Abstract
Summary
Potential FRAX®-based major osteoporotic fracture (MOF) and hip fracture (HF) intervention thresholds (ITs) for postmenopausal Singaporean women were explored. Age-dependent ethnic-specific and weighted mean ITs progressively increased with increasing age. Fixed ITs were derived via discriminatory value analysis. MOF and HF ITs with highest the Youden index were chosen as optimal.
Introduction
We aimed to explore FRAX®-based intervention thresholds (ITs) to potentially guide osteoporosis treatment in Singapore, a multi-ethnic nation.
Method
One thousand and one Singaporean postmenopausal community-dwelling women belonging to Chinese, Malay and Indian ethnicities underwent clinical risk factor (CRF) and BMD assessment. FRAX® major osteoporotic fracture (MOF) and hip fracture (HF) probabilities were calculated using ethnic-specific models. We employed the translational logic adopted by NOGG (UK), whereby osteoporosis treatment is recommended to any postmenopausal woman whose fracture probability based on other CRFs is similar to or exceeds that of an age-matched woman with a fracture. Using the same logic, ethnic-specific and mean weighted age-dependent ITs were computed. Employing these age-dependent ITs as a reference, the performance of fixed (age-independent) ITs were examined using ROC curves and discriminatory analysis, with the highest Youden index (YI) (sensitivity + specificity − 1) used to identify the optimal MOF and HF ITs.
Results
The mean age was 58.9 (6.9) years. Seven hundred and eighty-nine (79%) women were Chinese, 136 (13.5%) Indian and 76 (7.5%) Malay. Age-dependent MOF ITs ranged from 3.1 to 33%, 2.5 to 17% and 2.5 to 16% whilst HF ITs ranged from 0.7 to 17%, 0.4 to 6% and 0.4 to 6.3% in Chinese, Malay and Indian women, respectively, between the ages of 50 and 90 years. The weighted age-dependent MOF and HF ITs ranged from 2.9% and 0.6%, respectively, at the age of 50, to 28% and 14% at 90 years of age. Fixed MOF/HF ITs of 5.5%/1%, 2.5%/1% and 2.5%/0.25% were identified as the most optimal by the highest YI in Chinese, Malay and Indian women, respectively. Fixed MOFP and HF ITs of 4% and 1%, respectively, were found to be most optimal on the weighted means analysis.
Conclusion
The ITs for osteoporosis treatment in Singapore show marked variations across ethnicities. Weighted mean thresholds may overcome the dilemma of intervening at different thresholds for different ethnicities. Choosing fixed ITs may have to involve trade-offs between sensitivity and specificity. FRAX®-based age-dependent or the fixed intervention thresholds suggested as an alternative to be considered for use in Singapore though further studies on the societal and health economic impacts of choosing these thresholds in Singapore are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is characterised by low bone mass, microarchitectural deterioration of the skeleton and increased skeletal fragility resulting in an increased risk of fracture. In 1994, a working group of the World Health Organization (WHO) defined osteoporosis as a bone mineral density (BMD) at the lumbar spine, total hip or femoral neck that is 2.5 standard deviations or more below the young adult female mean [1]. This operational definition, aimed originally to facilitate epidemiological study of the disease, subsequently evolved into the clinical and diagnostic definition of osteoporosis. It has been recognised more recently that the inclusion of clinical risk factors enhances the performance of BMD in predicting fractures [2]. Several clinical risk scores have been published in recent years for estimating absolute fracture risk over fixed time periods [3]. FRAX® is an algorithm that computes 10-year fracture probabilities of major osteoporotic fractures (MOF) of the wrist, hip, humerus and spine or of hip fractures (HF) alone based on clinical risk factors with or without BMD input [2]. It was launched in 2008 and it was based on data generated by the World Health Organization (WHO) Collaborating Centre for Metabolic Bone Diseases (1991–2010) at the University of Sheffield.
Most treatment guidelines around the world concur on recommending medical treatment to postmenopausal women and older men who have a history of a prior fragility fracture especially that of the hip or spine [4, 5]. The WHO diagnostic criteria for osteoporosis, i.e. a T-score of − 2.5 or less, also serves as a threshold to guide decisions for instituting treatment in some guidelines [6]. However, epidemiological data consistently demonstrate that approximately half of women who fracture are not osteoporotic by BMD criteria [7] and evidence now suggests that intervention thresholds should be based on absolute risk of fracture, rather than solely on diagnostic thresholds based on BMD [8]. A strategy that incorporates clinical risk factors into the decision-making process may help identify patients who would have been otherwise missed and precluded from being offered treatment as well as serve to avoid treatment in low-risk individuals. Women at high risk of hip fracture based on FRAX® probability have been shown to be responsive to appropriate osteoporosis management [9] and response to pharmaceutical intervention also may be greater among women with higher probability of fracture [10].
Several osteoporosis management guidelines around the world now agree that anti-osteoporosis treatment should be offered to patients who have a FRAX®-derived fracture probability above a certain treatment threshold [11, 12]. Whether the ideal treatment threshold should be a fixed one [11,12,13] encompassing all ages, age-dependent [14] or a hybrid of the two [15] is unclear. Globally, countries have adopted different methods of deriving FRAX®-based intervention thresholds. It has been derived through cost-effectiveness analysis in Switzerland and in the USA [11, 13], translational logic in the UK [14], discriminatory value analysis in Hong Kong and in Sri Lanka [16, 17], or in Japan by aligning it with recommendations prior to the advent of FRAX [18]. It is unclear which approach is best.
Singapore is an island nation in SE Asia with a multi-ethnic population of 5.6 million people (https://www.moh.gov.sg/content/moh_web/home/statistics/Health_Facts_Singapore/Population_And_Vital_Statistics; last accessed August 15, 2018). Unlike other countries in South East Asia, dual X-ray absorptiometry (DXA) scanning for the measurement of BMD is easily available in Singapore, with 16.9 DXA machines currently in use per one million populations (https://iofbonehealth.org/data-publications/regional-audits/asia-pacific-regional-audit). At the time of publication of the Singapore Clinical Practice Guidelines (CPG) for Osteoporosis in 2009, FRAX® models for Singapore were not yet available. Ethnic-specific, Chinese, Malay and Indian FRAX® models for Singapore subsequently became available in December 2010, but to date, no specific intervention thresholds to guide treatment of osteoporosis based either on FRAX® or other available fracture risk calculators have been provided in Singapore. Though the CPG recommended that, after secondary contributors to bone loss are excluded, treatment be offered to patients with fragility fractures of the vertebrae, hip, pelvis, humerus or wrist, management of the osteopenic or osteoporotic patient without fragility fractures is less clear and there exists no consensus as to what thresholds to intervene with anti-osteoporosis agents. In a questionnaire-based survey that was conducted in 2012 among health care providers in the Asia Pacific including those from Singapore, clinicians had expressed a strong desire to have country-specific FRAX® models and a willingness to commit to treating patients with osteoporosis if they were provided guidance on intervention thresholds to use [19]. The aim of the current study was to explore FRAX®-based intervention thresholds that could potentially be considered for the management of osteoporosis in postmenopausal Singaporean women.
Method
Study population
The study sample was derived from women seen consecutively from January 1, 2014 to June 30, 2017 at the outpatient bone clinics of Singapore General Hospital and had a DXA scan done as part of work-up for osteopenia and osteoporosis (n = 400), women who had a DXA scan done during the same period as part of routine general health screening at the same institution (n = 200), and a cohort of 1201 well women, recruited into the Integrated Women’s Health Programme (IWHP) cohort study at the National University Hospital, Singapore. Details of this cohort have been published previously [20]. Institutional review board approval was obtained for this retrospective review.
Subjects were excluded from the study if they were premenopausal or had ever been treated for osteoporosis. Subjects who had incomplete baseline socio-demographic information, medical, menstrual, fracture, smoking, alcohol and medical history and laboratory data were also excluded from the final analysis as were subjects with uninterpretable DXA scans of the hip and lumbar vertebrae. BMD at the hip and lumbar spine (L1–L4) was measured by DXA (Hologic QDR 4500, Hologic Inc., Bedford, MA, USA). A subject was considered as having osteopenia or osteoporosis if the lowest T-score at any of three axial sites, viz. the neck of femur, total hip or lumbar spine (L1–L4), was between − 1 and − 2.5 or ≤ − 2.5, respectively. Female, ethnic-specific Singaporean reference database was used to calculate the T-scores [21]. The final data set for analysis comprised 1001 postmenopausal women.
FRAX® probabilities
Women belonging to the three ethnicities in the study population had their MOF and HF probabilities calculated based on their clinical risk factors and femoral neck BMD, using ethnic-specific Singapore FRAX® models (https://www.sheffield.ac.uk/FRAX/ Web version 4.0).
Determining intervention thresholds
Age-dependent thresholds
We first estimated age-dependent intervention thresholds using the translational logic adopted by the National Osteoporosis Guideline Group (NOGG) of the UK in that osteoporosis treatment should be offered to any postmenopausal woman without a fracture but whose fracture probability based on other clinical risk factors is similar to or exceeds that of an age-matched woman who has already sustained a fracture. We therefore calculated age-dependent fracture probabilities for both MOF and HF, separately for postmenopausal Chinese, Malay and Indian women for each year between the ages of 50 and 90 years, using the relevant ethnic-specific Singapore FRAX® models and considering that they have no clinical risk factors apart from a previous fragility fracture. For the Chinese women, we calculated the FRAX® thresholds using a mean BMI of 22.7 kg/m2 and for the Indian and Malay women, the mean BMIs of 27.1 kg/m2 and 27.5 kg/m2, respectively, were used. These values were adapted from published data [22] and existent population data from the National Health Surveillance Survey 2012 (https://www.moh.gov.sg/content/moh_web/home/pressRoom/pressRoomItemRelease/2012/national_health_surveillancesurvey2012). In addition, we calculated the mean Singaporean age-dependent thresholds for MOF and HF using the age-dependent values for all three ethnicities, weighted by the proportion of Chinese, Malays and Indians in the Singapore population; these were 74.3%, 13.4%% and 9.1%, respectively (https://www.moh.gov.sg/content/moh_web/home/statistics/Health_Facts_Singapore/Population_And_Vital_Statistics, last accessed August 15, 2018).
Fixed intervention thresholds
In the absence of a gold standard intervention threshold and given the logic behind the adoption of age-dependent thresholds, we decided to use the latter as a reference point and to determine the ability of fixed thresholds to provide similar performance to the age-dependent thresholds. Thus, women in the study population with probabilities at or above the age-dependent thresholds for MOF or HF were classified as being at high risk, whilst those below the thresholds were classified as low risk. This classification was conducted using the thresholds that were specific to each ethnicity but was also done using the weighted Singaporean mean age-dependent thresholds described above.
Receiver operating characteristic (ROC) curves were constructed with the risk category (high or low) as the state variable and fixed major osteoporotic and hip fracture probabilities as the test variables, and the area under the ROC curve (AUC) and its 95% confidence interval (CI) were estimated. We used the Youden index(Sensitivity + Specificity − 1) in establishing the optimal threshold point from the ROC data [23, 24].
All statistical analyses were performed using SPSS Version 17.0 (SPSS Inc., Chicago, IL, USA) and p < 0.05 was taken as the level of statistical significance.
Results
The majority (n = 789, 79%) of the study population were Chinese, 136 (13.5%) were Indian and 76 (7.5%) were Malay. The mean (SD) age of the entire cohort was 58.9 (6.9) years. It was 60 (6.8) years in the Chinese women, 55 (5.9) in the Malay and 56 (6.6) years in the Indian women. Forty-two percent of the subjects were between the ages of 50 and 59, 33% were between the ages of 60 and 69, 20% were between the ages of 70 and 79 and 5% were older than 80. The mean (SD) BMI was 23.6 (4.3) kg/m2, with a lower mean BMI (22.7 (3.6) kg/m2) in the Chinese women, compared to women of Malay (27.8 (4.5) kg/m2) or Indian ethnicity (27.1 (4.7) kg/m2). Sixty (6%) of the women had a history of prior fragility fractures. Only 2% of the population had ever consumed alcohol and only 1% reported a history of current or past smoking. On axial DXA scanning, 470 (46.7%) of the women had normal BMD whilst 290 (29.1%) had osteopenia and 240 (24.1%) had osteoporosis as defined earlier.
Intervention thresholds
Age-dependent thresholds
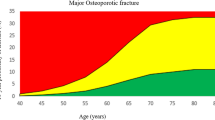
Age-dependent MOF threshold values varied from 3.1 to 33% in Chinese women, 2.5 to 17% in Indian women and 2.5 to 16% in Malay women between the ages of 50 and 90 years (Fig. 1). Age-dependent ethnic-specific hip fracture probabilities varied from 0.7 to 17%, 0.4 to 6% and 0.4 to 6.3% in Chinese, Indian and Malay women aged 50–90, respectively (Fig. 1). The mean weighted age-dependent MOF thresholds varied from 2.9 to 28% whilst those for hip fracture varied from 0.6 to 14% between the ages of 50 and 90 years (Fig. 1).
One hundred and forty-seven out of seven hundred and eighty-nine (18.6%) and 173/789 (22%) of the Chinese women had fracture probabilities above the MOF or HF ethnic-specific and weighted age-dependent ITs. For the Malay women, these proportions were 9/76 (11.8%) and 3/76 (3.9%), respectively, and for the Indian women, they were 18/136 (13.2%) and 13/136 (9.5%), respectively.
Fixed intervention thresholds
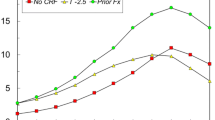
The AUCs of the ROC analyses for MOF and HF probabilities were highly significant within each ethnicity and within the study population as a whole (Table 1). The ROC curves for MOF and HF thresholds in the Chinese women who formed the largest proportion of the study population are shown in Fig. 2.
The sensitivities, specificities, positive predictive value, negative predictive value and the Youden indices of different fixed MOF and HF ITs of Chinese, Malay and Indian women are shown in Table 2. In the Chinese women, a MOF IT of 5.5% and an HF IT of 1% yielded the highest Youden indices. For Malay women, a MOF IT of 2.5% and HF IT threshold of 1% had the highest Youden indices and for Indian women, the MOF and HF thresholds that had the highest Youden indices were 2.5% and 0.25%, respectively.
The sensitivities, specificities, positive predictive values (PPVs), negative predictive values (NPVs) and the Youden indices of variously fixed thresholds derived from the weighted mean age-dependent thresholds of the entire population (viz. that inclusive of all three ethnicities) are shown in Table 3. A major osteoporotic fracture probability (MOFP) IT of 4% and an HFP IT of 1% had the highest Youden index in the population studied.
When a subgroup analysis dividing the largest cohort, viz. the Chinese into < 65 years of age and ≥ 65 years, was performed, a MOF threshold of 4% had the highest Youden index in those under the age of 65 years. The corresponding fixed HF IT with the highest Youden index was 0.75%. In Chinese women aged 65 years and over, a fixed MOF probability IT of 11% had the highest Youden index. The corresponding HF IT with the highest Youden index was 6% (Table 4).
When a subgroup analysis by age of the entire cohort was done, in the women below 65 years of age, a MOFP threshold of 4.5% offered sensitivities and specificities of 66% and 84%, respectively. An HFP threshold of 1.5% yielded sensitivities and specificities of 66% and 91%, respectively, in this age group. In the 65 years and older women, a MOFP threshold of 12.5% and HFP of 5.25% had the highest Youden index with sensitivities of 93% for both MOFP and HFP thresholds and specificities of 84% and 89%, respectively.
Discussion
This study is the first to explore different approaches for defining FRAX®-based intervention thresholds above which anti-osteoporosis drug treatment might be recommended for postmenopausal women in Singapore. As expected, age-dependent intervention thresholds varied considerably with progression of age from 50 to 90 years in women of all three ethnicities with MOF IT values, for instance, varying from 3.1%, 2.5% and 2.5% at age 50 to 33%, 17% and 16% at age 90 in the Chinese, Indian and Malay women, respectively. One potential concern associated with age-dependent intervention thresholds is that, in the absence of a prior fracture, high values of fracture risk need to be reached at older ages before treatment would be considered. Such considerations underpinned the decision by NOGG to set a plateau for fracture risk from the age of 70 years upwards in the UK [25]. The alternative to this might be to consider the use of fixed (i.e. age-independent) intervention thresholds, though these also have potential shortcomings as they can preclude treatment for younger postmenopausal women and mandate that intervention be done for a significant majority of older individuals, depending on the chosen threshold [26].
It is inevitable that trade-offs between sensitivity and specificity will be encountered when determining cut-off values for an intervention threshold by discriminatory value analysis. The Youden index used here gives equal weight to sensitivity and specificity, but when considering intervention thresholds to be recommended for clinical practice, a decision may have to be made as to whether sensitivity or specificity is more important. Thus, it might be preferable to have a slightly higher specificity at the expense of lower sensitivity to avoid overtreatment of people at lower risk. Choosing a threshold that affords higher specificitymight afford a good compromise between over treatment of those at low fracture riskwhile at the same time enable intervention in the older person who is likely to be at higher risk. For example, in the Chinese women, if a MOF threshold of 6.5% is chosen instead of the 5.5% identified through the discriminatory value analysis, sensitivity decreases slightly whereas specificity increases from 71 to 77%. Similarly, whilst an HFP threshold of 1% was identified as most optimal from the discriminatory value analysis in the Chinese women, choosing a cut-off point of 1.5% or even 2% still affords reasonable trade-offs between sensitivities and specificities and could be considered as practical alternatives to be recommended in clinical practice.
Whether lower intervention thresholds in Malay and Indian patients are justified is a philosophical matter for debate. In our study, the fixed MOF IT obtained from the discriminatory value analysis in the Malays and Indians was 2.5%, much lower than that in the Chinese women in whom it was 5.5%. With the use of the fixed ethnic-specific MOF and HF thresholds obtained from this study, it is estimated that very similar proportions of the three ethnicities (33%, 27% and 34% of the Chinese, Malay and Indian women, respectively) would have treatment indicated despite well-documented differences in fracture risk between the three ethnicities in Singapore [27].
There could therefore be an argument for having a weighted threshold (be it age-dependent or fixed) based on the mix of the Singaporean population rather than ethnic-specific thresholds. For example, if the fixed thresholds obtained using the weighted means from our study were employed, then 37%, 13% and 12% of Chinese, Malay and Indian women, respectively, would merit treatment. This approach would translate into a lesser number of women in the ethnicities at lower risk requiring treatment. The decision to use ethnic-specific thresholds would have been reasonable if there is good evidence that effectiveness and cost-effectiveness of intervention at a particular level of risk differs between ethnicities. In the absence of such evidence, it would be reasonable to consider the use of the same intervention threshold irrespective of ethnicity until proven incorrect. However, conceptually, at the individual level, informing a person of a particular ethnicity that she need not have treatment based on the lower risk in general of her ethnicity could be problematic. This matter will have to be accorded grave importance by guidelines formulating groups and policymakers and decisions on whether ethnic-specific or mean weighted thresholds be used will have to be made after healthy debate.
The use of a unified threshold for all ethnicities raises points that can also apply to gender. On the one hand, it can be argued that, since effectiveness [28] and cost-effectiveness [11, 13] of intervention in men are broadly similar to that in women for equivalent risk, the same intervention thresholds can be applied to men. On the other hand, higher levels of evidence exist for fracture risk reduction in women with a diagnosis of osteoporosis and/or prevalent fractures. The evidence is lower for the benefits and risks of long-term treatment for other populations, including men [29, 30]. The issue of deciding upon intervention thresholds in Singaporean men merits further research.
Our study population had women ranging in age from 50 to 90 years. Finding fixed ITs to replicate the performance of age-dependent ITs across such a wide age range is a tough goal. This could be the reason behind the low PPVs for the fixed MOF and HF ITs obtained in our analysis. As was seen, however, the performance characteristics somewhat improved when fixed thresholds were determined for instance in the Chinese women when they were divided by age into those above and below 65 years of age. This could be considered as a modified age-dependent threshold approach. We identified a MOF IT of 4% performing best in Chinese women who were below 65 years of age. In the women aged 65 and above, a MOF IT of 11% had the best performance. These thresholds had much higher PPVs than observed when a single IT threshold across the entire age span was considered. There is however an inherent imperfection in strategies which employ arbitrary and abrupt age cut-offs where the threshold for intervention can dramatically increase on the relevant birthday with little else changing. This can potentially be avoided if age-dependent thresholds are considered or narrower age bands (e.g. 10-year spans) are studied. Our study population however had too few subjects who could be classified as high versus low risk within such narrow age bands for the latter to be done.
To derive intervention thresholds for a given population, multiple factors should be taken into consideration including health economic issues. Costs of DXA scanning, consultations with the health care provider, medications, efficacy of such medications to reduce fractures and the threshold of cost-effectiveness at which intervention is considered appropriate or willingness to pay (WTP) all have to be taken into consideration when performing such health economic analysis [31]. This of course has to be balanced with the potential of rare but significant side effects from long-term use of potent anti-osteoporosis medications [32]. In the approach used by the NOGG of the UK, the relationship between cost-effectiveness and fracture probability used the source data from a prior publication that examined the cost-effectiveness of generic alendronate in the UK. Treatment was found to be cost-effective at all ages when the 10-year probability of a major fracture exceeded 7% [14].
Despite its few limitations including lack of cost-effectiveness analysis, the relatively small number of non-Chinese women in the study population and its non-prospective nature with the resultant inability to assess causal correlations, our study has several advantages. It is the first such study aimed at determining FRAX®-based intervention thresholds for osteoporosis management in Singapore. Though the study population was not randomly recruited from the community, we had the advantage of having two large cohorts from the two largest hospitals from the two health care clusters in Singapore that cover most of the population of Singapore. There were more than adequate numbers of normal women who had presented for general health screening as well as women with densitometrically diagnosed osteoporosis and osteopenia as would be found in the general population. All subjects had complete clinical risk factor assessment performed and data on the subjects gathered through the questionnaire in the clinics was then cross-checked via the electronic health record thereby minimising the issue of recall bias. All subjects had complete laboratory work either as part of routine clinical care or if they were part of the IWHP cohort, as part of the study protocol.
Conclusion
Early identification is key to appropriate management of osteoporosis and to prevent its devastating complication of fragility fractures. Strategies that only target patients with prior fragility fractures are unlikely to reduce the significant osteoporotic fracture burden. Development of country-specific intervention thresholds based on local fracture probabilities that incorporate meaningful clinical risk factors into the management algorithm with clear rationale and logic behind the reason for recommending such thresholds is essential. FRAX®-based age-dependent or the fixed intervention thresholds suggested as an alternative to be considered for use in Singapore. It is hoped that the thresholds identified from this study will be used as a base for further discussions and debate and subsequently adapted for use in Singapore. However, the clinical, societal and health economic impact of choosing these thresholds requires further study.
References
Assessment of fracture risk and its application to screening for postmenopausal osteoporosis (1994) Report of a WHO Study Group. World Health Organ Tech Rep Ser 843:1–129
Kanis JA, Oden A, Johnell O, Johansson H, De Laet C, Brown J et al (2007) The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int 18(8):1033–1046. https://doi.org/10.1007/s00198-007-0343-y
Marques A, Ferreira RJO, Santos E, Loza E, Carmona L, da Silva JAP et al (2015) The accuracy of osteoporotic fracture risk prediction tools: a systematic review and meta-analysis. Ann Rheum Dis 74(11):1958–1967. https://doi.org/10.1136/annrheumdis-2015-207907
Compston J, Cooper A, Cooper C, Gittoes N, Gregson C, Harvey N et al (2017) UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos 12(1):43
Camacho PM, Petak SM, Binkley N, Clarke BL, Harris ST, Hurley DL, Kleerekoper M, Lewiecki EM, Miller PD, Narula HS, Pessah-Pollack R, Tangpricha V, Wimalawansa SJ, Watts NB (2016) American association of clinical endocrinologists and American college of endocrinology clinical practice guidelines for the Diagnosis and treatment of postmenopausal osteoporosis - 2016. Endocr Pract 22(Suppl 4):1–42. https://doi.org/10.4158/EP161435.GL
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S et al (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25(10):2359–2381. https://doi.org/10.1007/s00198-014-2794-2
Wainwright SA, Marshall LM, Ensrud KE, Cauley JA, Black DM, Hillier TA, Hochberg MC, Vogt MT, Orwoll ES (2005) Hip fracture in women without osteoporosis. J Clin Endocrinol Metab 90(5):2787–2793. https://doi.org/10.1210/jc.2004-1568
Kanis JA, Borgstrom F, De Laet C, Johansson H, Johnell O, Jonsson B et al (2005) Assessment of fracture risk. Osteoporos Int 16(6):581–589. https://doi.org/10.1007/s00198-004-1780-5
Shepstone L, Lenaghan E, Cooper C, Clarke S, Fong-Soe-Khioe R, Fordham R et al (2018) Screening in the community to reduce fractures in older women (SCOOP): a randomised controlled trial. Lancet (London, England) 391(10122):741–747. https://doi.org/10.1016/S0140-6736(17)32640-5
McCloskey EV, Johansson H, Oden A, Austin M, Siris E, Wang A et al (2012) Denosumab reduces the risk of osteoporotic fractures in postmenopausal women, particularly in those with moderate to high fracture risk as assessed with FRAX. J Bone Miner Res 27(7):1480–1486. https://doi.org/10.1002/jbmr.1606
Lippuner K, Johansson H, Borgström F, Kanis JA, Rizzoli R (2012) Cost-effective intervention thresholds against osteoporotic fractures based on FRAX® in Switzerland. Osteoporos Int 23:2579–2589. https://doi.org/10.1007/s00198-011-1869-6
Zhang Z, Ou Y, Sheng Z, Liao E (2014) How to decide intervention thresholds based on FRAX in central south Chinese postmenopausal women. Endocrine 45(2):195–197. https://doi.org/10.1007/s12020-013-0076-y
Tosteson ANA, Melton LJ, Dawson-Hughes B, Baim S, Favus MJ, Khosla S et al (2008) Cost-effective osteoporosis treatment thresholds: the United States perspective. Osteoporos Int 19(4):437–447. https://doi.org/10.1007/s00198-007-0550-6
Kanis JA, McCloskey EV, Johansson H, Strom O, Borgstrom F, Oden A et al (2008) Case finding for the management of osteoporosis with FRAX--assessment and intervention thresholds for the UK. Osteoporos Int 19(10):1395–1408. https://doi.org/10.1007/s00198-008-0712-1
Chakhtoura M, Leslie WD, McClung M, Cheung AM, Fuleihan GEH (2017) The FRAX-based Lebanese osteoporosis treatment guidelines: rationale for a hybrid model. Osteoporos Int 28(1):127–137. https://doi.org/10.1007/s00198-016-3766-5
Cheung E, Cheung CL, Kung AWC, Tan KCB (2014) Possible FRAX-based intervention thresholds for a cohort of Chinese postmenopausal women. Osteoporos Int 25(3):1017–1023. https://doi.org/10.1007/s00198-013-2553-9
Lekamwasam S (2013) Sri Lankan FRAX model and country-specific intervention thresholds. Arch Osteoporos 8:148
Orimo H, Nakamura T, Hosoi T, Iki M, Uenishi K, Endo N, Ohta H, Shiraki M, Sugimoto T, Suzuki T, Soen S, Nishizawa Y, Hagino H, Fukunaga M, Fujiwara S (2012) Japanese 2011 guidelines for prevention and treatment of osteoporosis--executive summary. Arch Osteoporos 7:3–20. https://doi.org/10.1007/s11657-012-0109-9
Korthoewer D, Chandran M, Endocrine and Metabolic Society of Singapore (2012) Osteoporosis management and the utilization of FRAX®: a survey amongst health care professionals of the Asia-Pacific. Arch Osteoporos 7(1–2):193–200
Thu WPP, Logan SJS, Lim CW, Wang YL, Cauley JA, Yong EL et al (2018) Cohort profile: the Integrated Women’s Health Programme (IWHP): a study of key health issues of midlife Singaporean women. Int J Epidemiol 47(2):389–390f. https://doi.org/10.1093/ije/dyx278
Leong KH, Feng PH (1997) Bone mineral density measurements using the Hologic QD2000 in 175 Singaporean women aged 20–80. Singap Med J 38(1):25–26
Gao H, Salim A, Lee J, Tai ES, van Dam RM (2012) Can body fat distribution, adiponectin levels and inflammation explain differences in insulin resistance between ethnic Chinese, Malays and Asian Indians? Int J Obes 36(8):1086–1093. https://doi.org/10.1038/ijo.2011.185
Bewick V, Cheek L, Ball J (2004) Statistics review 13: receiver operating characteristic curves. Crit Care 8(6):508–512. https://doi.org/10.1186/cc3000
YOUDEN WJ (1950) Index for rating diagnostic tests. Cancer 3(1):32–35. https://doi.org/10.1002/1097-0142(1950)3:1<32::AID-CNCR2820030106>3.0.CO;2-3
McCloskey E, Kanis JA, Johansson H, Harvey N, Odén A, Cooper A, Cooper C, Francis RM, Reid DM, Marsh D, Selby P, Thompson F, Hewitt S, Compston J (2015) FRAX-based assessment and intervention thresholds--an exploration of thresholds in women aged 50 years and older in the UK. Osteoporos Int 26(8):2091–2099. https://doi.org/10.1007/s00198-015-3176-0
Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster JY et al (2013) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 24(1):23–57. https://doi.org/10.1007/s00198-012-2074-y
Koh LK, Saw SM, Lee JJ, Leong KH, Lee J, National Working Committee on Osteoporosis et al (2001) Hip fracture incidence rates in Singapore 1991–1998. Osteoporos Int 12(4):311–318. https://doi.org/10.1007/s001980170121
Kanis JA, Bianchi G, Bilezikian JP, Kaufman JM, Khosla S, Orwoll E, Seeman E (2011) Towards a diagnostic and therapeutic consensus in male osteoporosis. Osteoporos Int 22(11):2789–2798. https://doi.org/10.1007/s00198-011-1632-z
Levis S, Theodore G (2012) Summary of AHRQ’s comparative effectiveness review of treatment to prevent fractures in men and women with low bone density or osteoporosis: update of the 2007 report. J Manag Care Pharm 18(4 Suppl B):S1–S15 discussion S13
Ensrud KE, Taylor BC, Peters KW, Gourlay ML, Donaldson MG, Leslie WD et al (2014) Implications of expanding indications for drug treatment to prevent fracture in older men in United States: cross sectional and longitudinal analysis of prospective cohort study. BMJ 349:g4120
Eichler HG, Kong SX, Gerth WC, Mavros P, Jönsson B (2004) Use of cost-effectiveness analysis in health-care resource allocation decision-making: how are cost-effectiveness thresholds expected to emerge? Value Health 7(5):518–528. https://doi.org/10.1111/j.1524-4733.2004.75003.x
Harvey NC, McCloskey E, Kanis JA, Compston J, Cooper C (2018) Cost-effective but clinically inappropriate: new NICE intervention thresholds in osteoporosis (Technology Appraisal 464). Osteoporos Int 29(7):1511–1513. https://doi.org/10.1007/s00198-018-4505-x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
E. L. Yong and S. Lekamwasam are Joint Last Author
Rights and permissions
About this article
Cite this article
Chandran, M., McCloskey, E.V., Thu, W.P.P. et al. FRAX® based intervention thresholds for management of osteoporosis in Singaporean women. Arch Osteoporos 13, 130 (2018). https://doi.org/10.1007/s11657-018-0542-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-018-0542-5