Abstract
Background
No studies have yet analyzed the characteristics of recurrence after resection for intraductal papillary neoplasm of bile duct (IPNB) based on tumor location. We analyzed the patterns, timing, and risk factors for recurrence.
Methods
From 1994 to 2014, data from 103 patients who were diagnosed with IPNB were retrospectively reviewed. Among these, 44 were extrahepatic IPNB (E-IPNB) and 59 were intrahepatic IPNB (I-IPNB).
Results
CK20, pancreaticobiliary type, tumor invasion beyond ductal wall, tumor invasion to adjacent organs, and invasive disease were more frequently found in E-IPNB than in I-IPNB (22.7 vs. 8.5%; p = 0.043, 38.6 vs. 23.7%; p = 0.050, 20.5 vs. 11.9%; p < 0.001, 4.5 vs. 1.7%; p < 0.001 and 93.2 vs. 55.9%; p < 0.001). E-IPNB has poorer 5-year recurrence-free survival (RFS) compared to I-IPNB (51.7 vs. 91.4%; p < 0.001). There was no significant difference in the rate of initial isolated locoregional recurrence and initial distant recurrence according to tumor location (14.6 in E-IPNB vs. 3.0% in I-IPNB; p = 0.123, 19.5 in E = IPNB vs. 12.0% in I-IPNB; p = 0.136). Recurrence rate according to timing was different between E-IPNB and I-IPNB: within 1 year (33.3% vs. 83.3%; p = 0.061) and 1–3 years (50.0% vs. 0%; p = 0.052). The independent prognostic factors for RFS were tumor location (p = 0.034) and lymph node metastasis (p = 0.013).
Conclusions
E-IPNB has a worse prognosis than I-IPNB. Different follow-up schedules for surveillance according to tumor location are needed after surgery.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Intraductal papillary neoplasm of the bile duct (IPNB) is a rare tumor with a wide disease spectrum ranging from benign to malignant conditions. IPNB shows an exophytic growth pattern throughout the biliary tract. Compared with intraductal papillary mucinous neoplasm of the pancreas (IPMN), IPNB is more frequently associated with invasive disease.1,2 Previous studies reported that the 5-year survival rate ranges from 46 to 76%2,3,4,5,6,7,8 and that the recurrence rate ranges from 13 to 29%.3,8,9,10,11 Only a few studies have analyzed the patterns of recurrence after resection9,12,13,14 and prognostic factors for the recurrence of IPNB.5,12,15
However, no studies have been conducted to investigate the clinical characteristics of recurrence according to tumor location. The primary goal of this study was to determine whether tumor location could lead to differences in the risk and timing of recurrence. This can be important in that it can guide customized treatment and surveillance options through prognostic stratification. In this regard, we investigate the recurrence pattern and timing based on tumor location. In addition, identification of the risk factors for time to recurrence and recurrence-free survival (RFS) was performed.
Methods
Patient Selection
From 1994 to 2014, consecutive data from 103 patients who were diagnosed with IPNB after surgery were prospectively collected and retrospectively reviewed from electronic medical records. One pathologist (Jang K.T.) with extensive experience in hepato-biliary disease confirmed all the reports and findings of these 103 cases.
Preoperative Evaluation
For preoperative diagnosis, image work-up was routinely performed. Typical image findings, obtained by abdominal computed tomography (CT), magnetic resonance cholangiopancreatography (MRCP), and/or endoscopic retrograde cholangiopancreatography (ERCP), revealed cystic or tubular dilatations of the bile duct combined with an intraductal mass or mucobilia. However, some cases did not show typical image findings. Given these, we enrolled the patients according to final pathology.
Tumor Location and Surgical Procedures
The surgical strategy was firstly established at the preoperative multidisciplinary meeting, and ultimately, it was determined by confirming the extent of the tumor invasion grossly during the operation. Bile duct resection was performed when the proximal part of tumor was located in an extrahepatic duct but did not invade the hepatic confluence. When the tumor was present in the intrahepatic duct or invaded the confluence of the hilar portion, liver resection was performed. Pancreaticoduodenectomy (PD) was performed when the distal part of tumor extends intrapancreatic portion of bile duct.
The tumor location was defined as the location identified in the surgical specimen. Extrahepatic IPNB (E-IPNB) was defined as the tumor located at hilar portion or distal bile duct. If the center of the tumor mass is in the liver and is present between the left side of the right posterior portal vein and the right side of the umbilical portion of the left portal vein, we classified it as E-IPNB.16 Intrahepatic IPNB (I-IPNB) was defined as the intrahepatic tumor not involving hilar portion.
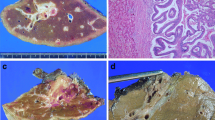
Pathological Assessment of IPNB
According to previous reports,3,17,18,19,20,21,22,23 IPNB was defined as a biliary neoplasm with an exophytic nature showing papillary mass within the biliary tree, including both intrahepatic and extrahepatic bile ducts. It contains microscopic papillary fronds with fine vascular cores. Based on macroscopic appearance, the entire IPNB was divided into protruding IPNB and diffuse IPNB. The former was defined as a grossly visible polypoid mass or sessile mass on the specimen, and the latter was defined as a case in which the papillary tumor was seen to extend diffusely along the bile duct. Tumors were considered as “multifocal” if more than two discrete tumors were present upon gross inspection. If all lesions are present in the intrahepatic duct except the hilar portion, it is classified as I-IPNB. In contrast, if any of the lesions were present in the hilar portion, they were classified as E-IPNB. Invasive IPNB was defined as malignant tumor cells invading bile duct and/or adjacent structures but excluding carcinoma in situ. The depth of invasion is divided into three categories as follows: (i) tumor within duct—tumor cell confined to the ductal wall; (ii) tumor invasion beyond ductal wall—tumor passes through the bile duct and invades the periductal soft tissue but does not invade the surrounding hepatic parenchyma or adjacent organ or vascular structures; and (iii) tumor invasion to adjacent organ—tumor penetrates the bile duct and invades the surrounding hepatic structures or adjacent organs.
Follow-up After Surgery and Diagnosis of Recurrence
After the operation, the follow-up test was performed once every 3 months for the first 12 months. This included laboratory testing, including CA19-9 testing and imaging examinations such as chest X-ray, abdominal CT, and MRCP. Follow-up after 12 months was performed at least every 6 months. During this period, history taking, laboratory test, and abdominal CT were performed in outpatient clinic. There was no established indication and regimen for adjuvant concurrent chemoradiation therapy in this study. Fluorouracil, gemcitabine, or cisplatin-based chemotherapy regimen was used depending on the oncologist’s preference.
Recurrence was determined by abdominal CT or biopsy. The locoregional recurrence was defined as a newly developed lesion at the (1) bilioenteric anastomotic site, liver hilum, common bile duct remnant, or hepatic resection margin or (2) lymph node (LN) around previous surgical area, including hepatoduodenal ligament. All other recurrences were classified as distant metastases. Recurrence at LN around common hepatic artery (CHA), celiac trunk, and superior mesenteric artery/vein (SMA/SMV) were classified as distant metastases. Analysis of the recurrence rate and pattern was based only on the initial site of recurrence. When two or more sites were confirmed concurrently, they were regarded as overlapping sites.
Statistical Analyses
Chi-square and Fisher’s exact test were used to compare categorical variables. Student’s t test and Mann–Whitney test were used for continuous variables. In univariable analysis, p < 0.1 was considered to be significant. Parameters with p < 0.1 were included in a multivariable Cox proportional hazards regression analysis to identify the risk factors for recurrence. Statistical significance was indicated at p < 0.05 in multivariate analysis. To calculate the overall survival rates and cumulative probability of recurrence, Kaplan–Meier curves were constructed, and each survival curve was compared using the log-rank test. Statistical analyses were performed using the PASW Statistics version 23.0 (SPSS, IBM corp., Armonk, NY, USA).
Results
Demographic and Clinicopathological Features According to Tumor Location (All 103 IPNBs)
Among 103 patients, 49 were males and 54 were females with a median age of 64 years. Forty-four were diagnosed as E-IPNB and 59 were diagnosed as I-IPNB. R0 resection was done in 99 (96.1%). The size of tumor was smaller in E-IPNB than in I-IPNB (3.3 ± 2.3 cm vs. 5.5 ± 4.9 cm; p = 0.009). The mean value of total bilirubin (T.Bil), alanine aminotransferase (ALT), and aspartate aminotransferase (AST) were higher in E-IPNB than in I-IPNB (1.5 ± 1.4 vs. 0.8 ± 0.5 mg/mL; p = 0.006, 53.3 ± 60.3 vs. 24.7 ± 21.0 U/L; p < 0.001 and 62.5 ± 102.9 vs. 28.7 ± 22.3 U/L; p = 0.004). Among 44 cases of E-IPNB, 1 case (2.3%) of low or intermediate grade dysplasia, 2 cases (6.8%) of high-grade dysplasia, and 41 cases (93.2%) of invasive IPNB were observed. In 59 cases of I-IPNB, low or intermediate grade dysplasia was observed in 23 cases (39.0%), high-grade dysplasia in 3 cases (5.1%), and invasive IPNB in 33 cases (59.9%). CK20, pancreaticobiliary type, tumor invasion beyond ductal wall, tumor invasion to adjacent organs, and invasive disease were more frequently found in E-IPNB than in I-IPNB (22.7 vs. 8.5%; p = 0.043, 38.6 vs. 23.7%; p = 0.050, 20.5 vs. 11.9%; p < 0.001, 4.5 vs. 1.7%; p < 0.001 and 93.2 vs. 55.9%; p < 0.001).
Among the 59 I-IPNBs, 31 occurred at left lobe and 21 occurred at right lobe. There was significant difference in proportion of patients undergoing extrahepatic bile duct resection and major hepatectomy between E-IPNB versus I-IPNB (97.7% vs. 10.2%; p < 0.001 and 56.8% vs. 64.4%; p < 0.001). Among the 44 E-IPNBs, 8 (18.2%) patients underwent bile duct resection with hepaticojejunostomy and 10 patients (22.7%) underwent PD. Among 59 I-IPNBs, segmentectomy, bisementectomy, and major hepatectomy were performed in 4 (6.8%), 14 (23.7%), and 40 (67.8%) patients, respectively.
Demographic and Clinicopathological Features According to Tumor Location (74 Invasive IPNBs)
We performed further analysis of invasive IPNB by tumor location and summarized it in Table 1. The size of tumor was significantly smaller in E-IPNB than I-IPNB (3.3 ± 2.4 vs. 3.5 ± 2.6; p = 0.009). The mean values of T.bil, ALT, AST, and CA19-9 were significantly higher in E-IPNB than I-IPNB (1.6 ± 1.4 vs. 0.8 ± 0.6 mg/mL; p = 0.008, 53.8 ± 63.5 vs. 26.6 ± 23.8 U/L; p < 0.001, 48.8 ± 54.0 vs. 29.1 ± 19.5 U/L; p = 0.030 and 76.7 ± 145.3 vs. 50.6 ± 190.9 U/L; p = 0.054). Although no significant difference was found, tumor multiplicity, MUC1, lymph node metastasis, and positive resection margins occurred more frequently in E-IPNB than in I-IPNB (90.2 vs. 78.8%; p = 0.201, 24.4 vs. 18.2%; p = 0.519, 9.8 vs. 6.1%; p = 0.563 and 7.3 vs. 3.0%; p = 0.624).
Clinical Outcomes
The median follow-up time of all enrolled patients was 52 (1–185) months. Following resection, concurrent chemoradiation therapy (CCRT) was performed in three E-IPNBs and chemotherapy in one I-IPNB. The 5-year overall survival (OSR) and disease-free survival (DFS) rates of all 103 cases were 80.8% and 75.2%, respectively (Fig. 1a, b). Figure 1c, d shows significant difference in 5-year OSR and DFS between E-IPNB and I-IPNB (68.6 vs. 89.0%; p = 0.009, 51.7 vs. 91.4%; p < 0.001). Regarding 74 cases diagnosed as invasive IPNB, the 5-year recurrence rate in E-IPNB and I-IPNB was found to be 51.2% and 15.2%, respectively (p = 0.033).
Time to Initial Recurrence
Among the 74 cases diagnosed as invasive IPNB, recurrences occurred in 24 (32.4%) patients. The estimated cumulative probability of recurrence is shown in Fig. 2a. Among the 24 patients with recurrence, 11 (45.8%) experienced recurrence within 1 year, 20 (83.3%) within 3 years, and 23 (95.8%) within 5 years.
The cumulative probability of recurrence in E-IPNB was significantly higher than in I-IPNB (51.2% vs. 15.2%; p = 0.033) (Fig. 2b). Among the 24 patients with recurrence, there was difference in the recurrence rate within 1 year between the E-IPNB and I-IPNB with marginal significance (33.3% vs. 83.3%; p = 0.061). The recurrence rate during the follow-up period ranging from 1 to 3 years between the E-IPNB and I-IPNB was also different (50% vs. 0%; p = 0.052). There was no significant difference between recurrence rates of E-IPNB and I-IPNB during the follow-up period ranging from 3 to 5 years (16.7% vs. 16.7%; p = 0.749).
Among 18 E-IPNBs with recurrence, six (33.3%) experienced recurrence within 1 year, 15 (83.3%) within 3 years, and 18 (100%) within 5 years. Of six I-IPNBs with recurrence, five (83.3%) experienced recurrence within 1 year. The remaining one patient experienced recurrence 67 months (5.6 years) after surgery. Among five recurred I-IPNB patients within a year, there were one (20%) patient with tumor multiplicity, three (60%) patients with MUC1, two (40%) patients with lymph node metastasis, and one (20%) patient with positive resection margins. Regarding tumor markers such as CA19-9, the value for each of the five patients was lower than the average of 33 invasive I-IPNBs, 50.6 ± 190.9 U/mL. Invasion beyond ductal wall and macroscopically diffuse type IPNBs were found in four (80%) patients, respectively. Contrary to the results of invasive I-IPNB, all six cases with early recurrence within 1 year of invasive E-IPNB were protruding IPNB.
Analysis of Initial Recurrence Site
Table 2 presents the initial recurrence site in 74 cases diagnosed as invasive IPNB. There was no significant difference in the rate of initial isolated locoregional recurrence and initial distant recurrence according to tumor location (14.6 in E-IPNB vs. 3.0% in I-IPNB; p = 0.123, 19.5 in E = IPNB vs. 12.0% in I-IPNB; p = 0.136).
Of the 24 patients with recurrence, no significant difference in the median time to recurrence was found between patients with isolated locoregional recurrence and those with distant recurrence (21.0 vs. 7.0 months; p = 0.496).
PRS
The 1-, 2-, and 3-year post-recurrence survival (PRS) rates were 67.8%, 26.1%, and 26.1%, respectively, and the median PRS time was 16.0 months. After diagnosis of recurrence, one (14.3%) of the seven patients with isolated locoregional recurrence and six (60.0%) of the 12 patients with distant recurrence underwent palliative chemotherapy. Median PRS time was not significantly different between patients with isolated locoregional recurrence and those with distant recurrence (24.0 vs. 15.0 months; p = 0.587). There was no significant difference in median PRS time according to tumor location (20.0 months in E-IPNB vs. 10 months in I-IPNB; p = 0.323) and palliative treatment (16.0 months in palliative treatment vs. 14 months in no palliative treatment; p = 0.440).
Risk Factors for Time to Recurrence
In multivariable analysis, E-IPNB (hazard ratio [HR] = 3.041, 95% confidence interval [CI] 1.086–8.509; p = 0.034) and LN metastasis (HR = 3.818, 95% CI 1.322–11.025; p = 0.013) were independent prognostic factors for RFS (Table 3). Figure 2b, c presents the cumulative probability of recurrence over time for each independent risk factor.
Discussion
IPNB is a disease that can occur anywhere in the biliary tract, including in the intrahepatic and extrahepatic bile duct. The differentiation of structures around the bile duct by tumor location can affect the way the tumor spreads and recurs. Indeed, in the case of cholangiocarcinoma (CCC), intrahepatic CCC and extrahepatic CCC have been widely known to have different clinicopathological characteristics.23,24,25 However, there is no definition of IPNB according to location by WHO classification.23 Only a few studies have reported the recurrence patterns of IPNB by location. Of these, Choi et al.’s investigation concluded that there is no need for other treatment methods depending on location.7 Despite the lack of statistical significance due to the small sample size, it should be noted that invasive disease and LN involvement were more frequently observed in the extrahepatic duct in this study. In the current study, the location of the tumor was found to be an independent factor associated with recurrence of the tumor. To our knowledge, this is the first study to demonstrate differences in the prognosis of IPNB according to the location of the tumor. Although no significant difference was found, tumor multiplicity, MUC1, lymph node metastasis, and positive resection margins occurred more frequently in invasive E-IPNB than in invasive I-IPNB. In fact, all of the four factors just mentioned have been reported as poor prognostic factors in previous studies.3,6,12,15,26 Of course, further evidence should be accumulated, but it is expected to be clinically useful to consider different approaches to treatment and surveillance for IPNB according to tumor location, as in the case of CCC.
Among the 74 cases diagnosed as invasive IPNB, the 5-year recurrence rate of E-IPNB was 51.2% in the current study. Given this recurrence rate, which cannot be ignored, it is meaningful to seek a treatment to reduce the recurrence after surgery. However, it was difficult to verify the oncologic effect of adjuvant treatment because it was only performed on four E-IPNBs. Future studies that can demonstrate oncologic effects through adjuvant local treatment should be conducted.
Analysis of the recurrence pattern and timing is important in that it can infer the clinical characteristics of the primary tumor and effectively establish the follow-up strategy. Studies on the timing of recurrence can be particularly helpful in determining the optimal surveillance period and interval after curative resection. However, recurrence timing of IPNB has been analyzed by only one study, 5 and no established follow-up guideline exists for after surgery. In the NCCN guidelines for CCC, it is recommended that follow-up inspections be performed at 6-month intervals for at least 2 years after resection, regardless of the location of the cancer.27 The present study provides an analysis of the recurrence rate within 1 year and the timing of recurrence according to tumor location. The plateau of the RFS curve in overall IPNB was observed within 5 years and the rate of early recurrence was high. In fact, nearly half of the patients with recurrent IPNB experienced recurrence within 1 year. Among these, it was confirmed that I-IPNB was more closely related to early recurrence. With marginal significance, I-IPNB had a higher recurrence rate than E-IPNB within 1 year (83.3% vs. 33.3%; p = 0.061). It is interesting that invasion beyond ductal wall and macroscopically diffuse type IPNBs were found in four (80%) of the five patients with early recurrence in invasive I-IPNBs, respectively. Both of these factors are notable in that they are related to tumor invasiveness. In particular, it has been reported in a retrospective study that diffuse IPNB has a worse prognosis than other protruding types (5 years survival rates—20.8% vs.70.7%; p = 0.010).12 By contrary, all six cases with early recurrence within 1 year of invasive E-IPNB were protruding IPNB. Perhaps this may be related to differences in the way the tumor spreads due to the anatomical structure that depends on the location of the tumor. In the future, it will be necessary to verify statistically them through a large cohort study.
Of the five patients with early recurrence in invasive I-IPNBs, one developed at a month, one at 3 months, two at 7 months, and one developed at 12 months. This was detected through our surveillance process conducted every 3 months during the first year. Although studies using large samples should be further conducted, these findings may support the need for at least 1 year of close observation after resection of I-IPNB. By contrary, among the recurrent E-IPNB, the recurrence rate after 1 year was 66.7%. In addition, 50% of recurrent E-IPNB experienced recurrence during the follow-up period ranging from 1 to 3 years. Therefore, it is necessary to consider the mandatory surveillance for at least 3 years after resection of E-IPNB. Given the differences in recurrence timing according to tumor location, it is reasonable to apply different follow-up policies to E-IPNB and I-IPNB, respectively.
However, there has not yet been any study on whether palliative treatment can actually improve survival outcome after relapse. In the current study, small sample sizes failed to draw a solid conclusion about the effectiveness of palliative treatment compared with no treatment (median PRS time—16.0 months vs. 14 months; p = 0.440). Nonetheless, if the efficacy of palliative therapy is proven in subsequent studies, detection of recurrence may give an opportunity to provide palliative care at an appropriate time. Further studies should particularly demonstrate the oncologic benefits of local control for patients with isolated locoregional recurrence.
LN metastasis as well as tumor location were found to be independent prognostic factors for RFS in this study. From an oncologic point of view, lymph node involvement has traditionally been accepted as a clinical indicator to predict prognosis, because it indicates poorer biologic behavior as well as the potential for subsequent metastasis by cancer cells remaining in LNs.28 In two previous studies, LN involvement was revealed as an independent risk factor for survival29 and recurrence of malignant IPNB.15 This was also identified as an independent risk factor for recurrence in the present study. But, no one has identified the prognostic significance of lymph node dissection. In this regard, validating whether lymphadenectomy for IPNB can lead to oncologic benefits remains a challenge.
This study has some limitations. First, no established adjuvant treatment might have acted as bias for recurrence analysis. The chemotherapy regimen was determined by the oncologist’s preference. Second, small sample size of patients with recurrence makes it difficult to draw solid statistical conclusion about recurrence timing according to tumor location. This is related to the tendency to increase the model instability as the number of events per variable is smaller. Multicenter large cohort studies are needed to establish a more detailed and specific follow-up schedule according to tumor location of IPNB.
Conclusions
Tumor location proved to be an independent predictor of recurrence of IPNB. E-IPNB has a worse prognosis than I-IPNB. Of the recurrent E-IPNB, two-thirds have recurrence after 1 year. By contrary, I-IPNB has higher tendency of early recurrence within 1 year. Different surveillance policies according to tumor location are needed in patients undergoing surgery for IPNB.
References
Zen Y, Jang KT, Ahn S, Kim DH, Choi DW, Choi SH, Heo JS, Yeh MM. Intraductal papillary neoplasms and mucinous cystic neoplasms of the hepatobiliary system: demographic differences between Asian and Western populations, and comparison with pancreatic counterparts. Histopathology. 2014;65:164–173.
Minagawa N, Sato N, Mori Y, Tamura T, Higure A, Yamaguchi K. A comparison between intraductal papillary neoplasms of the biliary tract (BT-IPMNs) and intraductal papillary mucinous neoplasms of the pancreas (P-IPMNs) reveals distinct clinical manifestations and outcomes. Eur J Surg Oncol. 2013;39:554–558.
Rocha FG, Lee H, Katabi N, DeMatteo RP, Fong Y, D’Angelica MI, Allen PJ, Klimstra DS, Jarnagin WR. Intraductal papillary neoplasm of the bile duct: a biliary equivalent to intraductal papillary mucinous neoplasm of the pancreas? Hepatology. 2012;56:1352–1360.
Kubota K, Nakanuma Y, Kondo F, Hachiya H, Miyazaki M, Nagino M, Yamamoto M, Isayama H, Tabata M, Kinoshita H, Kamisawa T, Inui K. Clinicopathological features and prognosis of mucin-producing bile duct tumor and mucinous cystic tumor of the liver: a multi-institutional study by the Japan Biliary Association. J Hepatobiliary Pancreat Sci. 2014;21:176–185.
Kim KM, Lee JK, Shin JU, Lee KH, Lee KT, Sung JY, Jang KT, Heo JS, Choi SH, Choi DW, Lim JH. Clinicopathologic features of intraductal papillary neoplasm of the bile duct according to histologic subtype. Am J Gastroenterol. 2012;107:118–125.
Kloek JJ, van der Gaag NA, Erdogan D, Rauws EA, Busch OR, Gouma DJ, ten Kate FJ, van Gulik TM. A comparative study of intraductal papillary neoplasia of the biliary tract and pancreas. Hum Pathol. 2011;42:824–832.
Choi SC, Lee JK, Jung JH, Lee JS, Lee KH, Lee KT, Rhee JC, Jang KT, Choi SH, Heo JS, Choi DW, Lim JH. The clinicopathological features of biliary intraductal papillary neoplasms according to the location of tumors. J Gastroenterol Hepatol. 2010;25:725–730.
Tsuyuguchi T, Sakai Y, Sugiyama H, Miyakawa K, Ishihara T, Ohtsuka M, Miyazaki M, Yokosuka O. Endoscopic diagnosis of intraductal papillary mucinous neoplasm of the bile duct. J Hepatobiliary Pancreat Sci. 2010;17:230–235.
D’Souza M A, Isaksson B, Lohr M, Enochsson L, Swahn F, Lundell L, Arnelo U. The clinicopathological spectrum and management of intraductal papillary mucinous neoplasm of the bile duct (IPMN-B). Scand J Gastroenterol. 2013;48:473–479.
Mabrut JY, Boulez J, Peix JL, Gigot JF, Gouillat C, de La Roche E, Ducerf C, Baulieux J. Laparoscopic pancreatic resection: a preliminary experience of 15 patients. Hepatogastroenterology. 2005;52:230–232.
Horm TM, Schroeder JA. MUC1 and metastatic cancer: expression, function and therapeutic targeting. Cell Adh Migr. 2013;7:187–198.
Kang MJ, Jang JY, Lee KB, Han IW, Kim SW. Impact of macroscopic morphology, multifocality, and mucin secretion on survival outcome of intraductal papillary neoplasm of the bile duct. J Gastrointest Surg. 2013;17:931–938.
Yang J, Wang W, Yan L. The clinicopathological features of intraductal papillary neoplasms of the bile duct in a Chinese population. Dig Liver Dis. 2012;44:251–256.
Li T, Ji Y, Zhi XT, Wang L, Yang XR, Shi GM, Zhang W, Tang ZY. A comparison of hepatic mucinous cystic neoplasms with biliary intraductal papillary neoplasms. Clin Gastroenterol Hepatol. 2009;7:586–593.
Jung G, Park KM, Lee SS, Yu E, Hong SM, Kim J. Long-term clinical outcome of the surgically resected intraductal papillary neoplasm of the bile duct. J Hepatol. 2012;57:787–793.
Ebata T, Kosuge T, Hirano S, Unno M, Yamamoto M, Miyazaki M, Kokudo N, Miyagawa S, Takada T, Nagino M. Proposal to modify the International Union Against Cancer staging system for perihilar cholangiocarcinomas. Br J Surg. 2014;101:79–88.
Zen Y, Pedica F, Patcha VR, Capelli P, Zamboni G, Casaril A, Quaglia A, Nakanuma Y, Heaton N, Portmann B. Mucinous cystic neoplasms of the liver: a clinicopathological study and comparison with intraductal papillary neoplasms of the bile duct. Mod Pathol. 2011;24:1079–1089.
Jang GW, Hwang S, Lee YJ, Kim KH, Park KM, Ahn CS, Moon DB, Ha TY, Song GW, Jung DH, Park GC, Lee SG. Clinicopathological features of the intraductal papillary neoplasms of the intrahepatic bile duct. Korean J Hepatobiliary Pancreat Surg. 2012;16:138–141.
Naito Y, Kusano H, Nakashima O, Sadashima E, Hattori S, Taira T, Kawahara A, Okabe Y, Shimamatsu K, Taguchi J, Momosaki S, Irie K, Yamaguchi R, Yokomizo H, Nagamine M, Fukuda S, Sugiyama S, Nishida N, Higaki K, Yoshitomi M, Yasunaga M, Okuda K, Kinoshita H, Nakayama M, Yasumoto M, Akiba J, Kage M, Yano H. Intraductal neoplasm of the intrahepatic bile duct: clinicopathological study of 24 cases. World J Gastroenterol. 2012;18:3673–3680.
Katabi N, Torres J, Klimstra DS. Intraductal tubular neoplasms of the bile ducts. Am J Surg Pathol. 2012;36:1647–1655.
Nakanuma Y, Sato Y, Ojima H, Kanai Y, Aishima S, Yamamoto M, Ariizumi S, Furukawa T, Hayashi H, Unno M, Ohta T, Hepatolithiasis Subdivision of Intractable Hepatobiliary Diseases Study Group of J. Clinicopathological characterization of so-called “cholangiocarcinoma with intraductal papillary growth” with respect to “intraductal papillary neoplasm of bile duct (IPNB)”. Int J Clin Exp Pathol. 2014;7:3112–3122.
Ohtsuka M, Shimizu H, Kato A, Yoshitomi H, Furukawa K, Tsuyuguchi T, Sakai Y, Yokosuka O, Miyazaki M. Intraductal papillary neoplasms of the bile duct. Int J Hepatol. 2014;2014:459091.
FT B, F C, RH H, ND T. WHO Classification of Tumours of the Digestive System. Lyon: IARC 2010.
Rizvi S, Gores GJ. Pathogenesis, diagnosis, and management of cholangiocarcinoma. Gastroenterology. 2013;145:1215–1229.
Nakeeb A, Pitt HA, Sohn TA, Coleman J, Abrams RA, Piantadosi S, Hruban RH, Lillemoe KD, Yeo CJ, Cameron JL. Cholangiocarcinoma. A spectrum of intrahepatic, perihilar, and distal tumors. Ann Surg. 1996;224:463–473; discussion 473-465.
Gordon-Weeks AN, Jones K, Harriss E, Smith A, Silva M. Systematic Review and Meta-analysis of Current Experience in Treating IPNB: Clinical and Pathological Correlates. Ann Surg. 2016;263:656–663.
National Comprehensive Cancer Network. Hepatobiliary Cancers (Version 2.2019). https://www.nccn.org/professionals/physician_gls/pdf/hepatobiliary.pdf. Accessed March 7, 2019.
Kawada K, Taketo MM. Significance and mechanism of lymph node metastasis in cancer progression. Cancer Res. 2011;71:1214–1218.
Luvira V, Pugkhem A, Bhudhisawasdi V, Pairojkul C, Sathitkarnmanee E, Luvira V, Kamsa-Ard S. Long-term outcome of surgical resection for intraductal papillary neoplasm of the bile duct. J Gastroenterol Hepatol. 2017;32:527–533.
Author information
Authors and Affiliations
Contributions
Conception/design (Seong Ho Choi, Dong Wook Choi, Yunghun You); data acquisition (Seong Ho Choi, Dong Wook Choi, Jin Seok Heo, Kee-Taek Jang); data interpretation (Seong Ho Choi, Yunghun You, Dong Wook Choi, Jin Seok Heo, In Woong Han, Kee-Taek Jang, Sunjong Han); drafting (Yunghun You); critical revisions (Seong Ho Choi, Kee-Taek Jang); final approval (all authors).
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
You, Y., Choi, S.H., Choi, D.W. et al. Recurrence After Resection for Intraductal Papillary Neoplasm of Bile Duct (IPNB) According to Tumor Location. J Gastrointest Surg 24, 804–812 (2020). https://doi.org/10.1007/s11605-019-04235-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04235-8