Abstract
Summary
Greater bone mineral density was observed after treating hypertension using angiotensin-converting enzyme inhibitor (ACEi). We report decreased rate of bone loss in hypertensive black men using ACEi for 9 years. There may be a gender- and race-specific effect of ACEi in the prevention of age-associated bone loss.
Purpose
There is evidence of bone mass preservation in patients receiving ACEis, commonly used to treat hypertension. However, limitations of previous studies include being cross-sectional or only including a short-term follow-up of patients using ACEi and including patients with diabetes, which affects bone metabolism. None of the previous studies described effects of ACEi stratified by race. The objective of this study was to investigate differences in changes in bone mineral density (BMD) in older adults who suffer from hypertension and had reported ACEi use during each study visit for at least 9 years during the study, stratified by gender and race.
Methods
We used data from the Dynamics of Health, Aging and Body Composition (HABC) study, which enrolled 3075 community-dwelling older white and black individuals. We compared changes in femoral neck, total hip, and whole-body BMD after either no use of ACEi (n = 580) or long-term use (at least 9 years) of ACEi (n = 239) in HABC participants with hypertension and no known diagnosis of diabetes mellitus.
Results
Overall, BMD values significantly decreased for all subgroups over time. In the stratified multivariate analysis, long-term use of ACEi was associated with a reduced rate of decline for all three BMD measures among black men, but no significant effect was observed in the other subgroups.
Conclusion
Our findings show a gender- and race-specific effect of ACEi in the prevention of age-associated bone loss that warrants further evaluation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a disease predominantly associated with aging and results in substantial disability and reduction in quality of life [1,2,3]. Prevention and management of osteoporotic fractures can be achieved with the combined administration of calcium and vitamin D supplements, regular weight-bearing exercise, and antiresorptive or bone-forming agents. However, the use of these agents is not devoid of adverse effects [2,3,4].
Hypertension, a chronic disease that also affects older adults, is known to be associated with decreased bone mass. Reduced BMD and increased urinary calcium excretion have been observed in women with increased blood pressure, which constitutes a risk factor for the occurrence of fractures [5,6,7]. Several studies have pointed to the existence of an interconnection between bone tissue and the vasculature through the endocrine renin-angiotensin system (RAS). In vitro studies revealed that angiotensin II (AngII) receptors are expressed in osteoblasts and osteoclasts and that AngII plays a relevant role in the activation of osteoclastogenesis [8, 9]. AngII is also capable of inhibiting the differentiation and mineralization of primary osteoblast cultures and stimulating collagen synthesis [10, 11]. Moreover, upregulation of renin and angiotensin expression in bone tissue was associated with bone loss in aging mice, and activation of the RAS system in a transgenic mouse model of hypertension resulted in osteopenia due to increased bone resorption independently of the elevated blood pressure phenotype, suggesting a role for RAS activation in hypertension-related osteoporosis [12, 13]. Another study in wild-type rats showed that blocking the AngII receptor increased BMD, with decreased resorption and increased formation, further supporting AngII antagonism as a potential strategy for enhancing bone mass [14]. This led to the hypothesis that AngII antagonists could be potential agents to prevent bone loss resulting from a high turnover state, e.g., in older adults with hypertension.
Non-interventional observational studies in humans also point to some level of protection against bone loss upon administration of antihypertensive agents, including angiotensin-converting enzyme inhibitors (ACEis). In a large case-control study conducted in Denmark, which involved more than 12,400 individuals with a history of fractures, treatment with several non-diuretic antihypertensive drugs, including ACEi, resulted in an overall fracture risk reduction of 7% for any fracture and 14% for hip fracture. No dosage effect or differences between genders and age groups were observed [15]. Moreover, hypertensive patients aged ≥ 80 years treated with a combination of an ACEi and a thiazide-like diuretic in the randomized controlled Hypertension in the Very Elderly Trial (HYVET) trial also showed fewer fractures [16]. In a cross-sectional, community-based study, ACEi use was associated with increased femoral neck BMD in Chinese adults [17]. A cross-sectional analysis of patients from the Health, Aging and Body Composition (HABC) study showed a positive correlation between femoral neck BMD and use of ACEis for men (analysis was not stratified by ethnic/racial background), but not for women, after 5 years of treatment [18]. In addition, in a randomized study of hypertensive patients receiving an ACEi, e.g., enalapril, or quinapril in combination with hydrochlorothiazide, quinapril maintained BMD over 1 year [19].
Altogether, these data suggest that RAS-inhibiting antihypertensive medications may have a potential role in the prevention of bone loss and, consequently, debilitating fractures in the elderly. Thus, ACEis show a potential dual role in cardiovascular and bone loss prevention in the elderly, which led to the hypothesis that they could be potential medications to prevent bone loss resulting from a high turnover state. The few human observational studies that report bone loss prevention after use of an ACEi are limited to mostly cross-sectional designs or short-term follow-up periods of patients. In addition, the use of ACEis in these studies was not limited to those with hypertension only and included other diseases known to alter bone metabolism, e.g., diabetes mellitus. Moreover, none of these studies investigated whether the effects of ACEis would vary by race/ethnicity [15,16,17,18]. The main objective of this longitudinal analysis of elderly, hypertensive individuals receiving long-term (at least 9 years) treatment with ACEis to control blood pressure was to identify differences in BMD or bone loss dynamic determined by gender and race/ethnicity in those with hypertension without any known diagnosis of diabetes mellitus.
Methods
Study population
The Health, Aging and Body Composition (HABC) study is an observational, prospective study sponsored by the National Institutes of Health that aimed to understand functional decline in community-dwelling elderly individuals by establishing correlations between changes in body composition, disability, and other age-related conditions. The study was conducted between 1997 and 2016 at two sites in Memphis, TN, and Pittsburgh, PA, and included 3075 participants aged 70–79 years who did not report with disability when performing daily routine activities or any functional limitations. The HABC study was conducted in accordance with the ethical principles of clinical research in human subjects and was approved by the institutional review boards of the University of Pittsburgh and the University of Tennessee, Memphis [20].
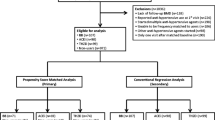
This longitudinal analysis of existing data from the HABC study included patients with a diagnosis of hypertension, either self-reported or confirmed by a physician. Participants must have had hip total, femoral neck, or whole-body DXA data from at least two visits in order to calculate change in BMD. Exclusion criteria for this analysis were diagnosis of diabetes or reported use of diabetes medication at any follow-up visit, use of angiotensin II receptor blockers at baseline or any follow-up visit, thiazides use at baseline visit, unknown ACEi use status, or missing baseline clinical or biochemical parameters (e.g., albumin, creatinine, calcium, 25OHD). Medications were brought in by patients during data collection visits and were recorded at the time of the visit. Fig. 1.
Variables
Demographic information and baseline medical history of hypertension and major diseases and report of use of medications for bone loss prevention (e.g., bisphosphonates, calcitonin, steroids, calcium, and vitamin D supplements) were abstracted from the HABC database. Hip total, femur neck, and whole-body BMD were measured using DXA at baseline (year 1) and 4 (year 5) and 9 (year 10) years after baseline. Outcome variables were hip total, femur neck, and whole-body BMD. History of ACEi use was the independent variable for our analysis. Long-term use of ACEi was defined as anyone reporting use of ACEis at baseline and at year 5 and year 10 at the data collection visit. Participants who never reported any use of ACEis were in the “non-long-term ACEi users” category.
Statistical analysis
The effect of long-term ACEi use on changes in hip total, femoral neck, and whole-body total BMD from baseline to 9 years after baseline was assessed using an adjusted longitudinal mixed model with random intercept and an autoregressive correlation structure. Data were adjusted for confounding factors that can potentially affect bone tissue, such as concomitant medications, history of fractures, and smoking status. Independent two-sample t-tests were used to assess differences in mean BMD between ACEi use groups at different time points (cross-sectional). A stratified analysis was done separately for white men, white women, black men, and black women [21]. Multiple regression models with absolute BMD changes as dependent variables and ACEi exposure for 9 years as the independent variable adjusted for age, gender, and race, concomitant medications and other demographic data were developed. The statistical analysis was performed using SAS 9.4 software.
Results
Of the 3075 participants in the HABC study, 819 met the eligibility criteria for this study and were included in analyses (Figs. 1 and Fig. 2); 239 (29.3%) participants were long-term users (i.e., use for at least 9 years) of ACEi. The demographic characteristics did not differ overall between the two ACEi use groups (long-term use and no use). The mean age was approximately 73 years for both groups, and about half (49%) of the participants were men. Black men and women constituted approximately one fourth (26%) of the study population. No significant differences were observed between groups regarding body mass index (BMI) at 25 years old, serum creatinine, calcium, or vitamin D levels (Table 1). More people started using bisphosphonates or osteoporosis drugs as the study went along [43 of 813 (5.3%) in year 1, 100 (12.3%) in year 5, and 138 (17%) at year 10 (data not shown in results)]. However, after a sensitivity analysis for osteoporosis drug use was done, our results still held the same.
All three measures of baseline BMD differed significantly between all race/gender groups (p < 0.001). In unadjusted analyses stratified by race and gender, baseline BMD was similar in those with and without long-term ACEi use with the exception of black men (Table 2). Overall, hip total, femoral neck, and whole-body total BMD values decreased for all groups over time, except in black men. BMD measures at each time point were similar between long-term users (ACEi use for 9 years) of ACEi and non-users among whites and black women, whereas they were higher for black men (Table 2).
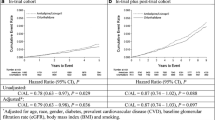
The gender and race were significant predictors of BMD over time in a multivariate model also including site, age, BMI at age 25, albumin, creatinine, calcium, 25OHD, and history of fracture (p < 0.001 for both gender and race for all BMD measures). Adding an interaction between race/gender group and long-term ACEi use on BMD was marginally significant (hip total, p = 0.12; femoral neck, p = 0.17; whole-body total, p = 0.09). The interaction effect was most strongly present between black men and the other three race/gender groups based on pairwise comparisons, and an interaction term specifically for the effect of long-term ACEi use in black men compared to long-term ACEi for all other participants found more significant results (hip total, p = 0.02; femoral neck, p = 0.08; whole-body total, p = 0.03), so we proceeded with the planned stratified analysis by race and gender. In the stratified multivariate analysis, long-term use of ACEi was associated with a reduced rate of decline for all three BMD measures among black men, but no significant effect was observed in the other subgroups (Table 3). Long-term ACEi use was associated with a relative increase in total hip BMD of 0.096 g/cm2 per year, an increase over 9 years of about 9% of baseline BMD (Fig. 1).
Discussion
We report a significant increase in total hip, femur, neck, and whole-body BMD in black men with long-term ACEi intake (for 9 years). This is the first long-term analysis of ACEi effects on bone loss taking race/ethnicity and gender into consideration. According to the literature, ACEi administration seems to induce beneficial changes in bone mass, although there are some conflicting data and apparent gender-specific effects [22, 23]. A community-based study revealed higher BMD measures for Chinese elderly men [17], but a protective effect was not seen in this patient population in a more recent cohort study [24]. Older Japanese men also did not benefit from treatment with ACEis in regard to bone health [25], and a large prospective study of American men aged ≥ 70 years showed that continuous use of ACEi actually induced a smaller increase in total hip and femur neck BMD loss over a period of 4 years [23].
In this longitudinal analysis, overall bone loss occurred over a period of 9 years, which is expected considering the advanced age of these participants. The protective effect of ACEi was more pronounced in men than in women, regardless of race/ethnicity (Table 3); however, this effect was small, which is in agreement with prior studies. The HABC dataset includes interim data from year 8, which we have not included in the presented analyses. However, sensitivity analysis using only data from baseline (year 1) and 5 years after baseline and an analysis incorporating data available from year 8 generated similar results and did not change the conclusions for the relationship between time of ACEi use and BMD in any stratum. A gender and race-/ethnicity-specific bone protective effect was observed in black men only, but further evaluation is needed. Presence of specific ACE polymorphisms could potentially point to genetic differences with impact in bone health and response to ACEi treatment. In fact, the ACE deletion (D) polymorphism in the homozygous state (DD) has been associated with osteoporosis in postmenopausal women, and ACEis, e.g., quinapril and enalapril, showed efficacy in increasing BMD in DD hypertensive female carriers, who show increased plasma and tissue AngII levels, in a 1-year randomized trial [19, 26]. Although our analysis is limited in doing any genetic analysis, the study reporting polymorphism does not provide information on variations by racial/ethnic differences. A future analysis for polymorphism by gender and race/ethnic background may be helpful in deciphering if the difference in effects of ACEi between black and white men and women observed in our study could be due to such variations due to polymorphism.
Increased osteoprotegerin (OPG)/receptor activator of nuclear factor-kappa B ligand (RANKL) ratio was reported after ACEi in ovariectomized rats [27]. Antiresorptive effects of ACEi through antiosteoclastogenic activities reported in other [8, 9] along with the increased OPG/RANKL ratio explains why use of ACEi would be associated with decreased bone loss, as observed in our study. Whether there are variations of these biomarkers between men and women from different racial/ethnic background is unknown. Further analysis of biomarkers including OPG and RANKL is recommended for confirming our findings and help policy makers to determine if a recommendations for ACEi use for treating hypertension in men at risk of bone loss could potentially help preventing osteoporosis in men in old age.
Differences in plasma renin activity (PRA) between black and white men women has been discussed as reasons for prescribing ACEi for treating hypertension in them [28]. Overall, ACEi was found to be useful in limiting organ damage due to long-term hypertension and was encouraged to use in both black and white men and women with a focus on individualizing treatment plan for each patient [28]. While we see more pronounced effects with significant improvement in BMD in black men, our results indicate that ACEi could be useful in older adults at risk of age-related bone loss and, therefore, could be helpful in individualizing cardiovascular and bone health care in older patients, specifically black men.
This observational study is the first study to look into ACEi use and differences in BMD potentially determined by race and provides a unique opportunity to assess changes over time in elderly white and black individuals at risk of bone loss. Limitations of the study include a small sample size; a significant number of participants in the HABC study were excluded because of missing data, presence of diabetes or because they were receiving other antihypertensives (thiazide and/or ARBs). Another limitation of the study is its reduced racial/ethnic representation beyond races/ethnicities of black and white. Absence of spine scans limits us from interpreting effects of ACEis on vertebral trabecular bone. Additionally, lack of detailed information on ACEi dosing makes it difficult to discuss if specific doses could be associated with our results. Information about adherence to treatment for hypertension or dietary habits and other lifestyle factors influencing bone health was not available and may have affected the results.
In summary, long-term ACEi intake corresponded in general to higher cross-sectional BMD in black men at all data points. Change in BMD did not differ by ACEi use except in black men, who had gains in BMD associated with long-term ACEi use. This is the first long-term analysis of ACEi effects on bone loss taking race/ethnicity into consideration; further evaluation of the influence of other racial/ethnic groups and genetic background in ACEi protective action is warranted. Knowledge of the specific long-term effects of these agents on bone will ultimately lead to improved treatment plans tailored to older hypertensive adults at risk of developing osteoporosis. This dual beneficial role of ACEi in the cardiovascular and bone tissues may help reduce pill burden and consequently contribute to improved treatment convenience and adherence among elderly patients with multiple comorbidities.
References
National Osteoporosis Foundation (NOF). www.nof.org. Accessed on 25 Jan 2017
Kling JM, Clarke BL, Sandhu NP (2014) Osteoporosis prevention, screening, and treatment: a review. J Women's Health (Larchmt) 23(7):563–572
Reginster JY, Neuprez A, Dardenne N et al (2014) Efficacy and safety of currently marketed anti-osteoporosis medications. Best Pract Res Clin Endocrinol Metabol 28(6):809–834
Silverman S, therapy CCI o (2012) Osteoporos Int 23(3):797–809
Cappuccio F, Meilahn E, Zmuda JM, Cauley JA, for the Study of Osteoporotic Fractures Research Group (1999) High blood pressure and bone-mineral loss in elderly white women: a prospective study. Lancet 354:971–975
Tsuda K, Nishio I, Masuyama Y (2001) Bone mineral density in women with essential hypertension. Am J Hypertens 14:704–707
Vestergaard P, Rejnmark L, Mosekilde L (2009) Hypertension is a risk factor for fractures. Calcif Tissue Int 84:103–111
Hatton R, Stimpel M, Chambers TJ (1997) Angiotensin II is generated from angiotensin I by bone cells and stimulates osteoclastic bone resorption in vitro. J Endocrinol 152(1):5–10
Shimizu H, Nakagami H, Osako MK et al (2008) Angiotensin II accelerates osteoporosis by activating osteoclasts. FASEB J 22:2465–2475
Hagiwara H, Hiruma Y, Inoue A et al (1998) Deceleration by angiotensin II of the differentiation and bone formation of rat calvarial osteoblastic cells. J Endocrinol 156:543–550
Lamparter S, Kling L, Schrader M et al (1998) Effects of angiotensin II on bone cells in vitro. J Cell Physiol 175:89–98
SS G, Zhang Y, Li XL et al (2012) Involvement of the skeletal renin-angiotensin system in age-related osteoporosis of ageing mice. Biosci Biotechnol Biochem 76:1367–1371
Asaba Y, Ito M, Fumoto T et al (2009) Activation of renin-angiotensin system induces osteoporosis independently of hypertension. J Bone Miner Res 24(2):241–250
Izu Y, Mizoguchi F, Kawamata A et al (2008) Angiotensin II type 2 receptor blockade increases bone mass. J Biol Chem 284(8):4857–4864
Rejnmark L, Vestergaard P, Mosekilde L (2006) Treatment with beta-blockers, ACE inhibitors, and calcium-channel blockers is associated with a reduced fracture risk: a nationwide case–control study. J Hypertens 24(3):581–589
Peters R, Beckett N, Burch L et al (2010) The effect of treatment based on a diuretic (indapamide) ± ACE inhibitor (perindopril) on fractures in the hypertension in the very elderly trial (HYVET). Age Ageing 39(5):609–616
Lynn H, Kwok T, Wong SYS et al (2006) Angiotensin converting enzyme inhibitor use is associated with higher bone mineral density in elderly Chinese. Bone 38:584–588
Rianon N, Garcia M, Stotts A et al (2011) Associations between femur neck BMD and antihypertensive medications affecting renin-angiotensin system in elderly men and women of the Health ABC study. Presented at the Forum on Aging and Skeletal Health. Bethesda, MD
Perez-Castrillon JL, Silva J, Justo I et al (2003) Effect of quinapril, quinapril-hydrochlorothiazide, and enalapril on the bone mass of hypertensive subjects: relationship with angiotensin converting enzyme polymorphisms. Am J Hypertens 16(6):453–459
National Institute on Aging. Health ABC. https://www.nia.nih.gov/research/intramural-research-program/dynamics-health-aging-and-body-composition-health-abc. Accessed on 25 Jan 2017
Looker AC, Wahner HW, Dunn WL et al (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8:468–489
Solomon D, Ruppert K, Zhao Z et al (2016) Bone mineral density changes among women initiating blood pressure lowering drugs: a SWAN cohort study. Osteoporos Int 27:1181–1189
Kwok T, Leung J, Zhang YF et al (2012) Does the use of ACE inhibitors or angiotensin receptor blockers affect bone loss in older men? Osteoporos Int 23:2159–2167
Zhang YF, Qin L, Leung PC et al (2012) The effect of angiotensin-converting enzyme inhibitor use on bone loss in elderly Chinese. J Bone Miner Metab 30(6):666–673
Masunari N, Fujiwara S, Nakata Y et al (2008) Effect of angiotensin-converting enzyme inhibitor and benzodiazepine intake on bone loss in older Japanese. Hiroshima J Med Sci 57:17–25
Cakmak B, Inanir A, Karakus N et al (2015) Association between the ACE gene I/D polymorphism and osteoporosis in a Turkish population. Z Rheumatol 74:346–350
Allam M, Hussien N (2016) A comparative study between the effect of 17-βestradiol and angiotensin converting enzyme inhibitor on osteoporosis in ovariectomized rats. Gen Physiol Biophys 35:433–441
Jamerson K (2000) Rationale for angiotensin II receptor blockers in patients with low-renin hypertension. Am J Kidney Dis 36:S24–S30
Acknowledgements
The authors received writing support from Patricia Fonseca, a freelance medical writer. The authors would like to acknowledge help from Sara Zwart for preparing figures. Susan Rubin, Steve Kritchevsky, Anne Newmen, Suzanne Satterfield, Diane Ives, Evan Tylavsky, and Jane Cauley contributed to data acquisition.
Author information
Authors and Affiliations
Contributions
All authors approved the final version submitted and are accountable for the accuracy and the integrity of the data presented.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Rianon, N., Ambrose, C.G., Pervin, H. et al. Long-term use of angiotensin-converting enzyme inhibitors protects against bone loss in African-American elderly men. Arch Osteoporos 12, 94 (2017). https://doi.org/10.1007/s11657-017-0387-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-017-0387-3