Abstract
Metastatic solid pseudopapillary neoplasms of the pancreas are rare, and the stomach is also a rare site for metastases. We present a case of a lady with solid pseudopapillary neoplasm of the pancreas who previously had a distal pancreatectomy but subsequently had multiple hepatic, adrenal peritoneal and nodal metastases. She developed dyspepsia and on oesophagogastroduodenoscopy, was found to have gastric metastases as well. We believe this is the first reported case of metastatic solid pseudopapillary neoplasm of the pancreas to the stomach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Clinical Case
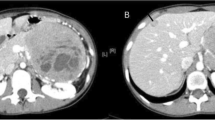
A 73-year-old Chinese lady with a previous history of solid pseudopapillary neoplasm (SPN) of the pancreas post distal pancreatectomy, splenectomy and wedge resection of the stomach 4 years ago presented to our clinic on follow-up with a surveillance CT scan showing several hepatic, a left adrenal and peritoneal metastases with prominent gastrohepatic and periportal lymph nodes. No masses were reported in the stomach. Core biopsies of the liver lesion revealed metastatic SPN of the pancreas.
The patient, who had previously been asymptomatic, now complained of poor appetite and dyspepsia. Abdominal examination was unremarkable with no palpable masses.
An oesophagogastroduodenoscopy (OGD) visualized tumour along the cardia, greater curve, and lesser curve of the stomach away from gastro-oesophagal junction (Fig. 1). Biopsies of this lesion too confirmed metastatic SPN of the pancreas.
In view of the natural history of slow growth of SPN of the pancreas and a lack of known chemotherapy, no treatment has been planned for this patient at this stage. She will require radiotherapy if a malignant bleed develops from the gastric lesions or for transcatheter arterial chemoembolization (TACE), radiotherapy or steroid treatment if the liver metastases become symptomatic.
Discussion
SPN of the pancreas is a rare entity.1 It constitutes about 5% of cystic pancreatic tumors and about 1 to 2% of exocrine pancreatic neoplasms.2 It is almost exclusively seen in females and usually occurs in the second or third decades of life.1,2 SPN of the pancreas can occur in every part of the pancreas but is slightly more common in the tail.2,3 A high index of clinical suspicion is necessary to suspect and diagnose SPN of the pancreas.1
SPN is considered to be a low-grade malignant tumour.1 In approximately 85% of the patients, SPN is limited to the pancreas, while about 10 to 15% of tumours have already metastasized at the time of presentation.2 Most authors agree that aggressive surgical resection is the best treatment for achieving curative results and a better long-term survival.1
A local recurrence rate of 6.2% is reported in cases treated by radical surgical excision and hepatic or Krukenberg-type distant metastases develop in 5.6% of cases.1 The most common sites for metastasis are the liver, portal, splenic, or superior mesenteric vein, regional lymph nodes, mesentery, omentum and peritoneum.2,3,4
The stomach, as reported in our patient, is a rare site of metastasis of SPN or for any other cancer. A PubMed search did not bring up any reported cases of SPN of the pancreas with gastric metastases. We believe that this may be the first reported case of SPN with gastric metastases.
Thus, in a patient with a known history of SPN, recurrence or metastatic disease should be excluded in the setting of symptoms such as epigastric pain, dyspepsia, gastrointestinal bleeding or gastric outlet obstruction. The prognosis of patients with gastric metastases of pancreatic SPN is unknown. There is no ideal treatment for symptomatic gastric metastases but radiotherapy is possible. Rarely is surgery an option especially when there are likely to be other metastases as well.
Treatment protocols do not exist for various types of metastatic disease of SPN, owing to the paucity of available literature. Current literature recommends complete surgical excision and debulking with even metastatectomy if required.4 These authors conclude that long-term survival improves with complete surgical resection of primary with metastectomy for synchronous or metachronous lesions.1
Conversely, the prognosis is favourable even in the presence of distant metastasis, and some patients with unresectable SPN or asymptomatic disseminated disease may also have a long-term survival ranging from years to decades.2,4 This possibly can be attributed to a low Ki-67 index (≤ 5%), indicating a slow growth of the tumor.3
As such, metastatic SPN presents clinicians with very real therapeutic dilemmas.
Close long-term follow-up appears to be required, in order to diagnose a local recurrence or distant metastasis and to facilitate choosing the proper therapeutic option for the patient.2 Further studies looking at both the long-term survival data of patients with metastatic SPN, as well as clinical and pathological prognosticating factors, are warranted.
References
Patil TB, Shrikhande SV, Kanhere HA, Saoji RR, Ramadwar MR, Shukla PJ.Solid pseudopapillary neoplasm of the pancreas: a single institution experience of 14 cases. HPB. 2006;8:148–150.
Ayse Y, Savas Y, Ali C, Erkan N, Yildirim M, Talcin E, Postaci H. Diagnosis and treatment of solid pseudopapillary tumor of the pancreas: experience of one single institution from Turkey. World J Surg Oncol. 2013;11:308
Vassos N, Abbas A, Klein P, Hohenberger W, Croner RS. Solid-pseudopapillary neoplasm (SPN) of the pancreas: case series and literature review on an enigmatic entity. Int J Clin Exp Pathol. 2013;6:1051–1059.
Lee HS, Kim HK, Shin BK, Choi JH, Choi YJ, Kim HY. A rare case of recurrent metastatic solid pseudopapillary neoplasm of the pancreas. J Pathol Tansl Med. 2017;51:87–91
Author information
Authors and Affiliations
Contributions
Prajwala S Prakash wrote and edited the manuscript, compiled the data, assisted in formulating the write up and looked after the patient. Dexter Yak Seng Chan wrote part of manuscript, formulated the write up, edited the manuscript, looked after the patient and is the corresponding author. Krishnakumar Madhavan is the main doctor looking after patient, edited the manuscript, followed up on the patient and formulated the write up. All the authors have read and approved of the content to be submitted for publication. Each author has contributed in the ways as listed above and met the four criteria as required for authorship.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Prakash, P.S., Chan, D.Y.S. & Madhavan, K. The Stomach: a Rare Site for Metastatic Solid Pseudopapillary Neoplasm of the Pancreas. J Gastrointest Surg 22, 759–760 (2018). https://doi.org/10.1007/s11605-017-3599-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-017-3599-3