Abstract
Background
Many studies on gastrointestinal stromal tumors (GISTs) derive from tertiary referral centers, but few examine strictly population-based cohorts. Thus, we evaluated the clinical features, surgical treatments, clinical outcomes, and factors predicting the survival of patients with GISTs in a population-based series.
Methods
Patients with GISTs diagnosed at Stavanger University Hospital over three decades (1980–2012) were analyzed. Data were retrieved from hospital records. Descriptive statistics and survival analyses (Kaplan–Meier) are presented. A limited number of colorectal GISTs (n = 6) restricted most analyses to those with a gastric or small bowel location.
Results
Among 66 patients surgically treated for GISTs, 60 patients (91 %) had either a gastric or a small bowel localization. Females comprised 61 %. The median age at diagnosis was 63 (range, 15–88) years. Clinical symptoms were recorded in 43 patients (65 %). Complete tumor resection was achieved in 85 % of the patients. During follow-up, 6 patients were surgically treated for local recurrence or metastatic disease. The median follow-up time was 6.1 years. At last follow-up, 30 patients (46 %) were deceased, 10 of whom died from GISTs. The median overall survival was 10.4 years. For GISTs with a gastric or small bowel location, a 1- and 5-year disease-specific survival of 100 and 96 %, and a relapse-free survival of 96 and 78 % were observed. Male gender, incidental diagnosis, smaller tumor size, a low mitotic rate, an intact pseudocapsule, low-risk categorization, and an early stage were significantly associated with improved outcomes.
Conclusion
Surgery in a low-volume, population-based setting yields enhanced long-term disease and recurrence-free survival for patients with GISTs of the stomach or small bowel. Incidental diagnosis, complete tumor resection, and low-risk categorization are good predictors of long-term prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastrointestinal stromal tumors (GISTs), although rare, are the most common non-epithelial neoplasms of the digestive tract [1, 2]. These tumors typically occur in the stomach or small bowel and are relatively infrequent elsewhere in the digestive tract and other locations [1–4]. GISTs account for less than 3 % of all gastrointestinal tumors but comprise nearly one-fifth of sarcomas and 80 % of gastrointestinal sarcomas [5–7]. The introduction of imatinib for the treatment of recurrent or metastatic GISTs in 2000, and later in the adjuvant setting, substantially improved selected patients’ outcomes. Nevertheless, complete surgical resection remains the gold-standard treatment for localized primary GISTs [3, 8–10].
Numerous clinical studies on GISTs have been published recently, mainly from tertiary referral centers, which may present an inherent selection bias. The present study evaluated the clinical features, surgical treatments, and clinical outcomes of patients with GISTs in a true population-based, single-institution consecutive series over the last three decades.
Materials and methods
Study population
Stavanger University Hospital (SUH) is the only hospital in its catchment area in southwestern Norway and provides healthcare services to a well-defined population that has increased from 220,000 individuals in 1980 to 340,000 in 2011 [11].
Study period and follow-up
The study period spanned 32 years, starting in January 1980, when a histopathological archive was established at SUH. Follow-up was performed on an individual basis, and clinical follow-up data were available for all patients. The follow-up was completed by May 2013. Patient demographics and clinical information were retrieved from hospital records, autopsy reports, and the official population registry. In the event of death, the details and cause of death were obtained from hospital records, including autopsy reports, when available, and from general practitioners.
Identification of patients and tumor characteristics
An experienced board-certified pathologist reviewed all mesenchymal tumors recorded in the pathology files at SUH over the last 32 years to identify eligible patients, as previously described in detail [12]. Lesions that had histomorphological and/or immunohistochemical profiles consistent with GISTs were included. Morphological tumor characteristics included tumor size, mitotic count, and tumor rupture [12, 13].
Definitions
Based on the symptoms and signs recorded at hospital admittance, each patient’s clinical presentation was assigned to one of the following three groups: a) acute illness with signs of peritonitis, ileus or significant gastrointestinal bleeding; b) relatively unspecific symptoms due to an abdominal mass with or without bleeding; and c) asymptomatic tumors incidentally diagnosed at surgery, endoscopy or radiology for other reasons or during histological examination of a specimen resected for another reason. Surgical resection margins were evaluated and classified as R0-R2 according to UICC standards [14].
The risk of disease progression was assessed according to the National Institute of Health (NIH) consensus criteria [15], the Armed Forces Institute of Pathology (AFIP) criteria [16], the modified NIH consensus (Joensuu) criteria [17, 18], and a recently published contour map [3]. The patients were grouped according to the 2010 UICC TNM classification [14]. Local recurrence was defined as the appearance of a gross tumor at the primary tumor site. Metastasis was defined as the appearance of a tumor distant from the resection site. Synchronous metastases were encountered at the time of diagnosis of the primary tumor or within the following 6 months. Overall survival (OS) was calculated from the day of diagnosis until death from any cause. Disease-specific survival (DSS) was defined as the time from gross complete resection until death from a GIST. Recurrence-free survival (RFS) was defined as the time from gross complete resection until the first tumor recurrence at any location.
Study ethics
The study was approved by the institution’s review board (ID No. 2009/1754) according to general guidelines provided by the Regional Ethics Committee.
Statistical analysis
A descriptive analysis was performed assuming a non-parametric distribution and using the χ 2 test or Fisher’s exact test, where appropriate, for dichotomous data and the Mann–Whitney U-test for continuous data. The data are reported as medians with ranges (or inter-quartile-ranges (IQRs)) for continuous variables or as rates/percentages for groups. Kaplan–Meier analysis was used to calculate survival curves, and survival was compared between groups using the log-rank test. All tests were two-tailed, and statistical significance was set at p < 0.05.
Results
Among 70 patients identified with GISTs during the study period, four patients were excluded (i.e., 2 had no surgery, 1 declined surgery, and 1 received neoadjuvant therapy, but surgery was not yet completed). Consequently, the study population comprised 66 patients, including 40 females (61 %), with primary GISTs. These patients had a median age of 63 (range, 15–88) years. The female preponderance was greater for tumor location in the small intestine. No significant difference in the median age at diagnosis was observed between genders. Patient demographics and clinical characteristics for 66 patients are summarized in Table 1.
Due to the small number of colon and rectum GISTs(n = 6), these patients were excluded from some analyses.
Clinical presentation
Clinical symptoms were encountered in 43 patients (65 %) (Table 1). Although symptomatic patients were younger (median, 62 years) compared to asymptomatic patients (median, 71 years), this difference did not reach statistical significance (p = 0.225). An acute diagnostic setting and emergency treatment were more frequently observed for small bowel tumors than for gastric GISTs (p = 0.029). Four of the incidental tumors were detected during acute surgery for unrelated conditions.
Tumor characteristics
Tumor distribution along the gastrointestinal tract is presented in Table 1. The median tumor diameter among all patients was 5.0 (range, 0.3–23) cm, with no statistically significant difference related to location between gastric and small bowel GISTs. Tumor diameters in the upper digestive tract were significantly larger among symptomatic patients compared with asymptomatic patients (median, 6.8 vs. 2.3 cm, respectively; p < 0.001). The median tumor diameter (7.1 cm; range, 1.8–23.0) among the 16 patients operated acutely for GISTs was similar to that of the 27 patients who underwent elective surgery (6.5 cm; range, 1.5–21.0).
Most tumors in both the stomach (64 %) and the small intestine (83 %) had a low mitotic rate (p = 0.150).
Tumor rupture was recorded in 2 gastric and 4 small bowel tumors (5 vs. 17 %; p = 0.288). Additionally, a similar perforation risk was observed between genders. The median age was 49 (range, 36–64) years, and the median tumor size was 10.8 (range, 6.2–18) cm among patients with tumor perforation.
Metastases
One patient with gastric GIST had lymph node involvement at diagnosis, and lymph node metastases were diagnosed during follow-up in another patient with a small bowel GIST. Four patients (1 stomach, 3 small bowel) had synchronous distant metastases, and 9 patients (6 stomach, 2 small bowel and 1 rectum) developed metachronous distant metastases. These patients had high-risk tumors according to the Joensuu criteria [17], with the exception of 1 intermediate-risk gastric GIST with metachronous metastases. The distribution into risk categories according to the aforementioned classification systems is given in Table 2 for the gastric and small bowel GISTs.
Surgery
Four patients (7 %), including 3 in the pre-imatinib era, underwent multivisceral resection. Combined total gastrectomy, splenectomy, distal pancreatectomy, and left hemicolectomy were the most extensive procedures performed in a single patient. However, most operations were limited open (or laparoscopic) resections, and typically gastric wedge resection or resection of short bowel segments.
Five gastric (14 %) and 10 small bowel (44 %) GISTs with acute clinical presentation were treated as surgical emergencies (p = 0.014; for separate comparison of these two groups). Complete resection (R0) was achieved in 32 patients (87 %) with gastric tumors, 19 patients (83 %) with small bowel, and 5 patients (83 %) with colorectal tumors, respectively. In total, 9 patients (14 %) had microscopically incomplete resection (R1), and 1 patient with a small bowel GIST had gross residual disease (R2) after surgery. Half of the patients (4/9) with R1 resection were operated on as emergencies.
Six patients (9 %) were surgically treated for local recurrence or metastatic disease, including one patient who required gastric wedge resection for local recurrence 4 years after the initial operation. Five patients underwent resections for metachronous metastatic disease, two of them repeatedly.
Postoperative mortality
Five patients (8 %), including 3 incidentally diagnosed patients, died in the hospital or within 30 days after surgery. The cause of death was postoperative abdominal sepsis (n = 3) or acute myocardial infarction (n = 2).
Systemic treatment
In total, 37 patients (58 %) were diagnosed with GISTs after the introduction of imatinib mesylate as a treatment option in 2001 [19]. Our first patient was offered palliative imatinib mesylate in September 2001, and 14 patients were eventually treated with a tyrosine kinase inhibitor (TKI). Two patients in the pre-TKI era received palliative conventional chemotherapy, 1 of them in combination with radiation for liver metastases.
Follow-up and survival
No patients were lost to follow-up. Half of the patients (n = 3) with colorectal GISTs died during the study period, 1 of them from disseminated disease.
The median follow-up time for 60 patients with gastric or small bowel location was 6.9 (IQR, 2.6–10.7) years. During follow-up, 27 (45 %) of these patients died, and an advanced or progressive GIST was the cause of death in 9 cases (9/27 = 33 %). Eleven patients, including 6 males and 5 females, had recurrent disease, and eventually 8 of these 11 patients died from the disease.
Overall survival (OS)
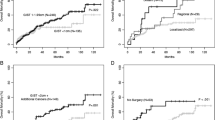
The median OS was 10.3 years (95 % confidence interval (CI) 5.1–15.5). The 1- and 5-year OS rates were 92 and 80 %, respectively (Figs. 1 and 2). In univariate survival analyses, male gender and younger age was associated with significantly better OS.
In the analyses of DSS and RFS, 1 patient with an R2 resection, who died of abdominal sepsis on the first postoperative day, was excluded.
Disease-specific survival (DSS)
The 1- and 5-year DSS rates were 100 and 96 %, respectively (Fig. 2). Smaller tumor size was significantly associated with longer DSS, as was the absence of tumor perforation. Additionally, low-risk classification [3, 15–18] and an early stage according to the UICC criteria of disease [14] indicated better outcomes.
Relapse-free survival (RFS)
The 1- and 5-year RFS rates were 96 and 78 %, respectively (Fig. 2). Male gender, smaller tumor size, a low mitotic rate, an intact pseudocapsule, incidental diagnosis, low-risk categorization, and an early stage were all significantly associated with a longer RFS in univariate analyses.
Discussion
This population-based study on surgery for GISTs highlights the overall good prognosis and outcomes of a disease that is often incidentally detected and treated in a community setting. Most patients with GISTs presented with limited disease and low-to-moderate risk, and surgery generally provided a long-term cure. This result contrasts with reports in the surgical literature, which have often analyzed patient series at tertiary referral centers that receive and treat more overt, aggressive, and complex GISTs. However, the importance of an intact pseudocapsule and the favorable outcomes observed in low-risk categories are comparable with the results of previous surgical series [8, 20–23].
GISTs have been reported in all age groups but are rare in patients younger than 30 years. The age distribution in this study, with a median of approximately 63 years, was similar to distributions in other reports [3]. The tumor distribution along the gastrointestinal tract was also similar to that of other studies, with most located in the stomach [3].
Localized primary GISTs are best treated with complete surgical resection [3, 8, 9], and a large proportion of patients can be cured by surgery alone. However, disease relapse may occur in up to 40 % of patients [3]. Adjuvant treatment with TKIs can increase RFS and prolong survival among high-risk patients [24–26]. Notably, adjuvant treatment with TKIs may also cause adverse effects and increase costs. Therefore, estimation of recurrence risk is important to optimize the management of operable GISTs.
Tumor size, the mitotic rate, the tumor site, and tumor perforation are recognized as risk factors for recurrence [3, 4, 8, 27–29]. Tumor size, the mitotic rate, and tumor perforation were also identified as significant factors in the present study, whereas the tumor site was not, possibly due to the small sample size. Additionally, classification into a high-risk group served as a negative prognostic factor for all included risk stratification systems. Patients with incidentally diagnosed GISTs demonstrated a significantly better prognosis (for RFS, not DSS) than did patients with symptomatic tumors, which may be explained by the smaller tumor size of incidentally diagnosed GISTs, as tumor size is an important prognosticator.
With a median OS of 10 years and 1- and 5-year DSS rates of 100 and 96 %, respectively, the prognosis of patients with GISTs is regarded as favorable. In fact, the DSS results of the current study are better than those reported for a large Memorial Sloan-Kettering series, with 1- and 5-year DSS rates of 88 and 54 %, respectively [8]. Clearly, patient selection, referral patterns, and the treatment period (1982–1998) differed between the studies, so the results are not immediately comparable. As such, the observed 1- and 5-year RFS rates of 96 and 78 %, respectively, may seem high but are consistent with a recent large, pooled dataset from Europe and Japan [3].
The well-defined, population-based study sample and the long-term follow-up represent strengths of this study. Additionally, the thorough re-evaluation and classification of archived specimens’ morphology based on contemporary criteria for correct diagnosis and proper risk evaluation contributed to the study’s consistency.
The current study’s limitations include its retrospective design and long inclusion timespan, during which considerable changes and improvements in routine preoperative imaging, primary treatment, and treatment options for recurrent or advanced disease occurred. The overall patient number was small, yet this size reflects a true population-based approach to management of this disease. The limited number of patients and the few endpoints for the investigated outcomes (i.e. survival) prevented the use of multivariate regression analyses, as these would have been fraught with uncertainty and large CIs.
The interventions’ heterogeneity over time and differences in the case-mix, as shown in comparable studies [3, 8], make it difficult to draw firm conclusions. Nevertheless, our results from a non-selected population-based series add to core knowledge on the management of this relatively rare malignant entity. Multidisciplinary collaboration to enable correct preoperative diagnosis and staging for appropriate primary surgical treatment, including neoadjuvant and/or adjuvant treatment, as indicated, are important for improving the standard of care for patients with GISTs in the future.
References
Miettinen M, Lasota J (2011) Histopathology of gastrointestinal stromal tumor. J Surg Oncol 104:865–873
Joensuu H, Hohenberger P, Corless CL (2013) Gastrointestinal stromal tumour. Lancet 382:973–983
Joensuu H, Vehtari A, Riihimaki J et al (2012) Risk of recurrence of gastrointestinal stromal tumour after surgery: an analysis of pooled population-based cohorts. Lancet Oncol 13:265–274
Miettinen M, Sobin LH, Lasota J (2005) Gastrointestinal stromal tumors of the stomach: a clinicopathologic, immunohistochemical, and molecular genetic study of 1765 cases with long-term follow-up. Am J Surg Pathol 29:52–68
Katz SC, DeMatteo RP (2008) Gastrointestinal stromal tumors and leiomyosarcomas. J Surg Oncol 97:350–359
Steigen SE, Eide TJ (2009) Gastrointestinal stromal tumors (GISTs): a review. APMIS 117:73–86
Ducimetière F, Lurkin A, Ranchère-Vince D et al (2011) Incidence of sarcoma histotypes and molecular subtypes in a prospective epidemiological study with central pathology review and molecular testing. PLoS 6(8):e20294
DeMatteo RP, Lewis JJ, Leung D et al (2000) Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survival. Ann Surg 231:51–58
Demetri GD, von Mehren M, Antonescu CR et al (2010) NCCN Task Force report: update on the management of patients with gastrointestinal stromal tumors. J Natl Compr Canc Netw 8(Suppl 2):S1–S41 quiz S42–S44
ESMO/European Sarcoma Network Working Group (2012) Gastrointestinal stromal tumors: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 23(Suppl 7):vii49–vii55
Statistics Norway, Oslo (2011) http://www.ssb.no/en/helse. Accessed 12 Oct 2013
Sandvik OM, Søreide K, Kvaløy JT et al (2011) Epidemiology of gastrointestinal stromal tumours: single-institution experience and clinical presentation over three decades. Cancer Epidemiol 35:515–520
Søreide K, Sandvik OM, Søreide JA et al (2012) Tyrosine-kinase mutations in c-KIT and PDGFR-alpha genes of imatinib naive adult patients with gastrointestinal stromal tumours (GISTs) of the stomach and small intestine: relation to tumour-biological risk-profile and long-term outcome. Clin Transl Oncol 14:619–629
Sobin LH, Gospodarwoicz MK, Wittekind C (2009) TNM classification of malignant tumours. Wiley, Hoboken
Fletcher CD, Berman JJ, Corless C et al (2002) Diagnosis of gastrointestinal stromal tumors: a consensus approach. Hum Pathol 33:459–465
Miettinen M, Lasota J (2006) Gastrointestinal stromal tumors: pathology and prognosis at different sites. Semin Diagn Pathol 23:70–83
Joensuu H (2008) Risk stratification of patients diagnosed with gastrointestinal stromal tumor. Hum Pathol 39:1411–1419
Rutkowski P, Bylina E, Wozniak A et al (2011) Validation of the Joensuu risk criteria for primary resectable gastrointestinal stromal tumour–the impact of tumour rupture on patient outcomes. Eur J Surg Oncol 37:890–896
Joensuu H, Roberts PJ, Sarlomo-Rikala M et al (2001) Effect of the tyrosine kinase inhibitor STI571 in a patient with a metastatic gastrointestinal stromal tumor. N Engl J Med 344:1052–1056
Kim KM, Kang DW, Moon WS et al (2005) Gastrointestinal stromal tumors in Koreans: it’s incidence and the clinical, pathologic and immunohistochemical findings. J Korean Med Sci 20:977–984
Steigen SE, Eide TJ (2006) Trends in incidence and survival of mesenchymal neoplasm of the digestive tract within a defined population of northern Norway. APMIS 114:192–200
Chan KH, Chan CW, Chow WH et al (2006) Gastrointestinal stromal tumors in a cohort of Chinese patients in Hong Kong. World J Gastroenterol 12:2223–2228
Tzen CY, Wang JH, Huang YJ et al (2007) Incidence of gastrointestinal stromal tumor: a retrospective study based on immunohistochemical and mutational analyses. Dig Dis Sci 52:792–797
Dematteo RP, Ballman KV, Antonescu CR et al (2009) Adjuvant imatinib mesylate after resection of localised, primary gastrointestinal stromal tumour: a randomised, double-blind, placebo-controlled trial. Lancet 373:1097–1104
Joensuu H, Eriksson M, Hall KS et al (2012) One vs. three years of adjuvant imatinib for operable gastrointestinal stromal tumor: a randomized trial. JAMA 307:1265–1272
Dematteo RP, Ballman KV, Antonescu CR et al (2013) Long-term results of adjuvant imatinib mesylate in localized, high-risk, primary gastrointestinal stromal tumor: ACOSOG Z9000 (Alliance) Intergroup Phase 2 Trial. Ann Surg 258:422–429
Miettinen M, Makhlouf H, Sobin LH et al (2006) Gastrointestinal stromal tumors of the jejunum and ileum: a clinicopathologic, immunohistochemical, and molecular genetic study of 906 cases before imatinib with long-term follow-up. Am J Surg Pathol 30:477–489
Dematteo RP, Gold JS, Saran L et al (2008) Tumor mitotic rate, size, and location independently predict recurrence after resection of primary gastrointestinal stromal tumor (GIST). Cancer 112:608–615
Hohenberger P, Ronellenfitsch U, Oladeji O et al (2010) Pattern of recurrence in patients with ruptured primary gastrointestinal stromal tumour. Br J Surg 97:1854–1859
Funding
None.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sandvik, O.M., Søreide, K., Gudlaugsson, E. et al. Surgery for Gastrointestinal Stromal Tumors (GISTs) of the Stomach and Small Bowel: Short- and Long-Term Outcomes Over Three Decades. World J Surg 39, 446–452 (2015). https://doi.org/10.1007/s00268-014-2824-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-014-2824-4