Abstract
Background
Obesity may impact surgical outcomes of gastrectomy. Whether visceral fat area (VFA) is a better obesity parameter than body mass index (BMI) is still controversial. The aim of this study is to compare the accuracy and effectiveness of VFA and BMI in predicting the short-term surgical outcomes of gastrectomy.
Methods
Patients who were diagnosed with gastric cancer were measured for BMI and VFA preoperatively and then divided into a VFA-H (VFA-high) group and VFA-L (VFA-low) group, at the cutoff point of 100 cm2, and a BMI-H (BMI-high) group and BMI-L (BMI-low) group, at the cutoff point of 25 kg/m2. The short-term surgical outcomes were compared between the different groups.
Results
In total, 276 patients were enrolled in this study; 55 (19.9%) patients were classified into the BMI-H group, and 122 (44.2%) patients were classified into the VFA-H group. There was a significant correlation between BMI and VFA (r = 0.652, p < 0.001). Compared with the VFA-L group, the VFA-H group had a higher incidence of postoperative complications (31.1% vs. 13.0%; p < 0.001), longer operation duration (270.0 (235.0–305.0) vs. 255.0 (223.8–295.0), p = 0.046), and more blood loss (100.0 (100.0–150.0) vs. 80.0 (80.0–100.0), p < 0.001), while the BMI-H group had more blood loss than the BMI-L group (100.0 (100.0–120.0) vs. 100.0(80.0–100.0), p = 0.006). Logistic regression showed that VFA was an independent risk factor for postoperative complications (odds ratio 2.813, 95% CI 1.523–5.194; p = 0.001).
Conclusion
For gastric cancer patients, VFA is superior to BMI in accurately and effectively illuminating the impact of obesity on short-term surgical outcomes.
Trial Registration
Clinicaltrials.gov: NCT02800005.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Gastric cancer (GC) is one of the most common malignances worldwide.1 Even through the overall incidence of gastric cancer has been decreasing globally, it is still the second-leading cause of cancer-related mortality in China.2,3 D2 lymphadenectomy is widely performed in East Asia, and it is associated with a lower local-regional recurrence and better survival benefits.4,5,6 The high incidence of adiposity worldwide has become a severe problem.7,8 The obesity rate in China has risen to 11.9%,9 and China already has the largest obese population worldwide.10 Excessive adipose tissue makes the process of lymphadenectomy and the exposure of vital arteries more difficult and dangerous. Some previous studies have indicated the influence of adiposity on the operation, but the impact of obesity on surgical short-term outcomes is still contentious, as studies have reached different conclusions about obesity’s effect on such surgical outcomes as the effect on blood loss, number of retrieved lymph nodes, operative duration, and postoperative complications.11,12,13
Body mass index (BMI) is a commonly used parameter to assess obesity. However, it cannot perfectly measure the distribution of fat tissue, which differs greatly between individuals. Accordingly, visceral fat area (VFA) has been proposed to assess obesity and fat distribution. The development of computed tomography and data processing techniques has made the value of VFA more accurate and easier to determine. VFA can better indicate the visceral fat level and has a stronger correlation with surgical outcomes and postoperative complications.12,13,14 However, those retrospective studies did not reach a consensus about the impact of VFA on the surgical outcomes or whether VFA was a better obesity parameter than BMI.11,13,14,15,16
Therefore, we designed this single-center prospective cohort study to investigate the impact of obesity on surgical outcomes and to compare the accuracy and effectiveness of VFA and BMI on evaluating the short-term outcomes of gastrectomy.
Patients and Methods
Study Design and Ethics
This is a prospective cohort study with the aim to explore the impact of obesity on surgical outcomes and compare the accuracy and effectiveness of VFA and BMI on evaluating the short-term surgical outcomes of gastrectomy. The primary endpoint was postoperative complications. This trial was registered on clinicaltrials.gov with the identifier, NCT02800005.17 The study protocol was approved by the Biomedical Ethical Committee of West China Hospital, Sichuan University (2015, no.123). The participants were fully informed and gave written informed consent.
Patients and Cohort Development
The inclusion criteria of this study were (1) age ≥ 18 years and ≤ 75 years; (2) preoperative endoscopy and biopsy confirmed gastric adenocarcinoma, and predicted feasible total gastrectomy or subtotal gastrectomy; (3) predicted resectable diseases of preoperative staging T1N0M0-T4aN+M0, Ia-IIIc stage; (4) no other primary malignancy; and (5) agreement to participate in the trial and written informed consent. The exclusion criteria of this study were patients who (1) were treated with neoadjuvant chemotherapy or radiation therapy, which might affect the efficacy observation; (2) were not eligible for gastrectomy due to severe dysfunction of other organs; or (3) decided not to participate in the trial after signing the informed consent.
From April 2015 to December 2017, a total of 300 patients were included. VFA and BMI were calculated preoperatively. Nine patients were excluded because they did not accept the operation, 10 patients were excluded because they underwent laparoscopic exploration only, and 5 patients were excluded because they had palliative surgery. Ultimately, 276 patients were enrolled for statistical analysis (Fig. 1).
Fat Measurement
All included patients underwent abdominal computed tomography (CT) as a preoperative evaluation. VFA and subcutaneous fat area (SFA) were measured using a cross-sectional image from CT imaging of the abdomen at the umbilicus level. On CT scans, adipose tissue was determined by setting the attenuation level within the range of − 190 to − 30 Hounsfield units (HU).18
By tracing the outline of the visceral fat tissue and the contour of the subcutaneous fat tissue, the Fat Scan software calculated the VFA and SFA, respectively (Fig. 2). The patients were classified into two groups: the VFA-L group, with VFA < 100 cm2, and the VFA-H, with VFA ≥ 100 cm2, according to the recommended VFA cutoff from the Japan Society for the Study of Obesity.19 According to the World Health Organization (WHO), people with a BMI higher than 30 kg/m2 are treated as obese. However, considering different body shapes and fat distributions between different ethnic populations, we adopted the Asian-Pacific standard, and all the patients were classified into a BMI-H (BMI ≥ 25 kg/m2) group and a BMI-L (BMI < 25 kg/m2) group.20
Surgical Procedure and Short-term Surgical Outcomes
The operations of all enrolled patients were performed by an experienced surgeon with rich experience in performing both laparoscopic-assisted gastrectomy (LAG) and open gastrectomy (OG). The resection pattern of distal or total gastrectomy depended on the site of the stomach tumor. For the enrolled people, standard D2 lymphadenectomy was performed according to the treatment guidelines of the Japanese Gastric Cancer Association (JGCA).21 Intraoperative frozen sections of resection margins were examined to ensure R0 resection. Billroth-1 and Billroth-2 anastomoses were commonly used for distal gastrectomy, while Roux-en-Y anastomosis was selectively performed. Esophago-jejunal Roux-en-Y anastomosis was performed after total gastrectomy.
Operation duration, intraoperative blood loss, number of retrieved lymph nodes, postoperative hospital stays, and postoperative complications were recorded as short-term surgical outcomes. In addition, complications were further classified according to the Clavien-Dindo surgical complication grading system.22
Statistical Analysis
All statistical analyses were performed with the statistical software SPSS 20.0 (SPSS®, Chicago, IL, USA). Two-sided p values less than 0.05 were considered significant. Variables are expressed as median with interquartile range. In analyzing baseline characteristics and comparing the surgical outcomes of different groups, the chi-square test was used to analyze unordered categorical variables. Ranked data were analyzed by the rank sum test (Mann-Whitney U test). Student’s t test was used to analyze continuous data if homogeneity of variance and normal distribution were satisfied. Spearman’s rank correlation was used to evaluate relationships between individual fat parameters. A logistic regression model was used to evaluate the risk factors for postoperative complications.
Results
Patients’ Characteristics
A total of 276 patients were enrolled for statistical analysis. The comparison of characteristics between different cohorts are shown in Table 1, and the characteristics of all the patients are shown in Supplemental Table 1.The median of BMI was 22.5 kg/m2 (interquartile range, 20.2–24.5). Fifty-five (19.9%) patients were classified into the BMI-H group, and 221 (80.1%) were classified into the BMI-L group. The median of VFA was 88.4 cm2 (interquartile range, 50.6–131.6). One hundred twenty-two (44.2%) patients were classified into the VFA-H group, and 154 (55.8%) were classified into the VFA-L group. There was no significant difference in age, gender, tumor size, tumor location, or tumor stage between the VFA-H and VFA-L groups or BMI-H and BMI-L groups.
Distribution and Correlations of Fat Parameters
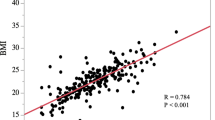
The distribution of fat tissue differs between individuals.23 As indicated in Fig. 2, two patients with almost the same BMI had a dramatically different VFA and SFA. The female patients had more subcutaneous fat than male patients (159.3 (99.2–200.3) vs. 99.1 (55.2–145.6), p < 0.001), while no significant difference was seen in visceral fat. In the male subgroup, the BMI-H group had a lower SFA/VFA ratio than the BMI-L group (0.9 (0.8–1.3) vs. 1.1 (0.9–1.6), p = 0.038), which indicated that BMI-H male patients were more likely to have more visceral fat tissue than subcutaneous fat tissue, which aligns with a previous study.24 Correlation analysis showed significant correlations between BMI and VFA (r = 0.652; p < 0.001), BMI and SFA (r = 0.565; p < 0.001), and SFA and VFA (r = 0.684; p < 0.001).
Short-term Surgical Outcomes
Compared with the VFA-L group, the VFA-H group had a significantly higher incidence of postoperative complications (31.1% vs. 13.0%; p < 0.001), longer operation duration (270.0 (235.0–305.0) vs. 255.0 (223.8–295.0), p = 0.046) and more blood loss (100.0 (100.0–150.0) vs. 80.0 (80.0–100.0), p < 0.001), and longer postoperative hospital stays (9.0 (8.0–11.0) vs. 8.0 (8.0–9.0), p = 0.045), while BMI-H group had more blood loss than the BMI-L group (100.0 (100.0–120.0) vs. 100.0 (80.0–100.0), p < 0.001) (Table 2). With standard D2 lymphadenectomy, the number of retrieved lymph nodes showed no significant difference between the VFA-H and VFA-L groups (p = 0.154) or the BMI-H and BMI-L groups (p = 0.652).
Complications were described according to the international consensus on complications after gastrectomy25 (Table 3). Then, the postoperative complications were classified with the Clavien-Dindo classification criteria. VFA-H group had a higher incidence of Clavien-Dindo class I and class II complications than the VFA-L group (30.3% vs. 11.7%; p = 0.001) (Table 2).
In the laparoscopic-assisted gastrectomy subgroup, the VFA-H group (n = 35) had a higher incidence of postoperative complications than the VFA-L group (n = 72) (34.3% vs. 9.7%; p = 0.003) and longer operation duration (300.0 (275.0–335.0) vs. 278.5 (235.0–305.0), p = 0.004). No significant difference was seen in blood loss (p = 0.192) or the number of harvested lymph nodes (p = 0.865).
Among the BMI-L group, 33.9% (n = 75) of patients had high VFA (VFA ≥ 100 cm2), and 66.1% (n = 146) of patients had low VFA (VFA < 100 cm2). The VFA-H subgroup had a longer operation duration (275.0 (245.0–310.0) vs. 252.5 (223.8–295.0), p = 0.011), a higher rate of postoperative complications (32.0% vs. 12.3%; p = 0.001) and more blood loss (80.0 (80.0–150.0) vs. 80.0(80–100.0), p < 0.001), but the number of retrieved lymph nodes did not show a significant difference (p = 0.213) (Supplemental Table 2).
Risk Factors for Postoperative Complications
Table 4 shows the results of univariate and multivariate analysis to identify risk factors for postoperative complications. On the basis of univariate analysis, VFA and operation duration were the factors associated with the development of postoperative complications. Multivariate analysis revealed that VFA (p = 0.001) and operation duration (p = 0.028) were independent risk factors, with ORs (95% confidence intervals) of 2.813 (1.523–5.194) and 1.006 (1.001–1.011), respectively.
Discussion
Some previous retrospective studies have explored the relationship between VFA and BMI and the impact of excessive abdominal fat tissue on surgical outcomes. However, whether VFA is a better parameter than BMI is still controversial. We designed this prospective cohort study with the aim of providing a relatively high level of evidence to investigate the impact of obesity on surgical outcomes and to compare the accuracy and effectiveness of VFA and BMI on evaluating the short-term outcomes of gastrectomy. As far as we know, this is the first prospective cohort study focusing on this contentious question.
We found significant positive correlations between different pairs of fat parameters, such as VFA and BMI, SFA and BMI, and VFA and SFA, in line with previous studies.11,12 Approximately 14.5% of high-BMI (BMI ≥ 25 kg/m2) patients had low VFA (VFA < 100 cm2), and 33.9% of low-BMI (BMI < 25 kg/m2) patients had high VFA (VFA ≥ 100 cm2), which aligns with the report from Yoshikawa that 33.3% of low-BMI (< 25 kg/m2) patients had high VFA (≥ 100 cm2).14 In the BMI-L group, the VFA-H subgroup had a higher incidence of postoperative complications, longer operation duration, and more blood loss than the VFA-L subgroup. The BMI-L group accounted for 80.1% of the enrolled patients. Therefore, for low-BMI (< 25 kg/m2) patients, VFA can better predict surgical outcomes, and calculating VFA preoperatively is of great significance, especially for low-BMI patients.
Gastrectomy with D2 lymphadenectomy is widely performed in East Asia, as it has been associated with a lower local-regional recurrence and better survival benefit. The National Comprehensive Cancer Network (NCCN) guidelines for gastric cancer suggest that the removal of at least 15 lymph nodes is recommended.26 In this study, among all the enrolled cases, the median of retrieved lymph nodes was 36.0 (interquartile range, 27.0–46.0). We found that there was no significant difference between the number of retrieved lymph nodes in the VFA-H and VFA-L groups or the BMI-H and BMI-L groups. The dissection of lymph nodes is a difficult part of gastrectomy, and excessive visceral fat can increase the difficulty, maybe causing insufficient lymphadenectomy. The standard D2 lymphadenectomy can improve the survival outcomes of gastric cancer patients.27 In our medical center, we follow a series of strict quality control strategies, strictly defining the standard of D2 lymphadenectomy, and the surgical outcome indicates that by using these quality control strategies, we can avoid the impact of excessive visceral fat and achieve a standard D2 lymphadenectomy.
Due to the complexity and difficulty of radical surgery of gastric cancer (D2 lymph node dissection), postoperative complications have a high incidence, according to the results of some high quality RCTs from Japan and Korea,28,29,30,31,32 the incidence of postoperative complications after gastrectomy ranged from 10 to 30%, and respiratory infections was a common postoperative complication. In this study, the postoperative general complications of VFA-H group were higher than the VFA-L group (20.5% vs. 5.8%). The postoperative surgical complications of VFA-H group were also higher than the VFA-L group (10.7% vs. 7.1%). 10.5% of all patients had respiratory infections; the VFA-H group had a significant higher proportion than the VFA-L group (16.4% vs. 5.8%). Thus, for high VFA patients, we need to take effective measures to avoid respiratory infections during the perioperative time.
Laparoscopic distal gastrectomy has been recommended as an optimal treatment for cStage-I gastric cancer by the JGCA.21 Several ongoing trials are assessing the safety and feasibility of laparoscopic total gastrectomy and laparoscopic gastrectomy for advanced GC.33,34,35 We also investigated the impact of obesity on surgical outcomes in the laparoscopic gastrectomy subgroup, revealing that the VFA-H group had longer operation duration and a higher incidence of postoperative complications, but no difference was seen in blood loss or the number of harvested lymph nodes. Excessive visceral fat tissue increased the difficulty of laparoscopic-assisted gastrectomy, maybe because the excessive visceral fat tissue made the narrow cavity more crowded, resulting in longer operation duration. However, magnified laparoscopic images helped the surgeons perform operations more accurately, and excessive visceral fat tissue did not result in more blood loss in laparoscopic-assisted gastrectomy.
BMI is widely used to evaluate the degree of obesity, and it is a simple and easy index to use, but it cannot evaluate the distribution of fat tissue. VFA can directly reveal visceral fat tissue, which may have a larger effect on gastrectomy and lymphadenectomy outcomes than subcutaneous fat tissue. In the present study, VFA had a stronger correlation with short-term surgical outcomes than BMI, and the volume of blood loss of the VFA-H group was larger, the operation duration was longer, and the postoperative complication rate was higher.
Compared with BMI, the calculation of VFA is more complex. While an abdominal CT scan is taken as common test for preoperative evaluation, the development of software technology will make VFA measurements easier. Thus, VFA can be recommended as a routine test for gastric cancer patients, especially for low-BMI patients.
This study had some limitations. It was a single-center study, and most of the patients came from Southwest China, so the data may not represent patients from other areas well, and body shape is inherently different between locations and races, so our results need to be validated by further studies from other medical centers.
Conclusion
VFA had more sensitive correlations with short-term surgical outcomes than BMI. For gastrectomy, high VFA caused more blood loss, longer operation duration, and higher incidence of postoperative complications. By following strict quality control strategies, VFA does not affect the number of harvested lymph nodes. VFA is recommended to predict perioperative risk for gastric cancer patients, especially low-BMI patients. More attention needs to be paid to high-VFA patients during the perioperative period.
References
Van Cutsem, E., X. Sagaert, B. Topal, et al., Gastric cancer. Lancet, 2016. 388(10060): p. 2654–2664.
Chen, W., R. Zheng, P.D. Baade, et al., Cancer statistics in China, 2015. CA Cancer J Clin, 2016. 66(2): p. 115–32.
Torre, L.A., F. Bray, R.L. Siegel, et al., Global cancer statistics, 2012. CA Cancer J Clin, 2015. 65(2): p. 87–108.
Songun, I., H. Putter, E.M. Kranenbarg, et al., Surgical treatment of gastric cancer: 15-year follow-up results of the randomised nationwide Dutch D1D2 trial. Lancet Oncol, 2010. 11(5): p. 439–49.
Degiuli, M., M. Sasako, A. Ponti, et al., Survival results of a multicentre phase II study to evaluate D2 gastrectomy for gastric cancer. Br J Cancer, 2004. 90(9): p. 1727–32.
Sasako, M., T. Sano, S. Yamamoto, et al., D2 lymphadenectomy alone or with para-aortic nodal dissection for gastric cancer. N Engl J Med, 2008. 359(5): p. 453–62.
Perez Rodrigo, C., Current mapping of obesity. Nutr Hosp, 2013. 28 Suppl 5: p. 21–31.
Ogden, C.L., M.D. Carroll, B.K. Kit, et al., Prevalence of childhood and adult obesity in the United States, 2011-2012. Jama, 2014. 311(8): p. 806–14.
The Chinese National Health and Family Planning Commission. The Nutrition and Health Status of the Chinese People (2015 Report). Available at http://mp.weixin.qq.com/s?__biz=MjM5OTIyODc1NA==&mid=205782183&idx=1&sn=12d59495ff4866ffa0d92023e4efc40e&scene=1#rd (accessed on 23 July, 2016). 401(6): p. 823–8.
Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. The Lancet, 2016. 387(10026): p. 1377–1396.
Kim, J.H., H.M. Chin, S.S. Hwang, et al., Impact of intra-abdominal fat on surgical outcome and overall survival of patients with gastric cancer. Int J Surg, 2014. 12(4): p. 346–52.
Sugisawa, N., M. Tokunaga, Y. Tanizawa, et al., Intra-abdominal infectious complications following gastrectomy in patients with excessive visceral fat. Gastric Cancer, 2012. 15(2): p. 206–12.
Takeuchi, M., K. Ishii, H. Seki, et al., Excessive visceral fat area as a risk factor for early postoperative complications of total gastrectomy for gastric cancer: a retrospective cohort study. BMC Surg, 2016. 16(1): p. 54.
Yoshikawa, K., M. Shimada, N. Kurita, et al., Visceral fat area is superior to body mass index as a predictive factor for risk with laparoscopy-assisted gastrectomy for gastric cancer. Surg Endosc, 2011. 25(12): p. 3825–30.
Watanabe, J., K. Tatsumi, M. Ota, et al., The impact of visceral obesity on surgical outcomes of laparoscopic surgery for colon cancer. Int J Colorectal Dis, 2014. 29(3): p. 343–51.
Go, J.E., M.C. Kim, K.H. Kim, et al., Effect of visceral fat area on outcomes of laparoscopyassisted distal gastrectomy for gastric cancer: subgroup analysis by gender and parameters of obesity. Ann Surg Treat Res, 2015. 88(6): p. 318–24.
Effect of Obesity on Surgical Outcomes and Survival for Gastric Cancer;https://clinicaltrials.gov/ct2/show/NCT02800005?cond=gastric+cancer&cntry=CN&city=Chengdu&rank=2. 10 Jul 2018
Clark, W., E.M. Siegel, Y.A. Chen, et al., Quantitative measures of visceral adiposity and body mass index in predicting rectal cancer outcomes after neoadjuvant chemoradiation. J Am Coll Surg, 2013. 216(6): p. 1070–81.
New criteria for 'obesity disease' in Japan. Circ J, 2002. 66(11): p. 987–92.
The Asia Pacific Perspective: Redefining Obesity and its Treatment. Melbourne [Internet], International Diabetes Institute, 2000.
Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer, 2017. 20(1): p. 1–19.
Dindo, D., N. Demartines, and P.A. Clavien, Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg, 2004. 240(2): p. 205–13.
Karastergiou, K., The Interplay Between Sex, Ethnicity, and Adipose Tissue Characteristics. Curr Obes Rep, 2015. 4(2): p. 269–78.
Bouchi, R., T. Takeuchi, M. Akihisa, et al., High visceral fat with low subcutaneous fat accumulation as a determinant of atherosclerosis in patients with type 2 diabetes. Cardiovasc Diabetol, 2015. 14: p. 136.
S, G., M. D, R. D, et al., International consensus on a complications list after gastrectomy for cancer.%A Baiocchi GL. Gastric cancer : official journal of the International Gastric Cancer Association and the Japanese Gastric Cancer Association, 2018. undefined(undefined): p. undefined.
Ajani, J.A., T.A. D'Amico, K. Almhanna, et al., Gastric Cancer, Version 3.2016, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw, 2016. 14(10): p. 1286–1312.
Yang, K., Y.Y. Choi, W.H. Zhang, et al., Strategies to improve treatment outcome in gastric cancer: a retrospective analysis of patients from two high-volume hospitals in Korea and China. Oncotarget, 2016. 7(28): p. 44660–44675.
HJ, L., H. WJ, Y. HK, et al., Short-term Outcomes of a Multicenter Randomized Controlled Trial Comparing Laparoscopic Distal Gastrectomy With D2 Lymphadenectomy to Open Distal Gastrectomy for Locally Advanced Gastric Cancer (KLASS-02-RCT). Annals of surgery, 2019. undefined(undefined): p. undefined.
Kim W, K.H., Han SU, et al; Korean Laparo―endoscopic and G.S.S.K. Group., Decreased Morbidity of Laparoscopic Distal Gastrectomy Compared With Open Distal Gastrectomy for Stage I Gastric Cancer: Short-term Outcomes From a Multicenter Randomized Controlled Trial (KLASS―01)[J]. Ann Surg 2016. 263(1):28―35. https://doi.org/10.1097/SLA.0000000000001346.
Sano, T., M. Sasako, S. Yamamoto, et al., Gastric cancer surgery: morbidity and mortality results from a prospective randomized controlled trial comparing D2 and extended para-aortic lymphadenectomy--Japan Clinical Oncology Group study 9501. J Clin Oncol, 2004. 22(14): p. 2767–73.
Sasako, M., T. Sano, S. Yamamoto, et al., Left thoracoabdominal approach versus abdominal-transhiatal approach for gastric cancer of the cardia or subcardia: a randomised controlled trial. Lancet Oncol, 2006. 7(8): p. 644–51.
Katai, H., J. Mizusawa, H. Katayama, et al., Short-term surgical outcomes from a phase III study of laparoscopy-assisted versus open distal gastrectomy with nodal dissection for clinical stage IA/IB gastric cancer: Japan Clinical Oncology Group Study JCOG0912. Gastric Cancer, 2017. 20(4): p. 699–708.
Kataoka, K., H. Katai, J. Mizusawa, et al., Non-Randomized Confirmatory Trial of Laparoscopy-Assisted Total Gastrectomy and Proximal Gastrectomy with Nodal Dissection for Clinical Stage I Gastric Cancer: Japan Clinical Oncology Group Study JCOG1401. J Gastric Cancer, 2016. 16(2): p. 93–7.
Hu, Y., C. Huang, Y. Sun, et al., Morbidity and Mortality of Laparoscopic Versus Open D2 Distal Gastrectomy for Advanced Gastric Cancer: A Randomized Controlled Trial. J Clin Oncol, 2016. 34(12): p. 1350–7.
Hur, H., H.Y. Lee, H.J. Lee, et al., Efficacy of laparoscopic subtotal gastrectomy with D2 lymphadenectomy for locally advanced gastric cancer: the protocol of the KLASS-02 multicenter randomized controlled clinical trial. BMC Cancer, 2015. 15: p. 355.
Acknowledgments
The authors thank the valuable work of the Volunteer Team of Gastric Cancer Surgery (VOLTGA) West China Hospital, Sichuan University, China, for the establishment and updating of the gastric cancer database.
Funding
This study is supported by grants of National Natural Science Foundation of China, No.81301866; Sichuan Province Youth Science Technology Innovative Research Team, No.2015TD0009; 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (ZY2017304); Fund for Fostering Academic and Technical Leaders of Sichuan Province, No. [2017]919; and Foundation of Science & Technology Department of Sichuan Province (No. 2018SZ0147).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Supplementary Table 1
(DOCX 16 kb)
Supplementary Table 2
(DOCX 16 kb)
Rights and permissions
About this article
Cite this article
Yang, Sj., Li, Hr., Zhang, Wh. et al. Visceral Fat Area (VFA) Superior to BMI for Predicting Postoperative Complications After Radical Gastrectomy: a Prospective Cohort Study. J Gastrointest Surg 24, 1298–1306 (2020). https://doi.org/10.1007/s11605-019-04259-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04259-0