of that.
Others, among the “aware” men and women, perceived the risk and tried to reduce their activity in an attempt to reduce the risk of fracture.
MaES1: when you have OP, you have to be careful... I used to play tennis, windsurfing, but I stopped.
Women expressed their fear of OP and old age
Overall, women had a better knowledge of OP than men (Table 3). They generally associated OP with fracture and aging, but also with frailty, disability, and even death. They had the image of a “bent old lady,” with restricted physical capacities.
Wun1A:The little ladies who walk very bent, who have difficulties to raise their eyes, who walk with a walking stick, who can do nothing.
Wa3D: …When you are told that you have OP, it means that you are getting old. It is not very pleasant.
Women, more than men, evoked the psychological consequences of being diagnosed with OP, they discussed the psychological consequences of being diagnosed with OP, the fear of falls and fractures that will restrict their activities. It may create anxiety of becoming frail, disabled, and dependent on others, but also to be considered frail by the relatives and socially isolated.
Wa2D: It’s more the rest of the family who is afraid and is always telling me: “you have to be careful”. But I do not want to! I do not like being told “be careful”.
Wun4D: ...it’s the loneliness that it generates...
Conversely, men, and particularly “unaware” men, were generally convinced that they had perfect bone health. Some showed a disinterest for OP even if they were concerned.
MaR1who knew he was osteoporotic: As long as we do not have any problem, we do not think about anything.
OP prevention
Generally, both sexes had reasonably good knowledge of the recommendations for OP prevention: to have a healthy lifestyle, a balanced diet, with adequate calcium intake, solar exposure for vitamin D, and physical exercise. However, the benefits of dairy products, sun exposure, and exercise were considered with suspicion and balanced against their possible deleterious effects. Male respondents attached importance to continuing to practice sports at high risk of fracture (e.g., skiing, martial arts). Women were interested in knowing which sport was the most likely to strengthen muscles and bones and to maintain balance and coordination to avoid falling. To reduce the risk of fall by adapting or even limiting certain physical activities was an important part of OP prevention in several female focus groups, both “aware” and “unaware.”
Wun3D: To work on one’s balance, it is very important when you get older
For women, OP prevention should include information campaigns and OP screening, whereas this idea was controversial in focus groups composed of men: as OP is not frequent in men, they considered it useless to implement prevention campaigns.
Wun4B: It is by knowing things that we can better prevent them.
MaH4: If we don’t have a way to treat it, there’s no use in detecting it.
Although some women emphasized the risks associated with the hormonal treatment of menopause; the majority of them were in favor of it to prevent or cure OP.
Women and men mistrust pharmacological treatments
Little was known about OP treatments, except that they have deleterious side effects and strict administration requirements in all groups, “aware” or not. For some participants, treatment meant calcium and vitamin D supplementation, associated with prevention through a healthy lifestyle. The names of anti-resorptive drugs were mentioned only by “aware” men or women. Some were suspicious about treatment and reluctant to take a medication for which they did not see immediate benefits. Discussion focused mainly on the side effects and problems of absorption for patients who have received a treatment, i.e., mostly women but also a few men.
Wun2C: The treatment was almost more disabling than the disease.
Wa5B: I had a treatment but I stopped it. ... I do not believe in it.
MunB1: It is terrible, I know this treatment… you have to take it the first two days of the month and for one hour you cannot lie down.
MaES1: ... I had an acute esophagitis and since then I had a hiatal hernia and I am treated for that, it’s very annoying.
Patients’ expectations of the healthcare professionals
Most “unaware” men reported that their GP had never talked to them about OP. Among men who experienced a fracture, some had been advised to check their bone status by the orthopedic surgeon but others did not remember having been told anything.
MunE2: My GP never told me about it. I’m 74!
MaO3: after an accident I had an operation on my hip and the surgeon later said: “you should check if you do not suffer from a weakness of the bones”.
Most participants expected an appropriate management that would be initiated by their GP, concerning a pathology for which they had little information or even that they have never thought of before. Women expected discussion and prevention messages from their GP. Men generally thought that it was the role of the GP to screen for OP if he/she considered they were “at risk” and to treat if necessary. Some men were reluctant to receive prevention advice for a condition that they believed to concern women.
Wa2C: I expect that my physician talks to me about pathologies when you get older; that would seem obvious to me, and that the GP does prevention rather than give us a drug.
MunE2: In addition to prevention, it is the role of the physician to inform his/her patient if he/she thinks that a given patient may be more concerned by OP than others.
Some participants did not trust their GP with regard to OP and preferred to have a specialist referral. Men and women agreed on the fact that often the GPs did not have enough time during the consultation to discuss prevention. Some women mentioned that they received discordant messages from the healthcare providers in charge of their OP, i.e., GPs, gynecologists, and rheumatologists, leading to confusion.
Wun3E: I do not expect much from him for my bones.
Most women expected reliable information and prevention that should be initiated by the GP. They imagined prevention campaigns in the media, dedicated care centers, or a dedicated patient “health book” to trace treatment and follow-up.
“Unaware” men were not all convinced by the usefulness of prevention. However, some men recognized consulting only in emergency situations, leaving little room for prevention.
Each focus group ended with a free discussion; participants had several questions for the moderator and showed interest in having more information. Some reported that they appreciated the opportunity to share their experience with others dealing with the same disease.
Discussion
This focus-group-based study aimed to explore the representations regarding OP and bone health of French men and women, having been affected or not by OP and/or fragility fractures. We found that awareness of OP was poor considering that this study population was expected to be concerned given subjects’ age and, for nearly half of them, a history of fragility facture or an OP diagnosis. Women and men generally associated OP with bone fragility, aging, and fracture, but they did not show a great interest in it.
In line with that reported elsewhere, most of the participants herein could describe OP as bone fragility, associated with aging and fracture, but many, particularly men, had insufficient and sometimes inaccurate knowledge, with frequent confusion with osteoarticular diseases [18, 23, 24]. In the absence of visible signs, there was an ambiguity for participants to describe OP as a disease: it did not meet their classical representation of a disease and was generally described as a natural bone deterioration associated with old age that they had to accept. In the absence of pain or symptom, OP was not considered a serious condition compared to cancer or cardiovascular diseases [15, 18, 23].
Most of the participants herein generally considered a low-energy fracture as an isolated event not related to bone fragility; they explained it by the fall and the violence of impact. Even after a re-fracture, they did not consider themselves at increased fracture risk and, consequently, could not be receptive to OP investigation and medication as described [14, 25, 26]. Giangregorio et al. have reported that awareness of an increased susceptibility to re-fracture decreases in function of patient age, which is worrying as both age and a previous fracture are predictors of re-fracture [14]. It has been proposed that the term “fragility fracture” be reconsidered, as patients do not see anything fragile in their fracture related to a traumatic event and not to bone quality [26].
An interesting fact was that we could not detect an important difference in the perception between “aware” and “unaware” patients; thus, having experienced a fragility fracture or received a diagnosis of OP does not always lead patients to recognize they should be concerned by OP. Indeed, there was ambiguity in the representations of OP and a true paradox: participants usually associated OP with bone fragility and fracture but did not relate their own fractures to OP. “Aware” men and women often under-estimated their condition when they were personally concerned. They did not feel sick and denied the evidence, as described in other studies, mainly for women [15, 17, 23].
However, there were differences between the perceptions of men and women. The perceptions of men on OP have rarely been gathered and the few published studies have shown that OP is generally considered as a women’s problem although the prevalence of OP and low bone density in men over 65 years of age reaches approximately 45% [27, 28]. Compared to women, men had a more limited and sometimes inaccurate knowledge on OP that they often associated with women. They generally considered that they had a perfect bone health and felt confident in their capacity to have a lifestyle compatible with a good bone health [27]. Although male OP is recognized nowadays, Although male osteoporosis is recognized nowadays, it has long been considered a female disease only, which probably delays its recognition as a male disease in both the general population and among health care providers [29, 30].
Conversely to men, women had a better knowledge of OP that they associated with frailty, aging, fractures, dependence, and end of life. For some women, to be diagnosed as osteoporotic may create anxiety of becoming frail, disabled, dependent on others, and socially isolated, but also to be considered vulnerable and frail by the relatives. It is important for healthcare providers to understand the feelings and perceptions of their patients with regard to OP and to provide them with adapted, meaningful, and usable knowledge. This will enable patients to make sense of the diagnosis and improve their adherence to prevention measures and treatments. Several theoretical models were proposed to describe the different steps of the management of illnesses. One of these, Leventhal’s common sense model, provides a framework to explain the multi-level process by which patients become aware of health threat and manage to cope with it; it may be adapted to OP and fit with the ideas expressed by our patients [18, 25, 31].
Most had heard about BMD but they were not certain about the goal of the test and the meaning of its results and had difficulties to understand the diagnosis, as has been described elsewhere [15]. We recently reported in a population of women with a fragility fracture and a low BMD that only 61% could report this result, while 49% considered they had a normal BMD [20]. These data point to a lack of efficacy in the communication between healthcare professionals and patients: the message given by the medical staff is probably not clear enough and/or misunderstood by the patient. Prevention measures, i.e., a balanced diet, calcium intake, solar exposure for vitamin D, physical exercise, and fall prevention, were generally known by most participants, particularly women; to have a healthy lifestyle was considered beneficial to health in general. A few women herein expressed their fear of fall and fracture and self-limited their activities, as has been reported in other countries [18, 32]. Furthermore, women perceiving a risk for OP tend to avoid weight-bearing sports to put less strain on their bone [33]. Men, especially those “unaware,” considered that they had a perfect bone health and could carry on practicing at-risk activities. Even if they knew their personal risk factors and prevention measures, some interviewees, particularly men, were not ready to change their way of life to prevent OP, as they did not perceive any threat [24, 29].
Pharmacological treatments were mainly known for their deleterious side effects and dosing recommendations rather than for their positive effects. The negative information sometimes delivered by the media may render it difficult for the physician to explain the benefits and risks of the treatments [17, 25]. In addition, GPs are sometimes reluctant to prescribe OP treatment for the same reasons: side effects, doubt as to their efficacy, over-medicated elderly patients [17, 34]. If the GP is not convinced of the benefit, the patient is less likely to be convinced to begin a long-term treatment, for an improvement he/she will not perceive. These results are in accordance with the low OP treatment prescription and adherence worldwide [35,36,37].
The participants of the present study, especially women, generally considered that it is the role of the GP to initiate the investigation for OP and give prevention advices. To induce a change in the management of OP, the first step is to inform patients without creating anxiety, to make them perceive the threat and raise confidence in their ability to be active in the management of their health. Health empowerment focuses on bringing patients with basic knowledge and skills to raise awareness of their health status and help them to engage successfully in an adapted health behavior [38]. The data presented herein indicate that people lacked basic knowledge of OP but were interested to have more information. Education and prevention should focus on the possibilities rather than the limitations, showing that it is possible to live with OP considering preventive measures, without the constant threat of the fracture [39]. To provide patients with evidence-based information tailored to the needs of patient groups considering sex, age, and social context should facilitate discussion with their GP and increase patient involvement in OP management. This also implies a reinforcement of knowledge of OP care in healthcare providers.
The present study has strengths and limitations. The design with the inclusion of men and women both “aware” and “unaware” of OP allowed us to analyze beliefs according to four types of participants, which is unique since other studies in the field usually target one specific population [17, 33, 40]. However, it was conducted among patients who volunteered to participate; the “unaware” participants were recruited through a health insurance company, excluding a more fragile population not subscribing to any health insurance. Thus, the population may be biased towards those more actively engaged in their health and with a higher education, explaining, at least in part, why there was no great difference between “aware” and “unaware” men and women. Furthermore, it was conducted in the French health system in which the cost of the BMD test following a fragility fracture and of OP treatment after menopause or fragility fracture is covered by the national healthcare insurance; it therefore might not be representative of other healthcare systems. Nevertheless, this type of interviews in small groups allows participants to interact and to express their concerns and priorities. In addition, the participants reported they appreciated the opportunity to share their experience with others dealing with the same disease.
In conclusion, the present study highlighted the barriers to OP care in an elderly French population and showed that women and men often lack relevant information to deal with the disease. This may allow patient’s education to be adjusted to men and women representations and concerns about osteoporosis that could improve patients’ engagement in their health.
References
Kanis JA, Melton LJ 3rd, Christiansen C, Johnston CC, Khaltaev N (1994) The diagnosis of osteoporosis. J Bone Miner Res 9:1137–1141
Strom O, Borgstrom F, Kanis JA, Compston J, Cooper C, McCloskey EV, Jonsson B (2011) Osteoporosis: burden, health care provision and opportunities in the EU: a report prepared in collaboration with the international Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 6:59–155
Hernlund E, Svedbom A, Ivergard M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jonsson B, Kanis JA (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8:136
Svedbom A, Hernlund E, Ivergard M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jonsson B, Kanis JA, EURPo IOF (2013) Osteoporosis in the European Union: a compendium of country-specific reports. Arch Osteoporos 8:137
Maravic M, Taupin P, Landais P, Roux C (2011) Change in hip fracture incidence over the last 6 years in France. Osteoporos Int 22:797–801
Briot K, Cortet B, Thomas T et al (2012) 2012 update of French guidelines for the pharmacological treatment of postmenopausal osteoporosis. Joint Bone Spine 79:304–313
Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster JY, Scientific Advisory Board of the European Society for C, Economic Aspects of O, Osteoarthritis, the Committee of Scientific Advisors of the International Osteoporosis F (2013) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 24:23–57
Ganda K, Puech M, Chen JS, Speerin R, Bleasel J, Center JR, Eisman JA, March L, Seibel MJ (2013) Models of care for the secondary prevention of osteoporotic fractures: a systematic review and meta-analysis. Osteoporos Int 24:393–406
Mitchell PJ (2013) Best practices in secondary fracture prevention: fracture liaison services. Curr Osteoporos Rep 11:52–60
Nayak S, Greenspan SL (2018) How can we improve osteoporosis care? A systematic review and meta-analysis of the efficacy of quality improvement strategies for osteoporosis. J Bone Miner Res 33:1585–1594
Leslie WD, Giangregorio LM, Yogendran M, Azimaee M, Morin S, Metge C, Caetano P, Lix LM (2012) A population-based analysis of the post-fracture care gap 1996–2008: the situation is not improving. Osteoporos Int 23:1623–1629
Giangregorio L, Papaioannou A, Cranney A, Zytaruk N, Adachi JD (2006) Fragility fractures and the osteoporosis care gap: an international phenomenon. Semin Arthritis Rheum 35:293–305
Cheng N, Green ME (2008) Osteoporosis screening for men: are family physicians following the guidelines? Can Fam Physician 54:1140–1141 1141 e1141–1145
Giangregorio L, Papaioannou A, Thabane L, DeBeer J, Cranney A, Dolovich L, Adili A, Adachi JD (2008) Do patients perceive a link between a fragility fracture and osteoporosis? BMC Musculoskelet Disord 9:38
Sale JE, Beaton DE, Sujic R, Bogoch ER (2010) ‘If it was osteoporosis, I would have really hurt myself.’ Ambiguity about osteoporosis and osteoporosis care despite a screening programme to educate fragility fracture patients. J Eval Clin Pract 16:590–596
Malochet-Guinamand S, Chalard N, Billault C, Breuil N, Ristori JM, Schmidt J (2005) Osteoporosis treatment in postmenopausal women after peripheral fractures: impact of information to general practitioners. Joint Bone Spine 72:562–566
Alami S, Hervouet L, Poiraudeau S, Briot K, Roux C (2016) Barriers to effective postmenopausal osteoporosis treatment: a qualitative study of patients’ and practitioners’ views. PLoS One 11:e0158365
Weston JM, Norris EV, Clark EM (2011) The invisible disease: making sense of an osteoporosis diagnosis in older age. Qual Health Res 21:1692–1704
Kitzinger J (1995) Qualitative research. Introducing focus groups. BMJ 311:299–302
Merle B, Chapurlat R, Vignot E, Thomas T, Haesebaert J, Schott AM (2017) Post-fracture care: do we need to educate patients rather than doctors? The PREVOST randomized controlled trial. Osteoporos Int 28:1549–1558
Chaitou A, Boutroy S, Vilayphiou N, Munoz F, Delmas PD, Chapurlat R, Szulc P (2010) Association between bone turnover rate and bone microarchitecture in men: the STRAMBO study. J Bone Miner Res 25:2313–2323
Lau E, Papaioannou A, Dolovich L, Adachi J, Sawka AM, Burns S, Nair K, Pathak A (2008) Patients’ adherence to osteoporosis therapy: exploring the perceptions of postmenopausal women. Can Fam Physician 54:394–402
Barker KL, Toye F, Lowe CJ (2016) A qualitative systematic review of patients’ experience of osteoporosis using meta-ethnography. Arch Osteoporos 11:33
Baheiraei A, Ritchie JE, Eisman JA, Nguyen TV (2006) Exploring factors influencing osteoporosis prevention and control: a qualitative study of Iranian men and women in Australia. Maturitas 54:127–134
Besser SJ, Anderson JE, Weinman J (2012) How do osteoporosis patients perceive their illness and treatment? Implications for clinical practice. Arch Osteoporos 7:115–124
Sale JE, Gignac MA, Frankel L, Hawker G, Beaton D, Elliot-Gibson V, Bogoch E (2012) Patients reject the concept of fragility fracture--a new understanding based on fracture patients communication. Osteoporos Int 23:2829–2834
Gaines JM, Marx KA (2011) Older men’s knowledge about osteoporosis and educational interventions to increase osteoporosis knowledge in older men: a systematic review. Maturitas 68:5–12
Solimeo SL (2011) Living with a ‘women’s disease’: risk appraisal and management among men with osteoporosis. J Mens Health 8:185–191
Solimeo SL, Weber TJ, Gold DT (2011) Older men’s explanatory model for osteoporosis. Gerontologist 51:530–539
Banu J (2013) Causes, consequences, and treatment of osteoporosis in men. Drug Des Devel Ther 7:849–860
Leventhal H, Benyamini Y, Brownlee S, Diefenbach M, Leventhal EA, Patrick-Miller L, Robitaille C (1997) Illness representations: theoretical foundations. In: Petrie KJ, Weinman JA (eds) Perceptions of health and illness. Harwood Academic, Amsterdam, pp 19–45
Reventlow SD, Hvas L, Malterud K (2006) Making the invisible body visible. Bone scans, osteoporosis and women’s bodily experiences. Soc Sci Med 62:2720–2731
Reventlow SD (2007) Perceived risk of osteoporosis: restricted physical activities? Qualitative interview study with women in their sixties. Scand J Prim Health Care 25:160–165
Fogelman Y, Goldshtein I, Segal E, Ish-Shalom S (2016) Managing osteoporosis: a survey of knowledge, attitudes and practices among primary care physicians in Israel. PLoS One 11:e0160661
Iversen MD, Vora RR, Servi A, Solomon DH (2011) Factors affecting adherence to osteoporosis medications: a focus group approach examining viewpoints of patients and providers. J Geriatr Phys Ther 34:72–81
Yu J, Brenneman SK, Sazonov V, Modi A (2015) Reasons for not initiating osteoporosis therapy among a managed care population. Patient Prefer Adherence 9:821–830
Lindsay BR, Olufade T, Bauer J, Babrowicz J, Hahn R (2016) Patient-reported barriers to osteoporosis therapy. Arch Osteoporos 11:19
Crawford Shearer NB (2009) Health empowerment theory as a guide for practice. Geriatr Nurs 30:4–10
Nielsen D, Huniche L, Brixen K, Sahota O, Masud T (2013) Handling knowledge on osteoporosis--a qualitative study. Scand J Caring Sci 27:516–524
Meadows LM, Mrkonjic L, Lagendyk L (2005) Women’s perceptions of future risk after low-energy fractures at midlife. Ann Fam Med 3:64–69
Acknowledgements
The authors thank APICIL for having given access to their members and the women and men who took part in the study and accepted to share their ideas and experiences.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the local ethics committee (Institutional Review Board: IORG0007394. Ref: IRBN092014/CHUSTE).
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Merle, B., Dupraz, C., Haesebaert, J. et al. Osteoporosis prevention: where are the barriers to improvement in a French general population? A qualitative study. Osteoporos Int 30, 177–185 (2019). https://doi.org/10.1007/s00198-018-4720-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-018-4720-5