Abstract
Background and Aims
Gastrointestinal stromal tumors (GISTs) have significant variability in size and malignant behavior. Our current understanding is limited to pathological analyses, autopsy studies, and small case series. The aim of the current study is to define the risk factors, incidence, and mortality rates of GIST <2 cm in the National Cancer Institute’s Surveillance, Epidemiology, and End Results database.
Methods
Patients with histologically confirmed malignant GIST <2 cm were studied from 2001 to 2011. GIST was defined by GI tumor site codes and GIST-specific histology codes.
Results
We identified 378 patients with GIST <2 cm. The average age at diagnosis was 64.0 years with equal sex distribution. The most common tumor location was the stomach (62.2 %), followed by the small intestine (23.3 %), colon (5.6 %), and rectum (3.4 %). Most patients had localized disease (79.4 %), but 11.4 % had regional/distant metastatic disease. The annual incidence rate was 4.2 per 10,000,000 (10M). This was the highest among Blacks (7.6 per 10M). Among patients with GIST and no additional cancers, the 5-year GIST-specific mortality was 12.9 %. Moreover, there was a significantly increased 5-year GIST-specific mortality in those patients who had regionally advanced (34.0 %) or metastatic GIST (34.3 %), as compared to those patients with localized GIST (5.6 %).
Conclusions
This study represents the first population-based analysis of malignant GIST <2 cm. While quite rare, these tumors have an underappreciated disease-specific mortality. Further studies are needed to define the underlying reasons for the identified racial differences, to develop novel risk assessment schema for patients with these small tumors, and to determine appropriate indications for resection and/or medical therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastrointestinal stromal tumor (GIST) represents the most common sarcoma of the gastrointestinal (GI) tract. These tumors are thought to arise from the pacemaker cells of the gut known as the interstitial cells of Cajal (ICC).1 – 3 In 1998, Hirota and colleagues reported that GIST was initiated by gain-of-function mutations in KIT (c-KIT, CD117) with associated KIT-positive immunostaining.1 This provided an objective measure to diagnose GIST and led to the implementation of a GIST-specific histology code in 2001. This improved the validity and precision of GIST coding and reporting. Recently, our group defined the epidemiology of GIST of all sizes in the USA through analysis of the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) database using this histological code.4 The annual age-adjusted incidence averaged 6.8 per 1,000,000, and GIST was more common in males, non-Hispanics, Blacks, and Asians/Pacific Islanders.4
Despite our epidemiological analysis, it is increasingly evident that GIST is not one homogeneous malignancy; there is significant variability in terms of size and malignant behavior. The disease spectrum ranges from “small GIST” to massive intra-abdominal tumors. GISTs less than 2 cm have been referred to by a multitude of names, including ICC hyperplasia, minute GIST, GIST tumorlets, micro-GIST, and small GIST.5 , 6 Given their small size, patients are often asymptomatic and tumors are typically discovered incidentally during endoscopic procedures by gastroenterologists or during cross-sectional radiologic studies.7 – 10 It has been reported that up to 30 % of people have small GIST.11 – 14 However, this data comes from autopsy studies and retrospective pathological series, making it limited by several biases.11 – 15 Other studies have examined the biology of these tumors and demonstrated that GISTs <2 cm have a lower frequency of KIT mutations than larger GIST, and they tend to exhibit lower mitotic rates.12 , 13 , 15 Because our current understanding is limited to pathological analyses, autopsy studies, and case series with small sample sizes, we lack a clear understanding of the clinical significance of small GIST. In fact, the National Comprehensive Cancer Network (NCCN) and the European Society of Medical Oncology (ESMO) guidelines for the surveillance and management of GIST <2 cm have been deemed controversial or lack evidence-based approaches.8 Furthermore, little is known about the epidemiology, risk factors, and natural history of these smaller tumors.4 , 16 Therefore, the aim of the current study is to define the risk factors, incidence, and mortality rate of GIST <2 cm in the National Cancer Institute’s SEER database.
Materials and Methods
Using the SEER database,17 we identified patients with histologically confirmed GIST <2 cm diagnosed between 2001 and 2011. The SEER database consists of 18 regional cancer registries across the USA, which covers approximately 28 % of the US population. GIST was defined by GI tumor site codes (C150–C189, C199, C209–C212, C218, C220–C221, C239–C260, C268–C269, C480–C482, C488) and the GIST-specific histology code (ICD-O-3 code 8936); only patients with tissue sampled by biopsy or surgical resection were eligible for inclusion in this study. GIST <1 cm and GIST 1–1.99 cm were defined by EOD-10 tumor size codes for 2001–2003 and CS tumor size codes for 2004–2011. Follow-up extended through December 2011. Age-adjusted incidence rates per 10,000,000 (10M) subjects were based on 5-year age categories defined with the 2000 US standard population used as the denominator.18 The Tiwari method was used to calculate 95 % confidence intervals (CI) for incidence rates.19 Cancer-specific survival was determined using cumulative incidence analysis, with death from noncancer causes as a competing risk. Overall survival was determined using Kaplan-Meier analysis and comparisons were made using the log-rank test. In these analyses, patients were censored at death or date of last known follow-up. A multivariable Cox regression analysis was used to adjust for potential confounders when exploring the impact of the presence of additional cancers on survival. This included age as a continuous variable, as well as sex, race, and stage. Associations were considered statistically significant if the 95 % CI excluded the null value. Incidence rates were calculated with SEER-Stat (version 8.1.5, Calverton, MD), and multivariable analyses were conducted with SAS (version 9.4, Cary, NC) using Cox proportional hazard regression. Kaplan-Meier and cumulative incidence analyses were performed in R version 3.2.2. The Institutional Review Board of University of California, San Diego, deems studies of this nature exempt from review.
Results
Demographics
We identified 378 patients diagnosed with malignant GIST <2 cm between 2001 and 2011 within the SEER database. Table 1 shows the incidence rates for GIST <2 cm stratified by demographic and GIST-specific factors. The annual incidence rate was 4.2 per 10,000,000 (10M) (95 % CI 3.8–4.6). The average age (± standard deviation) at diagnosis was 64.0 ± 12.8 years. The distribution was nearly equal between the sexes (male 48.9 %; female 51.1 %). However, the incidence was highest among Blacks (7.6 per 10M, 95 % CI 5.8–9.7) and Asians/Pacific Islanders (4.6 per 10M, 95 % CI 3.2–6.3) as compared to Caucasians (3.7 per 10M, 95 % CI 3.3–4.2). The stomach was the most common tumor site (62.2 %) followed by the small intestine (23.3 %), colon (5.6 %), and rectum (3.4 %). Overall, 79.4 % of patients presented with localized disease, while 11.4 % had regional or distant metastatic disease. The remaining 9.2 % of patients had missing or unknown stage data. The majority of patients underwent surgical excision as part of their first course of treatment (322/375, 85.9 %). Of the remaining patients, 1 patient declined an operation (1/375, 0.27 %) while 52 patients only had biopsies, but no operation was recommended (52/375, 13.9 %). Three patients were excluded due to missing data.
Demographics of the GIST Subsets
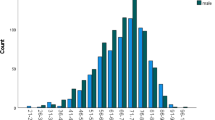
On subset analyses, we identified 138 patients with GIST <1 cm and 240 patients with GIST 1–1.99 cm. Supplemental Table 1 shows the incidence rates for the groups stratified by demographic and GIST-specific factors. For GIST <1 cm, the annual incidence rate was 1.5 per 10M (95 % CI 1.2–1.8), while for GIST 1–1.99 cm, the annual incidence rate was 2.7 per 10M (95 % CI 2.3–3.0). The average age (± standard deviation) at presentation was 62.3 ± 12.2 and 65.0 ± 13.0 years for GIST <1 cm and GIST 1–1.99 cm, respectively. Supplemental Fig. 1 shows the age-adjusted incidence of GIST <1 cm and GIST 1–1.99 cm stratified by age. The annual incidence increased with age for both subsets, from 0 per 10M (95 % CI 0–0.1) for those under age 20 years old in both subsets to 3.4 per 10M (95 % CI 1.6–6.2; GIST <1 cm) and 10.8 per 10M (95 % CI 7.4–15.2; GIST 1–1.99 cm) for those above 80 years old. The peak age range for GIST <1 cm was 60–69 years old with an incidence of 7.5 per 10M (95 % CI 5.6–9.8). The peak age range for GIST 1–1.99 cm was 70–79 years old with an incidence of 14.7 per 10M (95 % CI 11.4–18.6). The distribution was nearly equal between the sexes in the GIST <1-cm group (male 48.6 %; female 51.4 %) and the GIST 1–1.99-cm group (male 50.8 %; female 49.2 %). The incidence was also highest among Blacks with 2.5 per 10M (95 % CI 1.6–3.8; GIST <1 cm) and 5.1 per 10M (95 % CI 3.6–6.9; GIST 1–1.99 cm). Similar to GIST of all sizes, the stomach was the most common site of disease in both groups (64.5 and 60.8 %, respectively). Finally, most patients presented with localized disease in the two groups (81.9 and 77.9 %, respectively).
Analyses of Demographic Risk Factors
We next looked for risk factors for developing GIST among the entire cohort of GIST <2 cm and the two GIST subsets, namely GIST <1 cm and GIST 1–1.99 cm (Supplemental Table 2). As compared to Whites (reference group) in the entire cohort and the two GIST subsets, Blacks were 2.1, 1.8, and 2.2 times more likely to develop GIST, respectively. No other racial group was at higher or lower risk as compared to Whites. Moreover, the sex distribution was essentially equal in all groups. Finally, in distinction from the entire cohort and GIST <1-cm subset, GIST 1–1.99 cm was 1.8 times more likely to occur in non-Hispanics compared to Hispanics.
Overall and Cancer-Specific Mortality Analyses
We performed mortality analyses on a subset of our cohort that had no missing data (N = 375). The 5-year overall mortality was 30.9 % for all patients with GIST <2 cm. There was no significant difference in 5-year mortality between those with tumors <1 cm (23.3 %) and those with tumors 1–1.99 cm (33.8 %) (P = 0.322) (Fig. 1a). Given these high mortality rates and our recent publication describing higher incidences of additional cancers in GIST patients, we queried whether the presence of additional cancers may explain this unexpected finding.20 Kaplan-Meier analysis, stratified by the presence of additional cancers, demonstrated a significant difference in overall mortality between these groups, with a 5-year mortality of 20.0 % in those with GIST only and 33.8 % in those with GIST and additional cancers (P = 0.001) (Fig. 1b). On multivariable analysis, after adjusting for age, race, sex, and stage, we found that the presence of additional cancers was associated with increased risk of death (HR 1.82, 95 % CI 1.14, 2.90, P = 0.012) (Supplemental Table 3). Black race and advanced stage (i.e., regional and distant disease) were also associated with increase risk of death in this analysis (Supplemental Table 3). Subset Kaplan-Meier analysis of patients with known stage data (N = 340) demonstrated a mortality increase in those patients who had distant disease, as compared with localized or regional disease [5-year mortality—51.3, 26.6, and 26.5 %, respectively (P = 0.004)] (Fig. 1c). Similar analysis demonstrated significantly increased overall mortality among patients who did not undergo surgical excision of their GIST compared to those who did, with 5-year overall mortality of 54.5 and 27.15 %, respectively (P < 0.001) (Fig. 1d).
We then performed cumulative incidence analyses investigating cancer-specific mortality, taking death from any other causes into account as a competing risk. There was no significant difference in cancer-specific mortality between those with GIST <1 cm or those with tumors 1–1.99 cm (P = 0.57) (Fig. 2a). However, there was a significantly increased risk of death from cancer among patients who had additional cancers (5-year cancer-specific mortality 28.9 %) as compared to those who only had GIST (5-year cancer-specific mortality 12.9 %) (P = 0.005) (Fig. 2b). Analyses of patients with known GIST stage data (N = 340) demonstrated that the all-cause cancer-specific mortality increases in those patients who had metastatic GIST, as compared with localized GIST or regionally advanced GIST [5-year cancer-specific mortality—36.5, 15.2, and 31.4 %, respectively (P = 0.001)] (Fig. 2c). Similar analysis demonstrated significantly increased cancer-specific mortality among patients who did not undergo surgical excision of their GIST compared to those who did, with 5-year cancer-specific mortality of 39.8 and 17.5 %, respectively (P = 0.007) (Fig. 2d).
Finally, among GIST-only patients with tumors <2 cm and known stage (N = 204), there was a significantly increased 5-year GIST-specific mortality in patients who had regionally advanced GIST (34.0 %) or metastatic GIST (34.3 %), as compared to those patients with localized GIST (5.6 %) (P < 0.001) (Fig. 3a). Among patients who presented with regional disease, the stomach was the most common primary tumor site (7/15, 46.7 %), followed by the small intestine (6/15, 40.0 %) and colon or rectum (2/15, 13.3 %). Similarly, among patients who presented with distant disease, the stomach was again the most common primary tumor site (8/13, 61.5 %), followed by the small intestine (5/13, 38.5 %). Additional demographic and clinical characteristics of these patients are included in Supplemental Table 4. Analysis of GIST-only patients demonstrated no significant difference in GIST-specific mortality between patients who underwent surgical resection and those who did not (5-year GIST-specific mortality of 10.9 and 27.9 %, respectively, P = 0.13) (Fig. 3b).
Discussion
Building upon our group’s previous report on the epidemiology of GIST, this study represents the first population-based assessment that specifically focuses upon malignant GIST <2 cm. It demonstrates that patients with these tumors have demographic differences from patients with GIST of any size and these tumors occur most frequently in Blacks and can arise throughout the gastrointestinal tract. Moreover, while quite rare, these malignant tumors can lead to death for 1 in 7.8 patients at 5 years. Taken together, we provide a description and statistical examination of GIST <2 cm in the current era of immunohistochemical diagnoses of malignant GIST.
Until now, the epidemiology of GIST <2 cm was poorly understood, because prior studies were limited to pathological analyses, autopsy studies, and case series with small sample sizes.11 – 15 These studies commonly focused upon one region of the GI tract and thus provided an incomplete description of the true incidence and distribution of GIST <2 cm. Agaimy et al. estimated that 20–30 % of older adults have GIST <2 cm based upon autopsy cases and surgical pathology analyses.12 However, this study was limited by several biases, namely (1) it only included gastric GIST cases, (2) it was derived from a single institution, and (3) it analyzed two subsets of patients known to be at higher risk for GIST (i.e., older patients4 and patients undergoing surgery for other diseases or tumors20). Additionally, Chan et al. studied the prevalence of concurrent small GIST in 207 patients undergoing esophagectomy or gastrectomy. They found that 87 % of the 15 small GISTs discovered were located in the stomach.14 Again, this study only assessed the upper GI tract and was limited to patients undergoing surgery for other diseases or tumors. We now report that the average annual incidence of malignant GIST <2 cm in the USA is 4.2 per 10M. GIST <1 cm and GIST 1–1.99 cm represent 2.2 and 4.0 % of all GIST diagnoses, which have an overall incidence of 68 per 10M (i.e., 0.68 per 100,000). Thus, our population-based findings provide a more complete understanding of the current incidence of malignant GIST <2 cm throughout the GI tract.
The 5-year overall mortality rate for GIST <2 cm was 30.9 %, which is comparable to the mortality rate of 35 % for GIST of all sizes.4 Given this high mortality rate and our previous findings demonstrating a higher incidence of additional cancers among patients with GIST,20 we excluded patients with additional cancer diagnoses from our analyses. This revealed that the 5-year GIST-specific mortality rate was 12.9 %. Patients who underwent resection of their small GIST appeared to have increased overall and cancer-specific survival, although in a subset analysis of GIST-only patients, this trend failed to meet significance criteria. This finding must be interpreted with caution, however, given our inability to control for confounders such as frailty or comorbid conditions that may have precluded the patient from undergoing an operation and increased their risk of death. Consistent with the underappreciated aggressive biology noted, 11 % of patients with GIST <2 cm had regional or distant metastases. While previous data indicates that primary GIST of the colon and/or rectum put patients at higher risk of aggressive disease,21 our findings show that primary tumors of the stomach or small intestine are associated with the development of regional or metastatic disease. While our study is limited by small numbers of patients with regional or distant disease, this information regarding primary site should not be overlooked.
It is important to understand this mortality rate in the context of the tumors studied; this study does not include undiagnosed or asymptomatic tumors. Therefore, the described rates are specific to small GISTs that are coded as malignant and have been histologically evaluated following biopsy or resection. Thus, our findings likely overestimate the GIST-specific mortality of all small GISTs. However, clearly, a subset of small GIST with regionally advanced and/or metastatic disease has an aggressive phenotype with 1 in 2.9 patients dying of the disease at 5 years. Furthermore, 1 in 17.9 with small, localized GIST will also die of the disease at 5 years. The latter finding remains quite concerning as current NCCN guidelines provide a category 2B recommendation (i.e., nonuniform NCCN consensus) for the management of GIST <2 cm, and these are deemed controversial due to limited data on the subject. These current recommendations include surgical removal of symptomatic tumors versus close surveillance of low-risk tumors. However, given the high GIST-specific mortality rate that we identified in this population-based analysis, further studies are warranted to understand the natural history and malignant potential of these small GISTs.
We also compared patient demographics in this study population to those of all GIST patients. We found that GISTs <2 cm are equally distributed between the sexes, which differs from our analysis of patients with GIST of any size, in which GISTs were more common in males.4 Therefore, an unacknowledged biologic relationship may exist between GIST size and sex. Consistent with this hypothesis, Call et al. found that among pediatric GIST cases, patients were predominately female.22 While our study included no pediatric cases of GIST, it is possible that GISTs <2 cm share more characteristics with pediatric GIST as opposed to adult GIST, thus shifting the sex distribution. In terms of racial differences, malignant GISTs <2 cm were more common in Blacks as compared to Whites, consistent with our earlier finding in all patients with GIST.4 However, while GISTs of all sizes were more common in Asians/Pacific Islanders than Whites, this was not the case for GIST <2 cm. The highest incidence of GIST <2 cm was consistent with GIST of all sizes, peaking among patients aged 70 to 79 years of age. Similar to GIST of all sizes, GISTs <2 cm are most commonly found in the stomach (62 %) and the small intestine (23 %). Taken together, GISTs <2 cm occur in a similar patient population as compared to those patients with larger tumors, with differences in sex and race distributions.
Our study is limited to describing the epidemiology of malignant GIST <2 cm in the SEER database. As a result, we likely underestimated the true underlying incidence since there are many patients with asymptomatic GIST <2 cm that were not identified, lacked a tissue diagnosis, or were coded as “benign.” Consistent with the latter hypothesis, Choi et al. demonstrated that there is underreporting of GIST at the national registry level, because hospital-based cancer registrars and coders may code them as benign.23 This further confounds the underestimation of these tumors as the SEER database is missing these pathologically defined GISTs. Our study also carries a component of selection bias since we only assess patients with a tissue diagnosis of a frequently asymptomatic tumor; thus, patients who are undergoing surveillance of unresected tumors are not included. Despite these limitations, our study provides a better understanding of GIST <2 cm as we are able to assess a large number of patients across multiple ages and states, with GIST distributed throughout the GI tract. Since these tumors were identified using histology and site-specific codes, misdiagnosis and miscoding are still potential sources of error; however, these coding errors are likely equally distributed across all patients and thus should not greatly influence the distribution of tumors. Also, the current ICD-O-3 GIST histology code was instated in 2001. While we only included patients diagnosed after 2001, we may still be underestimating patients with GIST <2 cm in SEER in the early years of the study due to the adoption of the new code. Additionally, we lack data on the mitotic index or genomics of the tumors, including known drivers such as KIT, PDGFRα, and BRAF, which are commonly used as a variable for risk stratification.8 , 24 – 27 Therefore, we are unable to address that aspect of tumor biology and instead focus on tumor size and location as other variables for risk stratification.
In conclusion, the previous understanding of GIST <2 cm is derived from studies that have limited ability to assess the epidemiology and anatomic distribution of these tumors. The current study represents the first population-based analysis of malignant GIST <2 cm throughout the GI tract and identifies a mortality risk that has been underappreciated by gastroenterologists, surgeons, and oncologists. Further studies are needed to define the underlying reasons for the identified differences, to develop novel risk assessment schema for patients with these small tumors, and to determine appropriate indications for gastroenterologists to refer patients for resection and/or medical therapy.
Abbreviations
- 10M:
-
10,000,000
- ESMO:
-
European Society of Medical Oncology
- GIST:
-
Gastrointestinal stromal tumor
- ICC:
-
Interstitial cells of Cajal
- NCCN:
-
National Comprehensive Cancer Network
- SEER:
-
Surveillance, Epidemiology and End Results
References
Hirota S, Isozaki K, Moriyama Y, et al. Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science. 1998;279(5350):577–580.
DeMatteo RP, Lewis JJ, Leung D, Mudan SS, Woodruff JM, Brennan MF. Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survival. Ann Surg. 2000;231(1):51–58.
Roggin KK, Posner MC. Modern treatment of gastric gastrointestinal stromal tumors. World Journal of Gastroenterology: WJG. 2012;18(46):6720–6728.
Ma GL, Murphy JD, Martinez ME, Sicklick JK. Epidemiology of gastrointestinal stromal tumors in the era of histology codes: results of a population-based study. Cancer Epidemiology, Biomarkers & Prevention: a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2015;24(1):298–302.
Chetty R. Small and microscopically detected gastrointestinal stromal tumours: an overview. Pathology. 2008;40(1):9–12.
Dirnhofer S, Leyvraz S. Current standards and progress in understanding and treatment of GIST. Swiss Medical Weekly. 2009;139(7–8):90–102.
Rammohan A, Sathyanesan J, Rajendran K, et al. A gist of gastrointestinal stromal tumors: a review. World Journal of Gastrointestinal Oncology. 2013;5(6):102–112.
Demetri GD, von Mehren M, Antonescu CR, et al. NCCN Task Force report: update on the management of patients with gastrointestinal stromal tumors. Journal of the National Comprehensive Cancer Network: JNCCN. 2010;8 Suppl 2:S1-41; quiz S42-44.
Miettinen M, Lasota J. Gastrointestinal stromal tumors. Gastroenterology Clinics of North America. 2013;42(2):399–415.
Scherubl H, Faiss S, Knoefel WT, Wardelmann E. Management of early asymptomatic gastrointestinal stromal tumors of the stomach. World Journal of Gastrointestinal Endoscopy. 2014;6(7):266–271.
Abraham SC, Krasinskas AM, Hofstetter WL, Swisher SG, Wu TT. “Seedling” mesenchymal tumors (gastrointestinal stromal tumors and leiomyomas) are common incidental tumors of the esophagogastric junction. The American Journal of Surgical Pathology. 2007;31(11):1629–1635.
Agaimy A, Wunsch PH, Hofstaedter F, et al. Minute gastric sclerosing stromal tumors (GIST tumorlets) are common in adults and frequently show c-KIT mutations. The American Journal of Surgical Pathology. 2007;31(1):113–120.
Kawanowa K, Sakuma Y, Sakurai S, et al. High incidence of microscopic gastrointestinal stromal tumors in the stomach. Hum Pathol. 2006;37(12):1527–1535.
Chan CHF, Cools-Lartigue J, Marcus VA, Feldman LS, Ferri LE. The impact of incidental gastrointestinal stromal tumours on patients undergoing resection of upper gastrointestinal neoplasms. Canadian Journal of Surgery. 2012;55(6):366–370.
Rossi S, Gasparotto D, Toffolatti L, et al. Molecular and clinicopathologic characterization of gastrointestinal stromal tumors (GISTs) of small size. The American Journal of Surgical Pathology. 2010;34(10):1480–1491.
Tran T, Davila JA, El-Serag HB. The epidemiology of malignant gastrointestinal stromal tumors: an analysis of 1,458 cases from 1992 to 2000. Am J Gastroenterol. 2005;100(1):162–168.
Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: released April 2014 (updated 5/7/2014), based on the November 2013 submission.
Day JC. Population projections of the United States by age, sex, race, and Hispanic origin: 1995 to 2050. U.S. Bureau of the Census, Current Population Reports, P25-1130, U.S. Government Printing Office Washington, DC, 1996.
Tiwari RC, Clegg LX, Zou Z. Efficient interval estimation for age-adjusted cancer rates. Statistical Methods in Medical Research. 2006;15(6):547–569.
Murphy JD, Ma GL, Baumgartner JM, et al. Increased risk of additional cancers among patients with gastrointestinal stromal tumors: a population-based study. Cancer. 2015.
Miettinen M, Sobin LH, Lasota J. Gastrointestinal stromal tumors of the stomach: a clinicopathologic, immunohistochemical, and molecular genetic study of 1765 cases with long-term follow-up. The American Journal of Surgical Pathology. 2005;29(1):52–68.
Call J, Walentas CD, Eickhoff JC, Scherzer N. Survival of gastrointestinal stromal tumor patients in the imatinib era: life raft group observational registry. BMC Cancer. 2012;12:90.
Choi AH, Hamner JB, Merchant SJ, et al. Underreporting of gastrointestinal stromal tumors: is the true incidence being captured? Journal of Gastrointestinal Surgery: Official Journal of the Society for Surgery of the Alimentary Tract. 2015.
Miettinen M, Lasota J. Gastrointestinal stromal tumors: review on morphology, molecular pathology, prognosis, and differential diagnosis. Archives of Pathology & Laboratory Medicine. 2006;130(10):1466–1478.
Patil DT, Rubin BP. Genetics of gastrointestinal stromal tumors: a heterogeneous family of tumors? Surgical Pathology Clinics. 2015;8(3):515–524.
Rossi S, Gasparotto D, Miceli R, et al. KIT, PDGFRA, and BRAF mutational spectrum impacts on the natural history of imatinib-naive localized GIST: a population-based study. The American Journal of Surgical Pathology. 2015;39(7):922–930.
Kramer K, Knippschild U, Mayer B, et al. Impact of age and gender on tumor related prognosis in gastrointestinal stromal tumors (GIST). BMC Cancer. 2015;15:57.
Acknowledgments
The authors acknowledge the support of NIH TL1 TR001443 (K.E. Fero), NIH KL2 RR031978 (J.D. Murphy), and NIH K08 CA168999 (J.K. Sicklick).
Authors’ Contributions
There were no contributions to this manuscript by persons other than the authors. TMC and JKS were responsible for the study concept and design; TMC, KEF, and JDM for the acquisition of data; TMC, KEF, JDM, and JKS for the analysis and interpretation of data; TMC, KEF, CMT, JDM, and JKS for the drafting of the manuscript; TMC, KEF, PTF, RJM, CMT, JDM, and JKS for the critical revision of the manuscript for important intellectual content; KEF, JDM, and JKS for the statistical analysis; TMC, KEF, and JDM for the obtained funding; and JKS for the study supervision.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 70 kb)
Rights and permissions
About this article
Cite this article
Coe, T.M., Fero, K.E., Fanta, P.T. et al. Population-Based Epidemiology and Mortality of Small Malignant Gastrointestinal Stromal Tumors in the USA. J Gastrointest Surg 20, 1132–1140 (2016). https://doi.org/10.1007/s11605-016-3134-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-016-3134-y