Abstract
Background
Disparities in opioid prescribing among racial and ethnic groups have been observed in outpatient and emergency department settings, but it is unknown whether similar disparities exist at discharge among hospitalized older adults.
Objective
To determine filled opioid prescription rates on hospital discharge by race/ethnicity among Medicare beneficiaries.
Design
Retrospective cohort study.
Participants
Medicare beneficiaries 65 years or older discharged from hospital in 2016, without opioid fills in the 90 days prior to hospitalization (opioid-naïve).
Main Measures
Race/ethnicity was categorized by the Research Triangle Institute (RTI), grouped as Asian/Pacific Islander, Black, Hispanic, other (American Indian/Alaska Native/unknown/other), and White. The primary outcome was an opioid prescription claim within 2 days of hospital discharge. The secondary outcome was total morphine milligram equivalents (MMEs) among adults with a filled opioid prescription.
Key Results
Among 316,039 previously opioid-naïve beneficiaries (mean age, 76.8 years; 56.2% female), 49,131 (15.5%) filled an opioid prescription within 2 days of hospital discharge. After adjustment, Black beneficiaries were 6% less likely (relative risk [RR] 0.94, 95% CI 0.91–0.97) and Asian/Pacific Islander beneficiaries were 9% more likely (RR 1.09, 95% CI 1.03–1.14) to have filled an opioid prescription when compared to White beneficiaries. Among beneficiaries with a filled opioid prescription, mean total MMEs were lower among Black (356.9; adjusted difference − 4%, 95% CI − 7 to − 1%), Hispanic (327.0; adjusted difference − 7%, 95% CI − 10 to − 4%), and Asian/Pacific Islander (328.2; adjusted difference − 8%, 95% CI − 12 to − 4%) beneficiaries when compared to White beneficiaries (409.7).
Conclusions and Relevance
Black older adults were less likely to fill a new opioid prescription after hospital discharge when compared to White older adults and received lower total MMEs. The factors contributing to these differential prescribing patterns should be investigated further.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Over 2 million older adults are estimated to receive a new opioid prescription on hospital discharge annually.1 Prior studies have shown disparities in opioid prescribing among racial and ethnic minority groups in outpatient2 and emergency department settings.3,4 When patients from racial and ethnic minority groups do receive an opioid, they tend to receive a lower dose than White patients and this disparity persists within and across hospital systems.5,6 Research suggests no difference in prevalence of pain in minority groups when compared to White adults,7 resulting in concern for inadequate treatment of pain among minority groups.
Rates of opioid overdose have sharply risen over the last two decades, with an appropriate national focus on interventions to reduce opioid use. However, it is generally accepted that opioids have an indication for managing short-term moderate to severe pain, which clinicians must balance against the risks of adverse effects, including side effects, opioid use disorder, overdose, and death. Inadequate pain treatment may lead to poor quality of life, delayed hospital discharge, increased post-discharge care utilization, and worsened chronic surgical pain.8,9,10 Although risk factors for opioid-related adverse events are well-established,11,12 applying this information to an individual patient in a manner that allows for an understanding of the weight of the risks and benefits relative to one another is an inherently subjective practice, relying mostly upon clinical judgment, and subject to the influence of bias—implicit or explicit.
One prior single-center study showed that Black patients were less likely to receive opioids on hospital discharge and tended to receive shorter courses compared to White patients.13 However, no studies to date have evaluated if there are racial and ethnic disparities in opioid prescribing among opioid-naïve older adults on hospital discharge using national data. This study aimed to understand opioid prescribing patterns among racial and ethnic groups, and the effect of hospital racial composition on opioid prescribing disparities. We hypothesized that individuals belonging to a racial or ethnic minority group would be less likely to receive opioids on hospital discharge compared to White patients, and that disparities may be more evident in hospitals with greater proportions of White patients.
METHODS
Study Design and Data Collection
We conducted a retrospective cohort study using a 20% sample of US Medicare beneficiaries discharged home following an acute hospitalization in 2016. This study was restricted to secondary data analysis and approved with a waiver of informed consent by the Institutional Review Board at Beth Israel Deaconess Medical Center. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for cohort studies.13
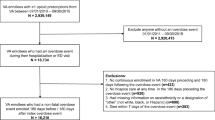
We included fee-for-service Medicare beneficiaries who were at least 65 years old with continuous enrollment in Medicare Parts A, B, and D for at least 12 months prior to hospitalization and 1 month after discharge. We excluded beneficiaries admitted from or discharge to skilled nursing facilities, as Part D claims are unavailable for these care settings. We excluded beneficiaries who had filled any opioid prescriptions in the 90 days prior to hospitalization. We further excluded beneficiaries who had an International Classification of Diseases (ICD) diagnosis code for sickle cell anemia and those discharged to hospice or who had hospice claims 12 months before or 1 week after discharge, owing to the unique aspects of pain management in these populations. Finally, we excluded hospitals with fewer than 30 discharges, due to the lack of precision in the corresponding hospital-level racial composition and opioid prescribing estimates. After applying these exclusion criteria, we randomly chose a single hospitalization per beneficiary to avoid correlated observations. See Figure 1 for a complete list of exclusion criteria.
Exposures and Covariates
Our predictor of interest was race/ethnicity, defined using the Research Triangle Institute (RTI) Race Code,14 grouped as Asian/Pacific Islander, Black or African American, Hispanic, non-Hispanic White, and other (American Indian, Alaskan Native, unknown, or other race).
Beneficiary-level covariates included age, sex, disability entitlement, Area Deprivation Index of residence (further defined below), Medicare-Medicaid dual-eligibility status, Elixhauser comorbidity score,15,16 and presence of chronic painful conditions. Chronic painful conditions were defined based on the US national pain strategy group diagnostic clusters for identifying patients with chronic pain for population research.17,18 Area Deprivation Index is a validated measure that uses 17 social and economic variables to create a percentile indicating social deprivation, with higher percentiles indicating greater social need.19 We matched a beneficiary to ADI percentile using their 9-digit zip code and categorized them into four quartiles. Due to differences in cohort inclusion criteria across data purchase episodes, 9-digit zip codes were missing for 35,550 beneficiaries who died within 30 days of hospital discharge (11.2% of the cohort). Additionally, 2683 (0.8%) did not have an ADI percentile in the Neighborhood Atlas due to reasons such as low population numbers or residence in group homes.20 To account for those with missing ADI data, we used the missing covariate indicator method, which allowed us to retain observations with missing data in the model.21 We conducted a sensitivity analysis excluding the ADI covariate from the model and results were largely unchanged.
Hospitalization-level covariates included hospital length of stay, intensive care unit stay, medical/surgical diagnosis–related group (DRG), and principal diagnosis and procedure codes defined by the HCUP Clinical Classification Software.22 Hospital-level covariates included US Census Region, rural/urban location, teaching status, and hospital minority composition. Because there may be hospital differences in tendency to prescribe opioids, which may be associated with hospital racial composition, we determined the racial and ethnic minority composition for each hospital and created a variable placing hospitals into quartiles of racial and ethnic minority composition.
Outcomes
Our primary outcome was a filled opioid prescription (i.e., opioid claim) within 2 days of hospital discharge, defined using the Centers for Disease Control (CDC) National Center for Injury Prevention and Control compilation of opioid analgesics. We excluded claims for buprenorphine formulations intended for treatment of opioid use disorder, as defined by the CDC algorithm.23 For beneficiaries with a filled opioid prescription, we calculated a secondary outcome of total morphine milligram equivalents (MMEs) filled. For those who received more than one opioid prescription within 2 days of discharge, we summed the MMEs across the prescriptions.
Statistical Analysis
All statistical analyses were conducted using SAS Software Version 9.4 and STATA v14.1. Bivariable analyses were performed to describe the beneficiary-, hospitalization-, and hospital-level descriptive characteristics by race/ethnicity. For unadjusted analyses, we used chi-square tests to compare proportions, and ANOVA to compare continuous data. For our primary outcome of filled opioids, we fit a multivariable generalized estimating equation model using a Poisson error term with log link to determine the adjusted relative risk of a filled opioid prescription after discharge by race/ethnicity, adjusting for the covariates. We then calculated post-estimation marginal effects and marginal differences, allowing us to report the predicted probability of filling an opioid prescription on hospital discharge by race/ethnicity after adjusting for covariates.24 For beneficiaries who filled an opioid prescription within 2 days of hospital discharge, we then fit a generalized estimating equation model to generate adjusted relative differences for our secondary outcome of total MME (log transformed, normal distribution) by race/ethnicity.
We further examined the extent to which hospital racial composition explained observed racial and ethnic differences in filled opioid prescriptions. To demonstrate the effect of adjustment for hospitals with varying minority populations, we present the results from each adjusted model with and without inclusion of the hospital minority composition quartile variable.
All models accounted for clustering at the hospital level using an exchangeable working correlation structure.
Subgroup Analyses
To further address possible confounding in our results, we performed analyses of our primary and secondary outcomes in two pre-defined subgroups with more homogeneous indications for opioid use: beneficiaries with cancer as the principal discharge diagnosis using Agency for Healthcare Research and Quality Clinical Classification Software (CCS) groupings22 and beneficiaries with a surgical DRG.
Role of the Funding Source
This work was funded by grant number R01HS026215 from the Agency for Healthcare Research and Quality. The funding agency had no role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of any of the funding agency.
RESULTS
Cohort Characteristics
There were 316,039 unique beneficiaries included in the cohort (Fig. 1), of which 256,584 were White (81.2%), 28,047 were Black (8.9%), 18,107 were Hispanic (5.7%), 7481 were Asian/Pacific Islander (2.4%), and 5820 were other (1.8%). The mean age of the cohort was 76.8 years and 56.2% were female. The most common principal discharge diagnosis categories across all races/ethnicities were circulatory (25.6–30.1%), digestive (12.2–15.1%), and respiratory (10.5–12.2%). The most common principal procedure categories across all races/ethnicities were musculoskeletal (4.5–13.6%), cardiovascular (5.2–8.2%), and digestive (3.3–5.6%) (Table 1). See Supplementary Table 1 for the full list of principal diagnosis and primary procedure groupings by race/ethnicity. Compared to White beneficiaries, Black beneficiaries were more likely to be female (62.4% vs 55.7%), to have disability as their reason for Medicare eligibility (1.5% vs 0.5%), and to have higher mean Elixhauser comorbidity score (3.5 vs 3.0) (Table 1). Black beneficiaries also resided in areas of higher social deprivation, reflected by a higher proportion of beneficiaries in the highest Area Deprivation Index quartile when compared to White beneficiaries (43.5% vs 18.1%). Compared to White beneficiaries, Asian/Pacific Islander beneficiaries had higher ICU utilization (29.8% vs 25.0%) and admission to urban hospitals (98.2% vs 89.7%).
Filled Opioid Prescriptions After Discharge
Overall, 49,131 (15.5%) beneficiaries had an opioid claim within 2 days of hospital discharge. Black beneficiaries had the lowest incidence of filled opioid prescriptions (9.9%), and White beneficiaries had the highest incidence (16.5%) (p < 0.001; Table 2). After adjusting for beneficiary, hospitalization, and hospital characteristics, Black beneficiaries had lower adjusted relative risk (RR) of filling an opioid prescription after discharge (0.94 [95% confidence interval 0.91–0.97]) than White beneficiaries. Using post-estimation margins, Black beneficiaries had a lower predicted probability of filling opioids compared to White beneficiaries (14.7% vs 15.5%; difference − 0.9% [95% CI − 1.4%, − 0.3%]). In contrast, Asian/Pacific Islander beneficiaries had a higher adjusted RR of filling an opioid prescription after discharge than White beneficiaries (1.09 [95% CI 1.03, 1.14]), with a higher predicted probability of filling an opioid (16.8% vs 15.5%; difference 1.2% [95% CI 0.3%, 2.1%]) when compared to White beneficiaries.
Total MME of Filled Opioids
Among the 49,131 (15.5%) beneficiaries who filled an opioid prescription within 2 days of hospital discharge, White beneficiaries had a higher mean total MME (409.7) than Black beneficiaries (356.9), Hispanic beneficiaries (327.0), and Asian/Pacific Islander beneficiaries (328.2) (p < 0.0001; Table 3). After adjusting for beneficiary, hospitalization, and hospital characteristics, total MME filled was lower for Black (mean adjusted relative difference [RD] − 4% [95% CI − 7%, − 1%]), Hispanic (− 7% [95% CI − 10%, − 4%]), and Asian/Pacific Islander beneficiaries (− 8% [95% CI − 12%, − 4%]).
Filled Opioid Prescriptions by Hospital Minority Composition
Compared to hospitals with the lowest minority beneficiary composition, hospitals with the highest minority beneficiary composition had a lower percentage of beneficiaries filling an opioid after hospital discharge across all races and ethnicities (p < 0.001 for all; Fig. 2). As the hospital minority beneficiary composition increased, there were increased differences in the percentage filling an opioid between Black and White beneficiaries (absolute differences of 2.4%, 5.3%, 6.0%, and 5.9% in the lowest to highest minority composition quartiles, respectively; p < 0.0001). The incidence of a Black beneficiary filling an opioid after discharge decreased steadily as the percentage of Black beneficiaries at that hospital increased (14.4% for quartile 1, 11.6% for quartile 2, 10.9% for quartile 3, and 8.7% for quartile 4; Fig. 2). Black beneficiaries continued to fill opioids at a lower rate than White beneficiaries after inclusion of hospital minority composition in our adjusted model (RR 0.96 [95% CI 0.93, 0.998]; Table 2).
Subgroup Analyses: Cancer and Surgical Hospitalizations
There were 13,095 beneficiaries with a principal discharge diagnosis of cancer. In the cancer subgroup, no significant differences were observed in the incidence of filled opioid prescription after discharge by race/ethnicity (Supplementary Table 2). However, among beneficiaries who filled an opioid prescription, Hispanic beneficiaries filled lower total MMEs when compared to White beneficiaries (mean adjusted RD − 10% [95% CI − 17%, − 2%]) (Supplementary Table 3). Results were similar after adjusting for hospital minority beneficiary composition.
There were 98,647 beneficiaries discharged following a surgical hospitalization. In this subgroup, Black beneficiaries were less likely to fill an opioid prescription after discharge than White beneficiaries (adjusted RR 0.95, 95% CI 0.92, 0.99; Supplementary Table 4). Among beneficiaries who filled an opioid prescription, Hispanic and Asian/Pacific Islander beneficiaries filled lower total MMEs (mean adjusted RD − 6% [95% CI − 9%, − 3%] and − 7% [95% CI − 11%, − 3%], respectively) (Supplementary Table 5).
DISCUSSION
In this national sample of older adults discharged home after acute care hospitalizations, Black beneficiaries were less likely to have filled an opioid prescription after hospital discharge and received a lower dose when compared to White beneficiaries. Although the minority composition of a hospital served as an effect modifier, these disparities were not fully explained by the minority composition of the hospital. Asian/Pacific Islander beneficiaries were more likely to fill opioids on discharge than White beneficiaries. This study adds to prior work demonstrating racial disparities in opioid prescribing in varied settings and highlights the need for additional work aimed at understanding the drivers and mitigators of these concerning patterns.
Pain is a subjective measure that is difficult to quantify, resulting in reliance on patient perception and clinical judgment for treatment decisions. This introduces opportunity for bias in pain assessment and associated treatment decisions on the part of the clinician. Studies have noted that pain is less likely to be diagnosed and treated in Black beneficiaries.25,26 Both individual and institutional racism may contribute to the differential prescribing patterns that we observed. Studies have demonstrated that many health care practitioners hold false beliefs about biological differences between Black and White patients, and that these beliefs predict racial bias in pain assessment and treatment decisions.27 However, due to the nature of claims data, we cannot determine the appropriateness of opioid prescribing in this analysis. The findings reflect differences in prescribing by race/ethnicity, but in the absence of information on pain severity or response to treatment, we cannot ultimately comment on whether our results reflect over-prescribing for White patients, under-prescribing for Black patients, or a combination of both.
Our finding of lower rates of filled opioid prescriptions in Black beneficiaries is consistent with prior literature in different clinical settings. It is consistent with the one prior single-center study of opioid prescribing on hospital discharge, in which Black patients had a 3.1% lower predicted population rate of receiving an opioid on hospital discharge than White patients.13 We showed similar results in a national cohort, suggesting that disparities exist across the country, although the magnitude of the disparity was lower in our cohort (− 0.9% predicted marginal difference for Black vs White beneficiaries). Because our study focused on older adults, one possible explanation for the smaller difference observed in our study is that older age could mitigate racial/ethnic disparities in opioid prescribing. This raises an important consideration for future study to compare disparities and understand prescriber behavior in older adults when compared to younger adults. Similar to this study, we found that Asian/Pacific Islander beneficiaries had a higher opioid fill rate when compared to White beneficiaries after adjustment. Given recent data demonstrating increasing prescription opioid misuse among Asian individuals from 2000 to 2012,28,29 further studies designed to better understand the reasons for differential prescribing and efforts to develop culturally sensitive interventions are imperative.
To further determine the level of care that most impacted the observed differential prescribing patterns, we assessed the impact of adjustment for the minority composition of hospitals in our cohort, above and beyond beneficiary, hospitalization, and other hospital characteristics. Although the disparity in prescribing between Black and White beneficiaries was evident within each quartile of hospital minority composition, disparities were greatest in hospitals with higher minority composition, compared to hospitals with lower minority composition. In other words, a Black patient admitted to a hospital with a low minority prevalence was more likely to receive an opioid than a Black patient admitted to a hospital with a high minority prevalence. Taken together with our finding that hospitals with lower minority composition tended to prescribe opioids more frequently across all races/ethnicities, these findings may suggest that the same factors driving prescribing disparities at the patient-level may also contribute to hospital-level prescribing disparities. Namely, Black patients admitted to hospitals with more White patients, and an associated higher overall opioid prescribing rate, may be managed more similarly to the White patients that surround them—a phenomenon somewhat akin to regression to the mean. For Asian/Pacific Islander beneficiaries, we found a similar trend wherein beneficiaries admitted to hospitals with higher minority population filled fewer opioids than beneficiaries admitted to hospitals with lower minority population. Interventions designed to facilitate between-hospital opioid prescribing comparisons and awareness may serve as fruitful targets for future research into mitigating these disparities at the hospital and patient level.
The observed disparities for Black beneficiaries in filled opioid prescriptions after discharge were similar when focusing on beneficiaries with a surgical hospitalization, but no longer apparent when focusing on beneficiaries with a cancer-related hospitalization. However, disparities in total MME were similar in magnitude when focusing on these subgroups, albeit no longer significant in the setting of reduced sample size and power. These findings suggest that disparities may be less manifest in decisions regarding when to prescribe opioids, and more manifest in decisions around how much to prescribe. Such insights may begin to suggest hypotheses for further testing in future research, such as whether the perceived strength of the indication for opioid prescribing affects prescribing decisions and associated disparities.
There are several limitations of our study. Because it was an observational study, it is not possible to rule out unmeasured confounders, which limits our ability to make casual assumptions. Moreover, claims data reflect filling of a prescription, rather than issuance of a prescription. As some states allow partial fills of opioid prescriptions, we cannot be sure that disparities in MME are due to disparities in prescribing practices. It is also possible that some patients did not fill post-discharge opioid prescriptions at all. The significant social and financial barriers that limit the ability of many racial/ethnic minorities to fill a prescription could explain some of the disparity, but this is less likely as few opioid medications are high cost or branded.
CONCLUSIONS
Among opioid-naïve older adults who were hospitalized in 2016, Black beneficiaries were less likely to fill an opioid prescription on discharge and received significantly lower amounts of total MME. Although absolute differences were small, when spread across the 2 million older adults who are newly prescribed opioids on discharge annually, the potential public health impact is large. Further research should aim to understand the drivers and mitigators of the observed prescribing disparities and their impact on patient outcomes.
References
Herzig SJ, Anderson TS, Jung Y, Ngo L, Kim DH, McCarthy EP. Relative Risks of Adverse Events Among Older Adults Receiving Opioids Versus NSAIDs After Hospital Discharge: a Nationwide Cohort Study. Basu S, ed. PLOS Med. 2021;18(9):e1003804. https://doi.org/10.1371/journal.pmed.1003804
Ly DP. Association of Patient Race and Ethnicity With Differences in Opioid Prescribing by Primary Care Physicians for Older Adults With New Low Back Pain. JAMA Health Forum. 2021;2(9):e212333. https://doi.org/10.1001/jamahealthforum.2021.2333
Pletcher MJ, Kertesz SG, Kohn MA, Gonzales R. Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments. JAMA. 2008;299(1):70-78. https://doi.org/10.1001/jama.2007.64
Meghani SH, Byun E, Gallagher RM. Time to Take Stock: a Meta-Analysis and Systematic Review of Analgesic Treatment Disparities for Pain in the United States. Pain Med. 2012;13(2):150-174.https://doi.org/10.1111/j.1526-4637.2011.01310.x
Lee P, Le Saux M, Siegel R, et al. Racial and Ethnic Disparities in the Management of Acute Pain in US Emergency Departments: Meta-Analysis and Systematic Review. Am J Emerg Med. 2019;37(9):1770-1777.https://doi.org/10.1016/j.ajem.2019.06.014
Morden NE, Chyn D, Wood A, Meara E. Racial Inequality in Prescription Opioid Receipt — Role of Individual Health Systems. N Engl J Med. 2021;385(4):342-351.https://doi.org/10.1056/NEJMsa2034159
Mossey JM. Defining Racial and Ethnic Disparities in Pain Management. Clin Orthop. 2011;469(7):1859-1870. https://doi.org/10.1007/s11999-011-1770-9
Jena AB, Goldman D, Karaca-Mandic P. Hospital Prescribing of Opioids to Medicare Beneficiaries. JAMA Intern Med. 2016;176(7):990. https://doi.org/10.1001/jamainternmed.2016.2737
Dolin SJ, Cashman JN, Bland JM. Effectiveness of acute postoperative pain management: I. Evidence from published data. Br J Anaesth. 2002;89(3):409-423.
Kinney MAO, Hooten WM, Cassivi SD, et al. Chronic Postthoracotomy Pain and Health-Related Quality of Life. Ann Thorac Surg. 2012;93(4):1242-1247.https://doi.org/10.1016/j.athoracsur.2012.01.031
Herzig SJ, Anderson TS, Jung Y, Ngo LH, McCarthy EP. Risk Factors for Opioid-Related Adverse Drug Events Among Older Adults After Hospital Discharge. J Am Geriatr Soc. 2022;70(1):228-234.https://doi.org/10.1111/jgs.17453
Herzig SJ, Stefan MS, Pekow PS, et al. Risk Factors for Severe Opioid-Related Adverse Events in a National Cohort of Medical Hospitalizations. J Gen Intern Med. 2020;35(2):538-545.https://doi.org/10.1007/s11606-019-05490-w
Rambachan A, Fang MC, Prasad P, Iverson N. Racial and Ethnic Disparities in Discharge Opioid Prescribing from a Hospital Medicine Service. J Hosp Med. 2021;16(10):589-595. https://doi.org/10.12788/jhm.3667
Eicheldinger C, Bonito A. More accurate racial and ethnic codes for Medicare administrative data. Health Care Financ Rev. 2008;29(3):27-42.
Tools Archive for Elixhauser Comorbidity Software Refined for ICD-10-CM Healthcare Cost and Utilization Project (HCUP). Published October 2021. https://www.hcup-us.ahrq.gov/toolssoftware/comorbidityicd10/comorbidity_icd10_archive.jsp
Elixhauser Comorbidity Software, Version 3.7. Accessed July 3, 2022. https://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp
Von Korff M, Scher AI, Helmick C, et al. United States National Pain Strategy for Population Research: Concepts, Definitions, and Pilot Data. J Pain. 2016;17(10):1068-1080.https://doi.org/10.1016/j.jpain.2016.06.009
Mayhew M, DeBar LL, Deyo RA, et al. Development and Assessment of a Crosswalk Between ICD-9-CM and ICD-10-CM to Identify Patients with Common Pain Conditions. J Pain. 2019;20(12):1429-1445.https://doi.org/10.1016/j.jpain.2019.05.006
Kind AJH, Buckingham WR. Making Neighborhood-Disadvantage Metrics Accessible — The Neighborhood Atlas. N Engl J Med. 2018;378(26):2456-2458. https://doi.org/10.1056/NEJMp1802313
Kind AJH, Buckingham W. Making Neighborhood Disadvantage Metrics Accessible: The Neighborhood Atlas. New England Journal of Medicine, 2018. 378: 2456-2458. https://doi.org/10.1056/NEJMp1802313
Song M, Zhou X, Pazaris M, Spiegelman D. The Missing Covariate Indicator Method Is Nearly Valid Almost Always. Published online 2021. arXiv:2111.00138. https://doi.org/10.48550/ARXIV.2111.00138
Agency for Healthcare Research and Quality, Rockville, MD. Tools Archive for Clinical Classifications Software Refined. Healthcare Cost and Utilization Project (HCUP). Published March 2021. Accessed October 31, 2022. https://www.hcup-us.ahrq.gov/toolssoftware/ccsr/ccsr_archive.jsp
CDC Compilation of Benzodiazepines, Muscle Relaxants, Stimulants, Zolpidem, and Opioid Analgesics with Oral Morphine Milligram Equivalent Conversion Factors. National Center for Injury Prevention and Control; 2018. Accessed October 21, 2022. https://www.cdc.gov/opioids/data-resources/index.html
Williams R. Using the Margins Command to Estimate and Interpret Adjusted Predictions and Marginal Effects. Stata J Promot Commun Stat Stata. 2012;12(2):308-331.https://doi.org/10.1177/1536867X1201200209.
Anderson KO, Green CR, Payne R. Racial and Ethnic Disparities in Pain: Causes and Consequences of Unequal Care. J Pain. 2009;10(12):1187-1204.https://doi.org/10.1016/j.jpain.2009.10.002.
Bonham VL. Race, Ethnicity, and Pain Treatment: Striving to Understand the Causes and Solutions to the Disparities in Pain Treatment. J Law Med Ethics J Am Soc Law Med Ethics. 2001;29(1):52-68.https://doi.org/10.1111/j.1748-720x.2001.tb00039.x.
Hoffman KM, Trawalter S, Axt JR, Oliver MN. Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs About Biological Differences Between Blacks and Whites. Proc Natl Acad Sci. 2016;113(16):4296-4301. https://doi.org/10.1073/pnas.1516047113.
Schuler MS, Schell TL, Wong EC. Racial/Ethnic Differences in Prescription Opioid Misuse and Heroin Use Among a National Sample, 1999–2018. Drug Alcohol Depend. 2021;221:108588. https://doi.org/10.1016/j.drugalcdep.2021.108588.
Sahker E, Yeung CW, Garrison YL, Park S, Arndt S. Asian American and Pacific Islander Substance Use Treatment Admission Trends. Drug Alcohol Depend. 2017;171:1-8.https://doi.org/10.1016/j.drugalcdep.2016.11.022.
Funding
This work was funded by grant number R01HS026215 from the Agency for Healthcare Research and Quality. The funding agency had no role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of any of the funding agency.
Koushik Kasanagottu, MD, MPH, was funded by grant number T32HP32715 from the Health Resources and Services Administration. He is a general internal medicine fellow at Harvard Medical School and Beth Israel Deaconess Medical Center.
Timothy Anderson, MD, MAS, was funded by grant number K76AG074878 from the National Institute on Aging
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This project with preliminary data was presented at the Annual Society of General Internal Medicine (SGIM) Conference on 04/07/2022.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kasanagottu, K., Anderson, T.S., Trivedi, S. et al. Racial and Ethnic Disparities in Opioid Prescribing on Hospital Discharge Among Older Adults: A National Retrospective Cohort Study. J GEN INTERN MED 39, 1444–1451 (2024). https://doi.org/10.1007/s11606-024-08687-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-024-08687-w