Abstract
35-year-old man with new onset abdominal pain. A mass in the tail of the pancreas was found on imaging.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Clinical History
35-year-old man with new onset abdominal pain. A mass in the tail of the pancreas was found on imaging.
Imaging Findings
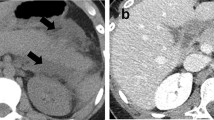
Axial contrast-enhanced venous phase CT demonstrates a 4 cm lobulated, hypodense cystic mass in the tail of the pancreas with mild enhancement of peripheral soft tissue component and septations (Fig. 1a, arrow). Coronal arterial phase CT shows compression and narrowing of the splenic vein by the mass without invasion (Fig. 1b, arrow).

Fig. 1
Differential Diagnosis
Solid-pseudopapillary (SPN) neoplasm, mucinous cystic neoplasm, intraductal papillary mucinous neoplasm (IPMN), pancreatic neuroendocrine tumor (PanNET), and pancreatic ductal adenocarcinoma.
Diagnosis
Solid-pseudopapillary neoplasm.
Discussion
Solid-pseudopapillary neoplasm (SPN) is a rare pancreatic neoplasm, accounting for less than 3% of all exocrine pancreatic tumors [1, 2]. These tumors usually affect young women but can also be seen in men. In a review of 553 patients with SPN, 59 (10%) were male patients [3].
On imaging studies, most SPNs are well-encapsulated, round, or oval complex masses with both solid and cystic components (Fig. 1) [2]. CT attenuation numbers in the cystic regions vary from fluid attenuation equal to that of water, to soft tissue attenuation in areas rich in blood [1]. Calcifications may be present within the capsule, a feature also found in mucinous cystic neoplasms (Fig. 3a and b). On MRI, SPNs are typically homogeneously or heterogeneously hypointense on T1-weighted images. Occasionally, areas of hyperintensity may be seen on T1-weighted images secondary to internal hemorrhage [2, 4] (Fig. 3c). On T2-weighted images, they are typically heterogeneously hyperintense [4] (Fig. 3e). After administration of contrast material, mild contrast enhancement is seen in the solid areas on CT or MRI, typically in the periphery of the tumors [2, 4] (Fig. 3d). This finding is helpful to distinguish SPN from neuroendocrine tumors which typically show an early intense contrast enhancement [4]. SPNs are usually not associated with the pancreatic ductal dilatation or vascular encasement [2, 4].
Patient illustrated in Fig. 1 underwent distal pancreatectomy. The surgical resection specimen showed an irregularly shaped, heterogeneous tumor with gray, yellow, and hemorrhagic regions; cystic degeneration was noted. A touch preparation made at the time of sectioning demonstrated the characteristic branching, delicate vasculature (pseudopapillae) lined by uniform loosely cohesive oval cells
Companion case. 49-year-old woman with incidentally found SPN in the tail of the pancreas. Axial contrast-enhanced venous phase CT shows predominantly cystic mass with minimal enhancement of peripheral solid components (a, thick arrows). Scattered rim calcifications (a, thin arrows) are also seen on axial images and the volume-rendered images (b, arrows). Axial T1-weighted image before (c) and after (d) contrast administration shows predominantly cystic mass with enhancing peripheral solid components (d, arrow). On axial T2-weighted image, the mass is in heterogeneous areas of high signal intensity representing the cystic component (e, arrow). Note peripheral calcifications better appreciated on CT
SPN is a low-grade malignant neoplasm. It is often cured after complete surgical resection [5]. However, metastasis may develop in 10–15% of patients [3, 6]. Common sites of metastasis include the liver, regional lymph nodes, mesentery, omentum, and peritoneum [3, 5, 6]. Local invasion to the duodenum, stomach, spleen, or major blood vessels may also occur [3, 6].
Teaching Point
SPN should be considered in young women with a complex, solid, or cystic mass in the pancreas.
References
Kawamoto S, Scudiere J, Hruban RH, Wolfgang CL, Cameron JL, Fishman EK. Solid-pseudopapillary neoplasm of the pancreas: spectrum of findings on multidetector CT. Clin Imaging. 2011;35(1):21–8. doi:10.1016/j.clinimag.2009.11.007.
Raman SP, Kawamoto S, Law JK, Blackford A, Lennon AM, Wolfgang CL, et al. Institutional experience with solid pseudopapillary neoplasms: focus on computed tomography, magnetic resonance imaging, conventional ultrasound, endoscopic ultrasound, and predictors of aggressive histology. J Comput Assist Tomogr. 2013;37(5):824–33. doi:10.1097/RCT.0b013e31829d44fa.
Yu PF, Hu ZH, Wang XB, Guo JM, Cheng XD, Zhang YL, et al. Solid pseudopapillary tumor of the pancreas: a review of 553 cases in Chinese literature. World J Gastroenterol. 2010;16(10):1209–14.
Ventriglia A, Manfredi R, Mehrabi S, Boninsegna E, Negrelli R, Pedrinolla B, et al. MRI features of solid pseudopapillary neoplasm of the pancreas. Abdom Imaging. 2014;39(6):1213–20. doi:10.1007/s00261-014-0169-y.
Reddy S, Cameron JL, Scudiere J, Hruban RH, Fishman EK, Ahuja N, et al. Surgical management of solid-pseudopapillary neoplasms of the pancreas (Franz or Hamoudi tumors): a large single-institutional series. J Am Coll Surg. 2009;208(5):950–7; discussion 7–9. doi:10.1016/j.jamcollsurg.2009.01.044.
Mao C, Guvendi M, Domenico DR, Kim K, Thomford NR, Howard JM. Papillary cystic and solid tumors of the pancreas: a pancreatic embryonic tumor? Studies of three cases and cumulative review of the world’s literature. Surgery. 1995;118(5):821–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Kawamoto, S. (2017). Case 45: Solid-Pseudopapillary Neoplasm. In: Zaheer, A., Fishman, E., Pittman, M., Hruban, R. (eds) Pancreatic Imaging. Springer, Cham. https://doi.org/10.1007/978-3-319-52680-5_45
Download citation
DOI: https://doi.org/10.1007/978-3-319-52680-5_45
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-52678-2
Online ISBN: 978-3-319-52680-5
eBook Packages: MedicineMedicine (R0)