Abstract
Summary
We prospectively analyzed 283 women to evaluate the effects of body mass index (BMI) and physical activity levels on bone mineral density (BMD) progression in pre- and postmenopausal women over 2 years. In postmenopausal women, lower BMI was linked with worsening BMD, and moderate activity levels were associated with a lower likelihood of worsening BMD at 2 years.
Purpose
The aim of our study is to evaluate the effects of BMI and physical activity levels on BMD progression in pre- and postmenopausal Asian women over 2 years.
Methods
We prospectively analyzed 283 women from 2006 to 2009. They were divided into two groups (159 pre- and 124 postmenopausal) and analyzed separately to avoid confounding by age and menopausal hormonal status. The mean follow-up period was 771 days. Demographic data was obtained, including medical history, calcium supplementation, BMI, and physical activity levels (IPAQ scale). Bilateral femoral neck BMD was determined at the time of recruitment, 1 year, and after 2 years. Generalized linear modeling was used to evaluate the effects of BMI and physical activity levels on BMD progression over a 2-year period.
Results
Amongst premenopausal women, lower initial femoral neck BMD scores were linked to worsening BMD (p = 0.048). In postmenopausal women, lower BMI was linked with worsening BMD (p = 0.012). Postmenopausal patients with moderate activity levels had a lower likelihood of worsening BMD at 2 years (p = 0.038). High physical activity levels were linked to a lower risk of BMD worsening (p = 0.066).
Conclusions
Higher BMI scores are protective for osteoporosis in postmenopausal women. Moderate levels of physical activity are beneficial for bone health in postmenopausal women, while low physical activity levels are not helpful. We recommend that, in the secondary prevention of osteoporosis, postmenopausal women should be encouraged to participate regularly in moderate physical activities. A practical approach would be walking 30 min a day for at least 5 days per week.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The World Health Organization defines osteoporosis as a progressive systemic skeletal disease characterized by low bone mass and microarchitectural deterioration of bone tissue, with a consequent increase in bone fragility and susceptibility to fracture [1]. Dual energy X-ray absorptiometry (DXA) is a simple, reliable, and reproducible tool used in the assessment of bone mineral density (BMD), and is the gold standard for the diagnosis of osteoporosis at the lumbar spine and hip. A strong association between BMD scores and the probability of fragility fractures is well-documented [2, 3]. Based on the WHO definitions, a T-score > −1 is normal, while T-scores < −1 to > −2.5 indicate osteopenia, and T-scores < −2.5 are diagnostic for osteoporosis [4].
Osteoporosis: dealing with the rising global pandemic
Generally accepted strategies to improve bone health and reduce the incidence of osteoporotic fracture in women aims to (1) maximize peak bone mass during growth in childhood and adolescence, (2) minimize age-related bone loss in middle-aged/premenopausal women, and (3) prevent falls and fractures in older/postmenopausal women.
In our study, we focus on secondary prevention measures to minimize age-related bone loss in the middle-aged population. There is strong evidence that patients who adopt a lifestyle that involves adequate participation in physical activity [5, 6], and avoids significant weight loss [7, 8], are at an advantage with regards to the preservation of bone health over the course of their life.
Body mass index and osteoporosis
Observational studies have shown that body mass index (BMI) is one of the modifiable factors affecting BMD [9, 10]. A higher BMI has been found to be a protective factor for bone density among older subjects, with higher BMD values found among the moderately overweight [11–13]. Patients with higher BMI and weight gain have also been found to exhibit reduced bone loss [14]. This is due to the positive effects of weight-related load on bone density [15]; furthermore, greater muscle mass seems to be associated with higher bone mass, likely due to the increased mechanical stress of muscle on bone [16].
Similarly, low body weight is considered a high risk factor for osteoporosis [17, 18]. Several studies have shown that low body weight and low BMI are associated with low BMD and fractures [19–21]. Older women who experience weight loss in later years have also been found to be at increased risk for bone loss and fractures, irrespective of current weight or intention to lose weight. These findings indicate that even voluntary weight loss in overweight elderly women increases bone loss [22]. So far, no value is agreed on for weight-to-height versus osteoporosis and related fracture risk, but a BMI of 26–28 has been suggested to confer some protection, whereas a slender build with a BMI of 22–24 has been thought to increase risk [23].
Physical activity levels and osteoporosis
Physical activity has long been considered to be a major potentially modifiable factor linked to BMD and fracture risk [24]. Mechanical stimulation from physical activity has been shown to modulate bone remodeling, resulting in increased bone mineralization, periosteal diameter, and cortical thickness [25]. The prevailing biomechanical theory is that mechanical stimuli engender beneficial structural adaptation in bone primarily through local physical forces that deform bone cells [26]. Therefore, physical activities that cause greater mechanical forces would be expected to have greater trophic effects.
There is evidence that regular physical activity minimizes postmenopausal bone loss [21, 27], and prevents falls and fall-related injuries in older people [20]. However, physical capacity has been shown to decline with age; in addition, lower bone density tends to occur together with impaired physical function [28]. Studies have consistently documented that the majority of young women do not engage in adequate physical activity, and rates of activity steadily decrease throughout the life span [29, 30]. Furthermore, it has been found that women are less likely to be active in their later years if they do not have a history of activity in their youth [31]. Consequently, regular physical activity has not been adequately established as a priority in this future generation of older women who are at risk of developing osteoporosis [24]. Thus, public health strategies aimed at improving bone health through the promotion of a practical lifestyle approach to increase physical activity at the population level may help to reduce overall prevalence of osteoporosis and its associated sequelae [32].
The objectives of this prospective observational study are to evaluate the following:
-
1.
The association between body mass index and bone mineral density
-
2.
The association between physical activity levels and bone mineral density
-
3.
To correct for the confounding effects of age and menopausal hormonal status by analyzing the patients in two separate groups—pre- and postmenopausal women
Methods
Setting and data sources
Female patient volunteers were recruited at the Department of Orthopedics, National University Hospital (NUH) in Singapore between 2006 and 2009. The inclusion criteria were (1) premenopausal community ambulant Chinese women aged 45–47 years with regular menses during the preceding 2 years, and (2) postmenopausal community ambulant Chinese women aged 55–60 years with cessation of menses for at least 12 months. Patients were excluded from the study if they had (1) history of metabolic bone disease (e.g., hyperparathyroidism, hyperthyroidism, Cushing's syndrome, osteomalacia, renal failure, and diabetes mellitus), (2) fractures involving the knee joint, (3) inflammatory, infectious, or neuropathic arthropathy, (4) hip or knee arthroplasty, and (5) chronic consumption of alcohol, tobacco, or medications known to affect bone metabolism (including bisphosphonates, estrogen preparations, antiepileptic drugs, corticosteroids, thyroxine, anticoagulants). The usage of calcium supplements was not an exclusion criterion.
The study population was divided into two groups—premenopausal and postmenopausal women. Premenopausal patients were defined as women with regular menses during the 2 years preceding recruitment into the study. Patients were deemed to be postmenopausal if they had cessation of menses for at least 12 months prior to entry into the study. Both groups were analyzed separately to eliminate age and menopausal hormonal status as potential confounders of BMI measurements, physical activity levels, and BMD scores. The study was approved by the NUH ethics committee, and written informed consent was obtained from all patients.
Outcome measurements
Patients were prospectively followed up from the time of entry into the study, at 1 year, and until approximately 2 years post-recruitment. Patients were reviewed by both an orthopedic surgeon and a research coordinator at each follow-up visit. The study participants' age, anthropometric characteristics, and use of calcium supplements were recorded. The BMI was calculated during patient recruitment. All patient height and weight measurements were taken by the same qualified research coordinator using a standardized weighing scale that was calibrated weekly. The physical activity levels of the study participants were assessed at the time of recruitment using the “long last 7 days self-administered format” of the International Physical Activity Questionnaire (IPAQ) [33].
The primary clinical outcome measure was the patients' BMD, and the progression of their BMD scores after 2 years. Bilateral femoral neck BMD was determined using a Norland XR-46 DXA scanner at the time of recruitment, at 1 year, and then at 2 years of follow-up. The precision of bone density measurement is important when the technique is being used to follow changes in bone density over time. In order to validate the technique and determine the reproducibility in BMD measurements, a precision study was performed by a qualified technician. The precision error of femoral neck BMD measurement in the lab was found to be 0.015 g/cm2, and the least significant change (LSC) at the 95 % confidence interval was 4.2 %.
Statistical analysis
Categorical variables are presented as percentages and compared using Pearson's chi-squared test or Fisher's exact test where appropriate. Continuous variables are presented using the mean (± standard deviation), and comparisons were done by utilizing the unpaired t test—the null hypothesis being that there was no association between the tested variable and BMD progression. BMD progression was defined as a worsening of the femoral neck T-score when comparing the first DXA scan at the time of recruitment and the third DXA scan after approximately 2 years, using the LSC as the threshold for difference.
Statistical significance was assumed if p < 0.05. Baseline characteristics were compared between the premenopausal and postmenopausal groups. For both study groups, patient characteristics were also compared between those who exhibited progressively worsening BMD at 2 years versus those patients whose BMD scores did not worsen. A generalized linear regression model was used to examine the relationship between the risk of BMD progression after 2 years with age, calcium supplementation, initial femoral BMD scores, BMI scores, and physical activity levels (low, moderate, and high on the IPAQ scale). This generalized linear model was used to allow for the non-normal distribution of outcomes and to correct for confounding factors. “Generalized estimating equations” were applied to extend the generalized model for application to repeated measures.
Results
The recruited study participants comprised of 283 female patients with a mean age of 50.61 ± 5.66 years-old (SD). There were 159 female patients (45.81 ± SD1.12 years) in the premenopausal group and 124 female patients (56.80 ± SD1.84 years) in the postmenopausal group. The mean follow-up period was 771 days. Seventeen patients in the premenopausal group and 19 patients in the postmenopausal group were lost to follow-up and excluded from the statistical analysis.
The baseline clinical characteristics of both patient groups are shown in Table 1, which includes the BMI scores, use of calcium supplements, level of physical activity, severity of knee osteoarthritis (Kellgren–Lawrence grading), and mean femoral BMD. Statistically significant differences between the pre- and postmenopausal groups included older patients, more usage of calcium supplements, more advanced knee osteoarthritis, and lower initial BMD scores in the postmenopausal group (p < 0.05). There were no statistically significant baseline differences in BMI scores and physical activity levels between both groups at the point of entry into the study.
Premenopausal group
There was a statistically significant association between age and the risk of BMD progression (Table 2). The mean age of those patients whose BMD did not worsen after 2 years was lower as compared to patients whose BMD scores deteriorated (p = 0.016; 95 % CI −0.843, −0.086). However, this is unlikely to be of clinical significance as the mean difference was approximately half a year.
There was no statistical link between BMI scores and the risk of BMD progression in the premenopausal group. There were also no statistically significant associations between worsening BMD and the use of calcium supplements, physical activity levels, knee osteoarthritis severity, or initial mean femoral neck BMD scores.
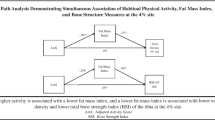
On further linear regression analysis using a generalized linear model to adjust for the level of physical activity, calcium supplement usage, age, and BMI, the mean femoral neck BMD at the time of recruitment was significantly associated with BMD progression, with lower initial BMD scores linked to worsening BMD after 2 years (p = 0.048; 95 % CI 0.007–0.973). On the other hand, BMI scores, age, and levels of physical activity were not found to be significantly related to BMD progression using this model (Table 3).
Postmenopausal group
There was a statistically significant association between the initial mean femoral neck BMD and the risk of BMD progression (Table 4). The mean initial femoral neck BMD of those patients whose BMD did not progress was lower when compared to patients whose BMD scores deteriorated after 2 years (p = 0.006; 95 % CI −0.109, −0.019). There was no statistically significant association between worsening BMD and age, BMI scores, calcium supplement usage, physical activity levels, or knee osteoarthritis severity.
After adjusting for the level of physical activity, calcium supplement usage, age, and BMI using the generalized linear model, the mean femoral neck BMD at the time of recruitment was significantly associated with BMD progression (Table 5). Higher initial BMD scores were linked to worsening BMD after 2 years (p = 0.007; 95 % CI 3.413–163.253).
Similarly, when adjustments had been made for physical activity levels, calcium supplementation, age, and initial femoral neck BMD, it was found that BMI was also significantly associated with BMD progression—patients with lower BMI were linked with worsening BMD at 2 years of follow-up (p = 0.012; 95 % CI 0.792–0.972). However, this is unlikely to be of clinical significance in our study population as the difference in mean BMI between both groups was 0.04 kg/m2.
Using the generalized linear model to adjust for calcium supplement usage, age, BMI, and initial femoral neck BMD, there was a statistically significant relation between moderate physical activity and BMD progression, with patients with moderate activity levels on the IPAQ scale having lower likelihood of worsening BMD at 2 years (p = 0.038; 95 % CI 0.092–0.932). There was also a marked trend towards patients with high levels of physical activity having less risk of BMD progression, although this was statistically nonsignificant (p = 0.066). Notably, there was no statistically significant relationship seen between low physical activity levels and BMD progression (p = 0.688).
Discussion
The main determinants of bone mass have still not been thoroughly elucidated; however, they are thought to include genetic potential, calcium intake, body weight, and physical activity [34, 35]. The latter three factors are potentially modifiable and have been the subject of considerable research interest, although most of the literature involves retrospective observational studies. To the best of the authors' knowledge, we believe that there are no other published longitudinal studies in current literature examining the effects of calcium supplementation, BMI, and physical activity levels on the risk of BMD progression in a population comprising predominantly of Asian pre- and postmenopausal women.
Only a few reports suggested a potential synergy between calcium intake and exercise [36]. However, the results with regard to the relationship between calcium intake, bone mass, and fracture risk were disparate. A meta-analysis showed that calcium intake correlated with the BMD of all areas except in the ulna of postmenopausal women [37]. However, another meta-analysis showed no clear correlation between dietary calcium intake and femoral neck fractures [38]. Thus, the relationship between calcium intake and fractures remains far more elusive than that between calcium intake and BMD. Likewise, our study did not reveal any significant relationship between calcium supplementation and the risk of BMD progression in both pre- and postmenopausal women.
Statistical analysis of the premenopausal women in our study revealed that lower initial femoral neck BMD scores during recruitment was significantly linked to worsening BMD after 2 years. As the average age of patients in this fairly youthful group was 45.8 years, we believe that the initial femoral BMD scores reflect an approximation of the peak bone mass attained by these women. Hence, it is unsurprising that patients in this group who had lower peak bone mass were at higher risk of having worsening BMD scores after 2 years.
On the contrary, in the postmenopausal group, linear regression analysis revealed that higher initial femoral neck BMD scores were statistically linked to worsening BMD after 2 years. While this may seem counterintuitive, this finding may be due in part to the relatively young age (average 56.8 years) of patients from this group. We believe that patients in their 50s may only recently have entered the phase of rapid postmenopausal bone loss, and as such, patients with higher BMD may initially lose more bone mass in this early phase compared to patients with poorer bone stock to begin with. A study with a significantly longer duration of follow-up may help to elucidate the long-term relationship between peak BMD and subsequent postmenopausal bone loss rates.
Generalized linear models of the postmenopausal group revealed that BMI was significantly associated with BMD progression; patients with lower BMI were linked with worsening BMD at 2 years of follow-up (although the clinical significance is questionable due to the small absolute difference in mean BMI levels between both groups). Nonetheless, this is consistent with the findings of most other published studies, which show that increased BMI and obesity are protective for osteoporosis [9–15, 34], while weight loss and a slender body habitus are associated with low BMD scores and fragility fractures [17–21]. Notably, there was no significant association between BMI and BMD in the premenopausal arm of our study.
In the postmenopausal group, there was a statistically significant relationship between moderate physical activity and BMD progression, with patients having moderate activity levels on the IPAQ scale being found to have a lower likelihood of worsening BMD at 2 years. There was also a marked but nonsignificant trend of patients with high levels of physical activity having a lower risk of BMD progression. Lastly, there was no statistical relationship seen between low physical activity levels and BMD progression. Our findings indicate that a moderate physical activity is desirable in maintaining bone health, while postmenopausal women with low physical activity levels may represent an at-risk group for BMD progression and development of osteoporosis. High physical activity levels may also be protective for osteoporosis, with the trend approaching statistical significance (p = 0.066). The lack of statistical significance may have been influenced by the relatively small sample size of high-activity group (36 patients), especially when compared to the moderate-activity group (62 patients). Nonetheless, our findings are congruent with those of multiple observational studies, which have consistently identified weight-bearing physical activities to be beneficial for bone health [20, 24, 27].
Lastly, it should also be noted that guidelines for weight-bearing activity with the aim of promoting bone health have yet to be well established, and this remains an area for future research. At present, the Centers for Disease Control and Prevention and American College of Sports Medicine recommend at least 30 min or more of physical activity, on at least 5 days of the week (∼2.5 h in total) [31].
The strengths of our paper lie in its design as a prospective study, avoiding the biases associated with retrospective study designs. In addition, patient compliance was good, with an acceptable loss to follow-up rate of 12.7 % that was evenly distributed over both study arms. We also avoided the main confounders of age and menopausal hormonal status by dividing our patients into pre- and postmenopausal groups and analyzing them independently, hence correcting for the systemic effects of estrogen on osteoporosis. Furthermore, we have factored in age, calcium supplementation, BMI, physical activity levels, and initial femoral neck BMD scores in the analysis with generalized linear modeling, thereby reducing the impact of these factors on the measured outcomes.
The study employed objective, well-validated measures for the primary outcomes under investigation. Height and weight measurements for BMI computation were taken using the same instruments by the same qualified research coordinator for all patients in both groups. The weighing scale was regularly calibrated by trained personnel. Femoral neck BMD measurements were taken by the same qualified technician using a regularly calibrated Norland XR-46 DXA scanner with a precision error in femoral neck BMD measurement of 0.015 g/cm2.
Physical activity levels were evaluated using the “long last 7 days self-administered format” of the IPAQ. IPAQ is a well-studied measure of physical activity. Studies have found IPAQ to have acceptable validity for monitoring population levels and patterns of physical activity among 18–65-year-old adults in diverse settings; the short IPAQ form “last 7 day recall” has been recommended for national monitoring, with the long IPAQ form being utilized for research that requires more detailed assessment [39].
It is well-known that leisure time physical activity (e.g., sports, recreational exercise) is associated with higher BMD in both premenopausal [40] and postmenopausal [41] women. In addition, increased home physical activity (e.g., housework) has been found by Greendale et al. to be associated with higher BMD at the spine and femoral neck [41]. It was also observed that both sport and home activity are independently related to BMD in a dose-dependent manner, substantiating prior evidence that a threshold of high-level activity is not required to stimulate bone accretion [42]. Also, compared with men, women are much more likely to engage in household and family care activities and much less likely to participate regularly in sports or other leisure-time exercise [43]. Thus, physical activity scales that focus solely on leisure activity will seriously underestimate physical activity among women and thereby may miss important associations between physical activity and health outcomes. The long form IPAQ questionnaire comprises 27 questions across 5 domains as follows: (1) job-related, (2) transportation, (3) housework, (4) recreation/sports, and (5) time spent sitting; hence the IPAQ questionnaire provides a comprehensive framework for the evaluation of physical activity levels in both pre- and postmenopausal women.
Limitations of our study include, most notably, the short follow-up period with a mean of only 771 days. As such, the mid-term and long-term effects of BMI and physical activity on BMD progression remain unknown. We are, hence, unable to confirm if moderate physical activity will continue to have protective effects on BMD progression in the long term. As previously noted, a study with a longer follow-up period is also needed to further evaluate the relationship between peak femoral BMD and subsequent rates of bone loss and BMD progression.
Furthermore, although prospective data on BMD changes were studied, BMI and physical activity levels were only assessed at the time of patient enrolment. As such, we do not have data with regards to the change in BMI and physical activity levels in both groups over the course of the study, and this could be a potential confounder. Additionally, there is no data on the use of oral contraceptive pills (OCP) and hormone replacement therapy (HRT), which could alter the sex steroid hormonal status of patients in both study arms. There was also incomplete data on the dosage and types of calcium supplements used by patients. Notably, this study involved only women; hence our findings cannot be reliably extrapolated to include the male population. Lastly, evaluation of physical activity levels using the self-administered IPAQ questionnaire has the drawback of being subject to recall bias.
As such, future studies would be needed to address these limitations, with recommendations for (1) designing a study with a longer follow-up period of 5–10 years, (2) more extensive data collection with regards to patient medical background (including OCP or HRT use, as well as the type and dosage of calcium supplementation), and (3) prospective collection of data on BMI and physical activity levels, in addition to BMD scores. In addition, utilizing an objective measurement of physical activity levels would be a natural approach in further studies.
Conclusion
Based on the results of our study, we have achieved the objectives outlined previously. Higher BMI scores are protective for osteoporosis in postmenopausal women. In addition, moderate levels of physical activity are beneficial for bone health in this group of women; on the other hand, low physical activity levels have not been found helpful in averting a decline in BMD. From these findings, it is apparent that postmenopausal women should be encouraged to participate regularly in at least moderate levels of physical activity as an integral component in the secondary prevention of osteoporosis and fragility fractures. Based on the IPAQ guidelines, this would correlate with a level of activity equivalent to “half an hour of at least moderate-intensity physical activity on most days” (at least 600 MET-min/week).
In practical terms, we would recommend promoting a regular regimen of at least moderate exercise. According to the IPAQ guidelines, this could comprise either (1) three or more days of vigorous-intensity activity of at least 20 min per day, or (2) five or more days of moderate-intensity activity (e.g., walking at least 30 min per day).
References
Consensus development conference: prophylaxis and treatment of osteoporosis. Am J Med. 1991 Jan;90(1):107–10.
Johnell O, Kanis JA, Oden A et al (2005) Predictive value of BMD for hip and other fractures. J Bone Miner Res 20(7):1185–1194
Marshall D, Johnell O, Wedel H (1996) Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ 312(7041):1254–1259
Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organ Tech Rep Ser. 1994;843:1–129
Gardner MM, Robertson MC, Campbell AJ (2000) Exercise in preventing falls and fall related injuries in older people: a review of randomized controlled trials. Br J Sports Med 34(1):7–17
Wallace BA, Cumming RG (2000) Systematic review of randomized trials of the effect of exercise on bone mass in pre- and postmenopausal women. Calcif Tissue Int 67(1):10–18
Hannan MT, Felson DT, Dawson-Hughes B et al (2000) Risk factors for longitudinal bone loss in elderly men and women: the Framingham Osteoporosis Study. J Bone Miner Res 15(4):710–720
De Laet C, Kanis JA, Oden A et al (2005) Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int 16(11):1330–1338
Cetin A, Gokce-Kutsal Y, Celiker R (2001) Predictors of bone mineral density in healthy males. Rheumatol Int 21:85–88
Kenny AM, Prestwood KM, Marcello KM, Raisz LG (2000) Determinants of bone density in healthy older men with low testosterone levels. J Gerontol A Biol Sci Med Sci 55:M492–M497
Barrera G, Bunout D, Gattas V, de la Maza MP, Leiva L, Hirsch S (2004) A high body mass index protects against femoral neck osteoporosis in healthy elderly subjects. Nutrition 20:769–771
Kirchengast S, Peterson B, Hauser G, Knogler W (2001) Body composition characteristics are associated with the bone density of the proximal femur end in middle- and old-aged women and men. Maturitas 39:133–145
Kirchengast S, Knogler W, Hauser G (2002) Protective effect of moderate overweight on bone density of the hip joint in elderly and old Austrians. Anthropol Anz 60:187–197
Heaney R, BargerLux M, Davies K, Ryan R, Johnson M, Gong G (1997) Bone dimensional change with age: interactions of genetic, hormonal, and body size variables. Osteoporos Int 7:426–431
Felson DT, Hannan MT, Anderson JJ (1993) Effects of weight and body mass index on bone mineral density in men and women: the Framingham Study. J Bone Min Res 8:567–573
Sandler RB (1988) Muscle strength and skeletal competence: implications for early prophylaxis. Calcif Tissue Int 42:281–283
Espallargues M, Sampietro-Colom L, Estrada MD, Sola M, del Rio L, Setoain J, Granados A (2001) Identifying bone-mass related risk factors for fracture to guide bone densitometry measurements: a systematic review of the literature. Osteoporos Int 12:811–822
Mazess RB, Barden HS (1991) Bone density in premenopausal women: effects of age, dietary intake, physical activity, smoking, and birth-control pills. Am J Clin Nutr 53:132–142
van der Voort DJ, Geusens PP, Dinant GJ (2001) Risk factors for osteoporosis related to their outcome: fractures. Osteoporos Int 12:630–638
Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE (1995) Risk factors for hip fracture in white women. N Engl J Med 332:767–773
Farahmand BY, Michaelsson K, Baron JA, Persson PG, Ljunghall S (2003) Body size and hip fracture risk. Swedish Hip Fracture Study Group. Epidemiology 11:214–219
Ensrud KE, Ewing SK, Stone KL, Cauley JA, Bowman PJ, Cummings SR (2003) Intentional and unintentional weight loss increase bone loss and hip fracture risk in older women. J Am Geriatr Soc 51:1740–1747
Wardlaw G (1996) Putting body weight and osteoporosis into perspective. Am J Clin Nutr 63:433S–436S
Kohrt WM, Bloomfield SA, Little KD, Nelson ME, Yingling VR (2004) American College of Sports Medicine Position Stand: physical activity and bone health. Med Sci Sports Exerc 36(11):1985–1996
Robling AG, Castillo AB, Turner CH (2006) Biomechanical and molecular regulation of bone remodeling. Annu Rev Biomed Eng 8:455–498
McLeod KJ, Rubin CT, Otter MW, Qin YX (1998) Skeletal cell stresses and bone adaptation. Am J Med Sci 316:176–183
Pines A, Berry EM (2007) Exercise in the menopause—an update. Climacteric 10(suppl 2):42–46
Aoyagi K, Ross PD, Hayashi T, Okano K, Moji K, Sasayama H, Yahata Y, Takemoto T (2000) Calcaneus bone mineral density is lower among men and women with lower physical performance. Calcif Tissue Int 67:106–110
NIH Consensus Conference. Physical activity and cardiovascular health. JAMA 1996;276:241
Pate RR, Pratt M, Blair SN et al (1996) Physical activity and public health. JAMA 276:402
Dishman RK, Sallis JF (1994) Determinants and interventions for physical activity and exercise. In: Bouchard C, Shepard RJ, eds. Physical activity, fitness and health: International proceedings and consensus statement. Champaign, IL: Human Kinetics, 214.
World Health Organization (2009) Global health risks report: mortality and burden of disease attributable to selected major risks. WHO, Geneva.
Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, Oja P (2003) International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 35(8):1381–1395
Pocock NA, Eisman JA, Hopper JL, Yeates MG, Sambrook PN, Eberl S (1987) Genetic determinants of bone mass in adults: a twin study. J Clin Invest 80:706–710
Slemenda CW, Miller JZ, Hui SL, Reister TK, Johnston CC (1991) Role of physical activity in the development of skeletal mass in children. J Bone Miner Res 6:1227–1233
Devine A, Dhaliwal SS, Dick IM, Bollerslev J, Prince RL (2004) Physical activity and calcium consumption are important determinants of lower limb bone mass in older women. J Bone Miner Res 19:1634–1639
Welten DC, Kemper HCG, Post GB, van Staveren WA (1995) A meta-analysis of the effect of calcium intake on bone mass in young and middle-aged females and males. J Nutr 125:2802–2813
Xu L, McElduff P, D’Este C, Attia J (2004) Does dietary calcium have a protective effect on bone fracture in women? A meta-analysis of observational studies. Br J Nutr 91:625–634
Hagströmer M, Oja P, Sjöström M (2006) The International Physical Activity Questionnaire (IPAQ): a study of concurrent and construct validity. Public Health Nutr 9(6):755–762
Rubin LA, Hawker GA, Peltekova VD, Fielding LJ, Ridout R, Cole DEC (1999) Determinants of peak bone mass: clinical and genetic analyses in a young female Canadian cohort. J Bone Miner Res 14:633–643
Greendale GA, Barrett-Connor E, Edelstein S, Ingles S, Haile R (1995) Lifetime leisure exercise and osteoporosis. Am J Epidemiol 141:951–959
Greendale GA, Huang MH, Wang Y, Finkelstein JS, Danielson ME, Sternfeld B (2003) Sport and home physical activity are independently associated with bone density. Med Sci Sports Exerc 35(3):506–512
Ainsworth BE, Leon AS (1993) Gender differences in self-reported physical activity. Women Sport Phys Act J 23:1–16
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wee, J., Sng, B.Y.J., Shen, L. et al. The relationship between body mass index and physical activity levels in relation to bone mineral density in premenopausal and postmenopausal women. Arch Osteoporos 8, 162 (2013). https://doi.org/10.1007/s11657-013-0162-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-013-0162-z