Abstract
Summary
This study examined the association between healthy lifestyle score (HLS), which contained 7 items (smoking, BMI, physical activity, diet, alcohol, sleep and anxiety) and BMD. Results showed HLS was positively associated with BMD at all studied sites, suggesting that healthier lifestyle patterns might be beneficial to bone health.
Purpose
Previous studies have reported favourable associations of individual healthy lifestyle factors with bone mineral density (BMD), but limited evidence showed the relationship of a combined healthy lifestyle score (HLS) with BMD. This study examined the association between the HLS and BMD.
Methods
This community-based cross-sectional study included 3051 participants aged 40–75 years. The HLS contained 7 items (smoking, BMI, physical activity, diet quality, alcohol intake, sleep and anxiety). BMD values of whole body (WB), lumbar spine 1–4 (L1–4), total hip (TH) and femur neck (FN) were measured using dual-energy X-ray absorptiometry.
Results
After adjusting for potential covariates, HLS was positively associated with BMD at all studied sites (P-trend < 0.01). The mean BMDs were 2.69% (WB), 5.62% (L1–4), 6.13% (TH) and 5.71% (FN) higher in participants with HLS of 6–7 points than in those with HLS of 0–2 points. The per 1 of 7 unit increase in the HLS was associated with increases of 7.63 (WB)–13.4 (TH) mg/cm2 BMD levels at all sites. These favourable associations tended to be more pronounced in men than in women. Among the 7 items, physical activity contributed most to the favourable associations, followed by BMI, non-smoking and diet; the other three items played little roles. Sensitivity analyses showed that the significant associations remained after excluding any one of the 7 components or excluding fracture subjects at all sites.
Conclusion
Higher HLS was associated with greater BMD in middle-aged and elderly Chinese, suggesting that healthier lifestyle patterns might be beneficial to bone health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis (OP) is a systemic skeletal disease characterized by low bone mass and microarchitectural deterioration. It is the world’s third most incident chronic disease after cardiovascular disease (CVD) and diabetes [1]. There were approximately 200 million (6.96%) OP patients around the globe in 2008 [1, 2]. In China, the prevalence of osteoporosis in those over the age of 50 was 23.9% and 12.5% in women and 3.2% and 5.3% in men, respectively, at the lumbar spine and femur neck [3]. Lifestyle played an indispensable role in various chronic diseases, including OP. Many studies have indicated favourable associations of some individual healthy lifestyle factors, such as non-smoking [4], proper body weight [5], moderate physical activity [6], healthy diet [7, 8], moderate alcohol intake [9], good sleep [10] and low anxiety levels [11], with bone health. However, each specific healthy behaviour was able to coexist with the others, and these behaviours may synergistically influence people’s health [12, 13]. Combining these relevant behaviours into one single measure of the whole lifestyle, such as the healthy lifestyle score (HLS), may be useful in assessing synergistic associations than using each individual behaviour.
A variety of studies have calculated the HLS and showed associations of higher HLS with lower incidence or mortality of CVD [14,15,16,17,18], some cancers [19,20,21,22] and some other diseases [23, 24]. In these studies, the HLS was typically composed of the following factors: smoking, body weight or body mass index (BMI), physical activity, diet, alcohol consumption, sleep, etc. To date, few studies have examined the association between HLS and bone health. Only two studies investigated an alternative HLS known as the American Heart Association Diet and Lifestyle Score (AHA-DLS), which combines BMI, physical activity, diet and alcohol intake, and showed significant protective associations with BMD [25, 26]. However, the AHA-DLS does not include smoking, mental stress and sleeping variables, and this measure was designed mainly for use in studies focused on the prevention of CVD. Therefore, the AHA-DLS measure might not be appropriate for bone health; it might be less specific in describing the association between lifestyle and BMD. Moreover, each individual component was given the same weight in the HLS calculations in most previous studies, although the strengths of the associations may differ for the different component lifestyle factors [20, 27].
To address these issues, this cross-sectional study examined the association between an HLS containing 7 lifestyle factors and BMD in the whole body, lumbar spine, total hip and femur neck in a middle-aged and elderly Chinese population and explored the optimal weight for each item based on a regression model.
Methods
Study participants
The study was based on the Guangzhou Nutrition and Health Study (GNHS), in which 4048 participants aged 40–75 and have lived in urban Guangzhou (South China) for more than 5 years were recruited from 2008 to 2010 (n = 3169) and in 2013 (n = 879). Of the first bunch of 3169 participants (2008–2010), 659 subjects were lost to follow-up in 2011–2013. Among 3389 participants who attended the survey during 2011–2013, 338 subjects were further excluded due to the following conditions: (1) history of serious diseases (n = 47), such as malignancy or hyperthyroidism; (2) missing core data (n = 211); and (3) extreme energy intakes (< 800 or > 4200 kcal/d for men and < 600 or > 3500 kcal/d for women) (n = 80). Finally, 3051 subjects (including 2065 women and 986 men; 2458 followed up and 593 newly recruited) who completed at least one round of questionnaires and bone scanning by dual-energy X-ray absorptiometry (DXA) in 2011–2013 were included in this cross-sectional analysis (Fig. 1). Informed consent was obtained from all individual participants included in the study. The study was conducted under the guidance and regulations of the Ethics Committee of the School of Public Health at the Sun Yat-Sen University.
Assessment of lifestyle behaviours and other covariates
Subjects were invited to the School of Public Health at the Sun Yat-sen University for face-to-face interviews and body assessments, and the following information was collected: demographic characteristics (e.g. age, sex, education, marital status and household income), habitual diet, sleep conditions, anxiety neurosis, history of diseases, use of supplements (e.g. multiple vitamins, calcium supplements and oral oestrogens) and other lifestyle factors (e.g. smoking, drinking and physical activity).
Smoking involved both active and passive smoking. Active smoking was defined as smoking more than 5 packs of cigarettes (100 cigarettes) in the past year. Passive smoking was defined as exposure to more than 1 cigarette or 5 min of indoor smoking every day in the past year. Physical activity included moderate and vigorous activities during work, leisure time and household chores. BMI values were calculated by measuring subjects’ heights and weights. Sleep conditions were obtained by asking subjects whether they had insomnia for more than half a year. The Self-Rating Anxiety Scale (SAS) was used to evaluate the subjects’ level of anxiety neurosis [28]. It consists of 20 items and a full score of 100 points.
Modified alternate Mediterranean diet score
A pre-validated 79-item food-frequency questionnaire [29] was used to collect the subjects’ dietary information. The diet component of HLS was defined by using the alternate Mediterranean diet (aMed) score [30, 31]. We further modified the aMed score by removing alcohol intake because it was used as a separate factor in the HLS [31]. The final modified aMed score (0–8 points) included 8 items assigned a value of 0/1 for each component [30]: energy-adjusted whole grains, vegetables (excluding potatoes), fruit (including juices), legumes, nuts, fish, ratio of monounsaturated fatty acid (MUFA) to saturated fatty acid (SFA) and red or processed meats.
Healthy lifestyle score (HLS)
The definition of the HLS varies among studies [19, 27]. In this analysis, seven lifestyle-related components were selected: smoking, physical activity, BMI, modified aMed score, alcohol intake, sleep and anxiety. Each component was dichotomized as healthy or unhealthy. One point was given to each item representing a healthy condition according to the following criteria [16, 32]: (1) non-smoking, (2) physically active (≥ 150 min/week of moderate or vigorous physical activity), (3) standard BMI (18.5 to 23.9 kg/m2), (4) healthy diet (5–8 points of modified aMed Score), (5) moderate alcohol intake (men, 10–50 g/d; women, 5–25 g/d), (6) good sleep (no insomnia for < 6 months) and (7) no anxiety neurosis (SAS < 50). The total points ranged from 0 (least healthy) to 7 (most healthy). Specific information about these HLS criteria can be found in Supplementary Table 1.
BMD assessment
BMD (g/cm2) was measured by dual-energy X-ray absorptiometry (DXA) (Discovery W, Hologic Inc., Waltham, MA, USA) and analysed with Hologic Discovery software version 3.2 during 2011–2013. The measured skeletal sites were whole body (WB), lumbar spine 1–4 (L1–4), total hip (TH) and femur neck (FN). The in vivo coefficients of variation (CV) of the duplicated BMD measurements in 30 subjects after repositioning were 1.18% (WB), 0.87% (LS), 1.02% (TH) and 1.92% (FN), respectively. The long-term CV of the measurements was 0.26%, a value found by testing the phantom daily between March 2011 and May 2015 [33].
Statistical analysis
Baseline characteristics were presented as mean (standard deviation, SD) or frequencies (percent), and the ANOVA and chi-square analyses were used to examine differences among the HLS groups, for the continuous or categorical variables, respectively.
Multivariate analysis of covariance (ANCOVA) was used to compare the mean BMD values among the five HLS groups. Model I was adjusted for age and sex. In model II, we further adjusted for marital status, education status, household income, calcium supplement use, multivitamin use and daily energy intake. A Bonferroni test was conducted to make multiple comparisons. Liner regression was also used to obtain the coefficients (β), standardized error (SE) and standardized β (sβ) of the HLS.
A stratified analysis was performed with the use of ANCOVA and linear regression according to sex under model II; years since menopause and use of oestrogen were further adjusted for in the analysis limited to females. We also evaluated the association of each binary lifestyle factor with BMD under model II and further adjusted for the other factors in the HLS except the one being analysed.
We conducted the following sensitivity analyses: (1) the stability of the HLS: we excluded each component in turn and excluded subjects with a history of fractures. (2) The associations were reanalysed by weighting the HLS according to the corresponding sβ values of the 7 factors (weighti = [sβi/(∑sβi)] × 7); and (3) the contribution of the current HLS was compared with the modified AHA-DLR [25, 26]. All analyses were performed with SPSS 22.0 for Windows (SPSS, Inc., NY, USA). A two-sided P value < 0.05 was considered statistically significant.
Results
A total of 3051 subjects (2065 women and 986 men) were included in this study. As HLS increased, subjects had higher levels of household incomes, education, physical activity, energy intake and dietary intakes of whole grain, vegetables, fruits, legumes, nuts and fish; subjects with increased HLS also had higher proportion of calcium and multivitamin supplement use but lower levels of body weight and BMI and fewer subjects with current smoking, insomnia and anxiety. There were no significant associations with HLS for other factors in Table 1 (P values ≥ 0.05).
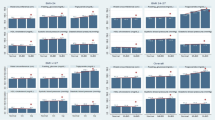
In all subjects (Table 2), higher HLS was significantly associated with higher BMD at most bone sites (except L1–4) after adjusting for age and sex in model I. The BMDs in the highest HLS (6–7 points) group were 2.87 (WB)–6.42% (FN) higher than those in the lowest HLS (0–2 points) group (all P values < 0.01). The association between HLS and BMD was strengthened after further adjusting for multiple covariates in model II. The percentage mean BMD differences between the extreme groups were 2.69% (WB), 5.62% (L1–4), 6.13% (TH) and 5.71% (FN). The changes in BMD (mg/cm2) associated with per 1 of 7 unit increase in HLS were 7.63 (WB), 12.2 (L1–4), 13.4 (TH) and 11.6 (FN) (all P values < 0.01) (Table 2). In the sex-stratified analysis in model II, the favourable associations tended to be relatively more pronounced in men than in women, although significant associations were observed at all studied sites in men and in women (Table 3).
We compared mean BMD differences between binary groups classified by each HLS component (Table 4). Among the 7 components of the HLS, physical activity played a leading role in the favourable association between HLS and BMD, followed by smoking, BMI and the aMed score. The BMDs were 1.19% (WB) to 2.36% (FN) higher in subjects with higher (vs. lower) physical activity (all P values < 0.001). No significant differences in BMD for the other three components (alcohol intake, sleep and anxiety) were observed at any studied site.
The sensitivity analyses showed that significant associations remained after excluding either one of the 7 components or those with a history of fractures. After adjusting AHA-DLS, the favourable associations of HLS with BMD remained significant at all studied sites (Supplementary Table 3).
Discussion
In this community-based cross-sectional study, the score of this 7-item HLS was positively associated with BMD in this middle-aged and elderly Chinese population, which suggested that subjects with better adherence to a healthy lifestyle pattern (standard BMI, non-smoking, moderate exercise, healthy diet, moderate alcohol intake, good sleep and no anxiety) might have better bone health.
HLS and bone health
Although many studies have examined each component of the 7-item HLS with BMD [4,5,6,7,8,9,10,11], few studies have reported synergistic associations between lifestyle score and bone health. Two cross-sectional studies examined the association of the AHA-DLS, which contains 4 lifestyle factors (BMI, physical activity, diet and alcohol intake), with BMD or osteoporosis [25, 26]. One study in 933 Puerto Rican subjects (aged 47–79 years) found that each 5 of 110 unit increase of the AHA-DLS was associated with a 5–8 mg/cm2 (or 5.5–8.8 per 5% unit) increased BMD as well as a lower prevalence of osteoporosis/osteopenia (OR, 0.83–0.91) at the hip sites and lumbar spine (all P values < 0.05) [25]. Another study showed a significant increase in BMD (4.20–6.07 mg/cm2) in the whole body, lumbar spine and hip sites with each 5% increase in the BMI-excluded AHA-DLS in 3143 Chinese women and men aged 40–75 years (all P values < 0.01) [26].
Since several other important lifestyle-related factors, such as smoking, sleeping habits and mental stress, were not included in the AHA-DLS, we calculated a more comprehensive HLS by including 7 items (non-smoking, physically active, normal BMI, healthy diet, moderate alcohol intake, good sleep and low anxiety neurosis), as has been done in many other studies of chronic diseases [19, 23, 27]. Each 1 of 7 unit increase in HLS was associated with an increase of 7.6–13.4 mg/cm2 BMD at the studied sites in this analysis. The differences in BMDs between the groups of HLS 6–7 and 0–2 in this study represent risk increases of fractures by 24.9% (lumber spine) and 34.2% (FN) [34]. The corresponding changes of T score of HLS 0–2 were − 0.29 (L1–4) and − 0.30 (FN) [3, 35], and changes of PMOF were 1.09% (L1–4) and 1.04% (FN), respectively [36]. This 7-item HLS had a significant association with BMD even adjusted for the AHA-DLS, suggesting that this 7-item HLS had extra contribution in the prediction of BMD in this population (Supplementary Table 3).
Given that lifestyle behaviours may show different impacts on BMD, simply adding equally weighted scores of the 7-item lifestyle factor may lead to misclassification. To address this issue, we weighted each item according to their sβs. The results showed the β, R2 and R2 change of HLS and wHLS were similar (Supplementary Table 3). Considering the complicated nature of calculating the weighted HLS, the HLS with equal weights for each item would be more applicable for public use.
HLS components and bone health
Among the 7 components of the HLS, physical activity played a leading role in the favourable association between HLS and BMD. The BMDs in subjects with higher (vs. lower) physical activity were 1.19 (WB)–2.36% (FN) higher at the studied sites (all P values < 0.001). A meta-analysis of 22 cohort studies with 1,235,768 participants and 14,843 fractures showed that the pooled relative risk (RR, 95% CI) for the highest versus lowest category of physical activity was 0.71 (0.63–0.80) for total fractures, 0.61(0.54–0.69) for hip fracture and 0.72 (0.49–0.96) for wrist fracture [37]. Physical exercise creates mechanical strain on the bones, which deforms bone tissue and promotes bone formation and bone remodelling to maintain bone mass and increase bone density [38].
The other favourable determinants among the HLS components in this study were non-smoking, normal BMI and a higher aMed diet quality score. Consistent with previous results that were reviewed in a meta-analysis [4], our findings showed that smoking was a strong risk factor for decreased BMD at most sites (except L1–4). We also observed that subjects with normal BMI (18.5–23.9 kg/m2) had 1.61% (FN) and 2.76% (L1–4) higher BMDs than those with low (< 18.5 kg/m2) or high (≥ 24.0 kg/m2) BMI. Possibly due to the biphasic effect of high BMI caused by higher weight load and more fat, U-shaped (for women) and reverse J-shaped (for men) associations were also observed between BMI and hip fracture in a Korean cohort study of 288,068 individuals [39]. A meta-analysis showed that subjects with the highest (vs. lowest) Mediterranean Diet score had a higher BMD of 0.12 g/cm2, 0.10 g/cm2 and 0.11 g/cm2 at the lumber spine, femoral neck and total hip [40]. The above-mentioned studies and our findings support an association between a good lifestyle, in terms of physical activity, non-smoking, moderate BMI and better diet quality, and better bone health.
Interestingly, our group found a significant synergistic association of HLS combined alcohol intake, sleep and anxiety with BMD (Supplementary Table 3), although the associations observed between each individual factor and total hip BMD were not significant (Table 4). It was possible that there was a synergistic action between the various components of the HLS such that the effect of the sum, on BMD, was greater than its parts. Our results reinforced the importance of a pattern of healthy lifestyle behaviours rather than any single lifestyle choice in protecting BMD.
Strengths and limitations
There are several strengths in our study. First, to the best of our knowledge, this is the first study to examine the association of the 7-item HLS with BMD based on a relatively large sample. Improving patterns seemed to be more effective than changing each single item [41]. Our findings provide a potential clue for the improvement of bone health via the HLS approach. Second, the sensitivity analyses generally showed a consistent favourable association, suggesting good internal consistency for the HLS evaluated.
Our study has several limitations. First, the HLS items and the cut-offs for each item were chosen for general health or major chronic diseases and not specifically for bone health. Second, the sleep conditions were obtained by simply asking whether subjects had insomnia for over half a year instead of using a systematic index, such as the Pittsburgh Sleep Quality Index. Third, the cross-sectional study design limits the ability to infer causality between the HLS and BMD. Typically, the studied association might be attenuated but not overestimated because healthier lifestyles would be advised to the participants with poor BMD. Fourthly, we did not compare the frequency data used in our study and the diary for physical activity questionnaire, although the questionnaire had good long-term reliability (r 0.646, P < 0.001) between baseline and the next survey after 3 years apart.
In conclusion, there was a favourable association between the 7-item HLS and BMD in this middle-aged and elderly Chinese population. Our findings suggested that a healthier lifestyle pattern suggested for general health might also be helpful for bone health in this population. HLS-based interventional studies are needed to address the causality between the HLS and BMD.
Abbreviations
- OP:
-
Osteoporosis
- HLS:
-
Healthy lifestyle score
- CVD:
-
Cardiovascular disease
- BMI:
-
Body mass index
- AHA-DLS:
-
American Heart Association Diet and Lifestyle Score
- GNHS:
-
Guangzhou Nutrition and Health Study
- DXA:
-
Dual-energy X-ray absorptiometry
- aMed:
-
Alternate Mediterranean diet
- MUFA:
-
Monounsaturated fatty acid
- SFA:
-
Saturated fatty acid
- SAS:
-
Self-Rating Anxiety Scale
- WB:
-
Whole body
- L1–4 :
-
Lumbar spine 1–4
- TH:
-
Total hip
- FN:
-
Femur neck
References
Cole ZA, Dennison EM, Cooper C (2008) Osteoporosis epidemiology update. Curr Rheumatol Rep 10:92–96
Cooper C, Melton LJ 3rd. (1992) Epidemiology of osteoporosis. Trends Endocrinol Metab 3:224–229
Zhang ZQ, Ho SC, Chen ZQ, Zhang CX, Chen YM (2014) Reference values of bone mineral density and prevalence of osteoporosis in Chinese adults. Osteoporosis Int 25:497–507
Ward KD, Klesges RC (2001) A meta-analysis of the effects of cigarette smoking on bone mineral density. Calcif Tissue Int 68:259–270
Morin S, Leslie WD (2009) Manitoba bone density program. High bone mineral density is associated with high body mass index. Osteoporosis Int 20:1267–1271
Wee J, Sng BY, Shen L, Lim CT, Singh G, Das De S (2013) The relationship between body mass index and physical activity levels in relation to bone mineral density in premenopausal and postmenopausal women. Arch Osteoporosis 8:162
McTiernan A, Wactawski-Wende J, Wu L, Rodabough RJ, Watts NB, Tylavsky F, Freeman R, Hendrix S, Jackson R, Women's Health Initiative Investigators (2009) Low-fat, increased fruit, vegetable, and grain dietary pattern, fractures, and bone mineral density: the Women’s Health Initiative Dietary Modification Trial. Am J Clin Nutr 89:1864–1876
Movassagh EZ, Vatanparast H (2017) Current evidence on the association of dietary patterns and bone health: a scoping review. Adv Nutr 8:1–16
Sommer I, Erkkilä AT, Järvinen R, Mursu J, Sirola J, Jurvelin JS, Kröger H, Tuppurainen M (2013) Alcohol consumption and bone mineral density in elderly women. Public Health Nutr 16:704–712
Saint Martin M, Labeix P, Garet M, Thomas T, Barthélémy JC, Collet P, Roche F, Sforza E (2016) Does subjective sleep affect bone mineral density in older people with minimal health disorders? The PROOF cohort. J Clin Sleep Med 12:1461–1469
Williams LJ, Bjerkeset O, Langhammer A, Berk M, Pasco JA, Henry MJ, Schei B, Forsmo S (2011) The association between depressive and anxiety symptoms and bone mineral density in the general population: the HUNT study. J Affect Disord 131:164–171
Berrigan D, Dodd K, Troiano RP, Krebs-Smith SM, Barbash RB (2003) Patterns of health behavior in U.S. adults. Prev Med 36:615–623
Reeves MJ, Rafferty AP (2005) Healthy lifestyle characteristics among adults in the United States, 2000. Arch Intern Med 165:854–857
Wang Y, Tuomilehto J, Jousilahti P, Antikainen R, Mähönen M, Katzmarzyk PT, Hu G (2011) Lifestyle factors in relation to heart failure among Finnish men and women. Circ Heart Fail 4:607–612
Djousse L, Driver JA, Gaziano JM (2009) Relation between modifiable lifestyle factors and lifetime risk of heart failure. JAMA 302:394–400
Larsson SC, Tektonidis TG, Gigante B, Akesson A, Wolk A (2016) Healthy lifestyle and risk of heart failure: results from 2 prospective cohort studies. Circ Heart Fail 9:e002855
Agha G, Loucks EB, Tinker LF, Waring ME, Michaud DS, Foraker RE, Li W, Martin LW, Greenland P, Manson JAE, Eaton CB (2014) Healthy lifestyle and decreasing risk of heart failure in women: the Women’s Health Initiative observational study. J Am Coll Cardiol 64:1777–1785
Del Gobbo LC, Kalantarian S, Imamura F et al (2015) Contribution of major lifestyle risk factors for incident heart failure in older adults: the cardiovascular health study. JACC Heart Fail 3:520–528
Buckland G, Travier N, Huerta JM, Bueno-de-Mesquita HB, Siersema PD, Skeie G, Weiderpass E, Engeset D, Ericson U, Ohlsson B, Agudo A, Romieu I, Ferrari P, Freisling H, Colorado-Yohar S, Li K, Kaaks R, Pala V, Cross AJ, Riboli E, Trichopoulou A, Lagiou P, Bamia C, Boutron-Ruault MC, Fagherazzi G, Dartois L, May AM, Peeters PH, Panico S, Johansson M, Wallner B, Palli D, Key TJ, Khaw KT, Ardanaz E, Overvad K, Tjønneland A, Dorronsoro M, Sánchez MJ, Quirós JR, Naccarati A, Tumino R, Boeing H, Gonzalez CA (2015) Healthy lifestyle index and risk of gastric adenocarcinoma in the EPIC cohort study. Int J Cancer 137:598–606
Jiao L, Mitrou PN, Reedy J, Graubard BI, Hollenbeck AR, Schatzkin A, Stolzenberg-Solomon R (2009) A combined healthy lifestyle score and risk of pancreatic cancer in a large cohort study. Arch Intern Med 169:764–770
Arthur R, Kirsh VA, Kreiger N, Rohan T (2018) A healthy lifestyle index and its association with risk of breast, endometrial, and ovarian cancer among Canadian women. Cancer Causes Control 29:485–493
Tabung FK, Steck SE, Burch JB, Chen CF, Zhang H, Hurley TG, Cavicchia P, Alexander M, Shivappa N, Creek KE, Lloyd SC, Hebert JR (2015) A healthy lifestyle index is associated with reduced risk of colorectal adenomatous polyps among non-users of non-steroidal anti-inflammatory drugs. J Prim Prev 36:21–31
Koch M, Borggrefe J, Schlesinger S, Barbaresko J, Groth G, Jacobs G, Lieb W, Laudes M, Müller MJ, Bosy-Westphal A, Heller M, Nöthlings U (2015) Association of a lifestyle index with MRI-determined liver fat content in a general population study. J Epidemiol Community Health 69:732–737
Leong TI, Weiland TJ, Jelinek GA, Simpson S, Brown CR, Neate SL, Taylor KL, O'Kearney E, Milanzi E, de Livera AM (2018) Longitudinal associations of the healthy lifestyle index score with quality of life in people with multiple sclerosis: a prospective cohort study. Front Neurol 9:874
Bhupathiraju SN, Lichtenstein AH, Dawson-Hughes B, Hannan MT, Tucker KL (2013) Adherence to the 2006 American Heart Association Diet and Lifestyle Recommendations for cardiovascular disease risk reduction is associated with bone health in older Puerto Ricans. Am J Clin Nutr 98:1309–1316
Chen GD, Ding D, Tian HY, Zhu YY, Cao WT, Wang C, Chen YM (2017) Adherence to the 2006 American Heart Association’s Diet and Lifestyle Recommendations for cardiovascular disease risk reduction is associated with bone mineral density in older Chinese. Osteoporosis Int 28:1295–1303
Sotos-Prieto M, Bhupathiraju SN, Falcón LM, Gao X, Tucker KL, Mattei J (2015) A healthy lifestyle score is associated with cardiometabolic and neuroendocrine risk factors among Puerto Rican adults. J Nutr 145:1531–1540
Zung WW (1971) A rating instrument for anxiety disorders. Psychosomatics. 12:371–379
Zhang CX, Ho SC (2009) Validity and reproducibility of a food frequency questionnaire among Chinese women in Guangdong province. Asia Pac J Clin Nutr 18:240–250
Fung TT, McCullough ML, Newby PK et al (2005) Diet-quality scores and plasma concentrations of markers of inflammation and endothelial dysfunction. Am J Clin Nutr 82:163–173
Mitrou PN, Kipnis V, Thiébaut AC, Reedy J, Subar AF, Wirfält E, Flood A, Mouw T, Hollenbeck AR, Leitzmann MF, Schatzkin A (2007) Mediterranean dietary pattern and prediction of all-cause mortality in a US population: results from the NIH-AARP Diet and Health Study. Arch Intern Med 167:2461–2468
World Health Organization. Global recommendations on physical activity for health. https://www.who.int/dietphysicalactivity/publications/9789241599979/en/. Accessed 05 May 2020
Chen GD, Dong XW, Zhu YY, Tian HY, He J, Chen YM (2016) Adherence to the Mediterranean diet is associated with a higher BMD in middle-aged and elderly Chinese. Sci Rep 6:25662
Stone Katie L, Seeley Dana G, Li-Yung L, Cauley Jane A, Kristine E, Browner Warren S, Nevitt Michael C, Cummings SR (2003) BMD at multiple sites and risk of fracture of multiple types: long-term results from the Study of Osteoporotic Fractures. J Bone Miner Res Off J Am Soc Bone Miner Res:18
Wu XP, Liao EY, Huang G, Dai RC, Zhang H (2003) A comparison study of the reference curves of bone mineral density at different skeletal sites in native Chinese, Japanese, and American Caucasian women. Calcif Tissue Int 73:122–132
Kuruvilla K, Kenny AM, Raisz LG, Kerstetter JE, Feinn RS, Rajan TV (2011) Importance of bone mineral density measurements in evaluating fragility bone fracture risk in Asian Indian men. Osteoporos Int 22:217–221
Qu X, Zhang X, Zhai Z, Li H, Liu X, Li H, Liu G, Zhu Z, Hao Y, Dai K (2014) Association between physical activity and risk of fracture. J Bone Miner Res 29:202–211
Cosman F, de Beur SJ, LeBoff MS et al (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporosis Int 25:2359–2381 1
Kim SH, Yi SW, Yi JJ, Kim YM, Won YJ (2018) Association between body mass index and the risk of hip fracture by sex and age: a prospective cohort study. J Bone Miner Res 33:1603–1611
Malmir H, Saneei P, Larijani B, Esmaillzadeh A (2018) Adherence to Mediterranean diet in relation to bone mineral density and risk of fracture: a systematic review and meta-analysis of observational studies. Eur J Nutr 57:2147–2160
Hu FB (2002) Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol 13:3–9
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 35 kb)
Rights and permissions
About this article
Cite this article
Deng, Yy., Liu, Yp., Ling, Cw. et al. Higher healthy lifestyle scores are associated with greater bone mineral density in middle-aged and elderly Chinese adults. Arch Osteoporos 15, 129 (2020). https://doi.org/10.1007/s11657-020-00758-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-020-00758-9