Abstract
Background
The aim of the study was to evaluate whether ultra-low-dose computed tomography (ULD-CT) could replace conventional-dose CT (CD-CT) for diagnosis of acute wrist, ankle, knee, and shoulder fractures in emergency departments (ED).
Methods
We developed CD-CT and ULD-CT scanning schemes for the various joints of the four limbs and scanned emergency patients prospectively. When performing CD-CT, a conventional bone reconstruction algorithm was used, while ULD-CT used both soft tissue and bone algorithms. A five-point scale was used to evaluate whether ULD-CT image quality affected surgical planning. The image quality and diagnostic performance of different types of scanned and reconstructed images for diagnosing fractures were evaluated and compared. Effective radiation dose of each group was calculated.
Results
Our study included 56 normal cases and 185 fracture cases. The combination of bone and soft tissue algorithms on ULD-CT can improve diagnostic performance, such that on ULD-CT, the sensitivity improved from 96.7% to 98.9%, specificity from 98.2% to 100%, positive predictive value from 99.4% to 100%, negative predictive value from 90.2% to 96.6% and diagnostic accuracy ranged from 97.5% to 99.1%. There were no statistically significant differences between ULD-CT and CD-CT on diagnostic performance (p values, 0.40–1.00). The radiation doses for ULD-CT protocols were only 3.0–7.7% of those for CD-CT protocols (all p < 0.01).
Conclusions
In the emergency department, the 320-row detector ULD-CT could replace CD-CT in the diagnosis of limb joint fractures. The combination of bone algorithm with soft tissue algorithm reconstruction can further improve the image quality and diagnostic performance.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Missed fractures have been found to account for up to 79.7% of missed diagnosis in an emergency department (ED) [1]. Although digital radiography (DR) is the first-line diagnostic tool in suspected traumatic injury, computed tomography (CT) is superior for examining axial skeleton and extremity components, as well as detecting subtle fractures [2,3,4]. Furthermore, in circumstances when conventional radiography observations of callus production are less clear, computed tomography may be particularly useful in monitoring metaphyseal and periarticular fracture-healing [5]. As doctors expect accurate diagnostic tests and detailed images to depict injuries and diseases before deciding on future therapy, the need for “high-end” diagnostic imaging, notably CT, has expanded tremendously. Between 1993 and 2007, the number of CT scans performed in ED in the United States climbed by 300%, reaching 71.7 million [6].
The advantages of using CT must, however, be balanced against the risk of increased ionizing radiation exposure, which is the primary safety concern while having a CT scan or working in an emergency department [7]. Unfortunately, as CT is utilized more extensively in emergency medicine in the pursuit of more accurate diagnostic images, the radiation dose received by emergency department patients is increasing, potentially may raising the lifetime cancer risk to one in seventeen [8]. Patients with acute fractures are more likely to have CT at the first visit and follow-up. It is essential to minimize the radiation dose of emergency department CT examinations while maintaining the benefits of performing CT. Several studies have recently revealed that low-dose and ultra-low-dose CT approaches for the diagnosis of fractures or traumas have radiation doses that are significantly decreased or even comparable to DR [9,10,11]. However, current low-dose trials have only demonstrated superiority over DR in fracture diagnosis, and there is a lack of data comparing the diagnostic performance of conventional-dose CT in emergency departments.
Therefore, in this study, we developed and assessed various ULD-CT schemes for the shoulder, knee, wrist, and ankle joints in the emergency medical practice. Moreover, we seek to increase the diagnostic performance of ULD-CT by incorporating soft tissue algorithm reconstruction, as prior research solely applied a bone algorithm reconstruction to evaluate bone health and orthopedic diseases. It is the first report that an extra soft tissue algorithm reconstruction images were used for limb fractures diagnosis in an emergency department. We assume that this ULD-CT protocol can reduce the radiation dose to a level comparable to DR, while maintaining the same diagnostic performance as the CD-CT in emergency department.
Methods
Study population
This prospective study was approved by the Ethics Committee of our hospital (BF2019-030-01). All patients gave written informed consent for the acquisition of ultra-low-dose CT (ULD-CT) after a clinically indicated conventional-dose CT (CD-CT). From November 30, 2019 to October 25, 2020, we consecutively enrolled 247 patients who underwent CT scans (CD-CT and ULD-CT) with musculoskeletal complaints after trauma in the emergency department (ED). Six patients were excluded who had pain due to other causes, such as systemic diseases involving the musculoskeletal system, tumorous conditions or infectious diseases. Finally, our study was consisted of 241 patients with 62 shoulder cases, 48 knee cases, 65 ankle cases and 66 wrist cases. There were 96 males and 145 females ranging in age from 20 to 86 years (mean age, 52.99 ± 15.11 years) enrolled in the study. The study included 56 normal cases and 185 fractures cases, with 107 patients receiving surgical treatment and 78 patients receiving conservative treatment. The final diagnosis was made through surgical findings for the surgical patients and comparing preliminary reports between CD-CT and ULD-CT for the non-operative fracture patients.
Scanning methods
All scans were performed using a Canon 320-row detector CT device (Aquilion One Vision Edition; Canon Medical Systems, Otawara, Japan). All the patients were examined in a supine position. For ankle assessments, the affected leg was extended into the gantry while the contralateral leg remained outside of the gantry. For the knee examinations, patients were situated in the middle of CT table with feet together. For the wrist assessments, the affected arm was extended above the head into the gantry. For the shoulder examinations, patients were situated in the middle of CT table with arms hanging naturally. For the shoulder, knee, ankle, and wrist, the CD-CT scanning parameters were 120 kV tube voltage and 150, 120, 120, and 50 mAs tube currents, respectively; while the ULD-CT scanning parameters were 80 kV tube voltage and 52, 11, 11, and 4 mAs tube currents, respectively. Table 2 shows the scanning conditions for each group. The scanner software automatically calculated the volume CT dose index (mGy) and dose-length product (DLP; mGy × cm) for all CT protocols. The DLP was then multiplied by k (a conversion coefficient) to obtain the effective dose (i.e., effective dose = DLP × k) for each patient. The k values for the ankle and wrist were both 0.0002, and the k value for the knee was 0.0004. At tube voltages of 80 and 120 kV, the k values for the shoulder were 0.0091 and 0.0113, respectively [12].
Image processing and analysis
Bone algorithm (kernel FC35) iterative reconstruction (AIDR 3D, Canon Medical Systems) was performed on CD-CT, while both bone algorithm and soft tissue algorithm (kernel FC08) were performed on ULD-CT (Table 2).
To quantify the CT values and standard deviation (SD) in the Hounsfield unit, a region of interest (ROI) was created within the medullary section of the muscle. The ROI was 1 cm in diameter. On a coronal image, the ROIs were located at the humeral head of the shoulder joint, the metaphysis of the distal femur of knee the metaphysis of the distal tibia of the ankle joint, the metaphysis of the distal radius of the wrist joint and muscle at the thickest cortex of each joint. The CT values and SD were calculated by two radiologists in consensus. The contrast-to-noise (CNR) and signal-to-noise (SNR) ratios were calculated as follows: SNR = CTjoint mean/SDjoint mean, CNR = (CTjoint mean − CTmucle mean)/SDjoint mean.
The subjective image quality was evaluated by two experienced musculoskeletal radiologists who were blinded to the scan and reconstruction parameters; the quality was rated on a five-point system from 1 to 5: 5 = excellent (excellent images quality without any artifacts); 4 = good (good images quality with slight artifacts and noise); 3 = adequate (adequate images quality with comparative artifacts and noise, but not interfering with diagnostic quality); 2 = poor (poor images quality, interfering with diagnostic quality by severe artifacts and noise); 1 = very poor (unclear images; impossible to diagnose). In addition, the two experienced were responsible for reporting location of the fracture and number of fracture fragments (Table 1) and the ULD-CT reports description were based on the combination of bone and soft tissue algorithms reconstruction images.
To assess the impact of ULD-CT on treatment choices, one independent experienced orthopedic surgeon retrospectively reviewed the reports from the cases compared to CD-CT. For the patients scheduled for surgery, two experienced orthopedic surgeons who were blinded to the scan and reconstruction parameters, evaluated the effects of three-dimensional reconstruction images on preoperative plan, and rated using a five-point scale from 1 to 5: 5 = excellent (very good visualization of the fracture line and fragments locations; excellent definition of fracture types; appropriate for preoperative assessment); 4 = good (good visualization of the fracture line and fragments locations with slight artifacts and noise; good definition of fracture types; appropriate for preoperative assessment); 3 = adequate (adequate visualization of the fracture line and fragments locations, slightly affected by comparative artifacts and noise; adequate definition of fracture types without influence from images noise; adequate for preoperative assessment, slightly affected by comparative artifacts and noise); 2 = poor (poor images quality; interfering with visualization of the fracture line, fragments locations, definition of fracture types and preoperative assessment by severe artifacts and noise; 1 = very poor (unclear images; not appropriate for preoperative assessment).
Statistical analysis
Statistical analyses were performed using IBM SPSS Statistics, version 26.0 (IBM Corp., Armonk, NY, USA). The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and diagnostic accuracy for diagnosing fracture were calculated. The Chi-square test and ANOVA were employed to compare the scores of image quality. The intra-class correlation coefficient (ICC)was used to analyze the inter-observer agreement in the qualitative evaluation, such that ICC values < 0.4 was poor, 0.41–0.6 was moderate, 0.61–0.8 was substantial, and 0.81–1.00 was near-perfect agreement. Differences with p values < 0.05 were considered statistically significant.
Results
The study included 56 normal cases and 185 fractures cases (including 43 simple fractures and 142 comminuted fractures, with one simple avulsion fracture of the wrist, five simple avulsion fractures of the ankle, one simple avulsion fracture of the shoulder, and two simple avulsion fractures of the knee) with 107 patients receiving surgical treatment and 78 patients receiving conservative treatment. In summary, there were total 347 fractures were found in 185 patients, with 70 shoulder fractures in 62 patients, 50 knee fractures in 48 patients, 104 ankle fractures in 65 patients, and 123 wrist fractures in 66 patients.
The CT value of the bones were significantly higher in the ULD-CT group than in the CD-CT group (p < 0.05) (Table 2); notably, the noise was lowest with soft tissue algorithm reconstruction, accompanied by highest values of SNR and CNR in the ultra-low-dose group (Table 3). Subjective image scores were significant higher on CD-CT protocol which was rated five points in all scanned cases by two readers. Six cases were rated two points on ULD-CT bone algorithm reconstruction images by two readers and the remaining bone algorithm reconstruction images were ≥ 3 points (2.99 ± 0.26). All ULD-CT soft tissue algorithm images were assigned ≥ 3 points that met the clinical diagnosis criteria (3.74 ± 0.46).
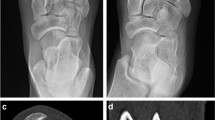
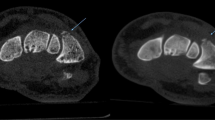
Both reader 1 and reader 2 missed one same ankle fractures on CD-CT (Fig. 2). Reader 1 missed two ankle fractures, one shoulder fracture and two wrist fractures on bone algorithm ULD-CT, while missed two ankle fractures, one shoulder fracture and three wrist fractures on soft tissue algorithm. However, when the two algorithms reconstruction methods were combined, the diagnostic performance improved. Reader 1 only missed two ankle fractures when using both bone and soft tissue algorithms reconstruction images. Reader 2 presented a similar scenario: he missed two ankle fractures, one shoulder fracture and three wrist fractures on bone algorithm ULD-CT, while missed two ankle fractures, one shoulder fracture and two wrist fractures on soft tissue algorithm ULD-CT. Combining both bone and soft tissue algorithms ULD-CT, he only missed two ankle fractures. In addition, reader 2 misdiagnosed one wrist fractures on soft tissue algorithm ULD-CT.
When compared to the bone algorithm or the soft tissue algorithm alone, the combination of bone and soft tissue algorithms on ULD-CT can improve diagnostic performance, such that on ULD-CT, the sensitivity improved from 96.7% to 98.9%, specificity from 98.2% to 100%, positive predictive value from 99.4% to 100%, negative predictive value from 90.2% to 96.6% and diagnostic accuracy ranged from 97.5% to 99.1%. On CD-CT, the sensitivity, specificity, PPV, NPV and diagnostic accuracy were 99.5%, 100%, 100%, 98.2% and 99.6%, respectively (Table 2). There were no statistically significant differences between ULD-CT and CD-CT in terms of sensitivity, specificity, PPV, NPV or diagnostic accuracy (p values, 0.40–1.00).
ULD-CT did not change any treatment option from the CD-CT. Furthermore, there was no significant difference of preoperative plan scores among CD-CT, ULD-CT bone algorithm and ULD-CT soft tissue algorithm (5.00 ± 0.00, 4.98 ± 0.12, 4.96 ± 0.19, respectively, all p < 0.01). The ICCs showed near-perfect agreement between readers for evaluating subjective image quality and preoperative plan for all joints (ICCs, 0.81–0.99).
The radiation doses for ULD-CT protocols were only 3.0–7.7% of those for CD-CT protocols, which were significantly lower than CD-CT and were listed as follows: on ULD-CT, the effective radiation doses for shoulder, knee, ankle, and wrist were 228.91 ± 26.25 μSv, 2.13 ± 0.1 μSv, 1.06 ± 0.11 μSv and 0.29 ± 0.07 μSv, respectively; on CD-CT, the effective radiation doses were 2252.64 ± 126.73 μSv, 72.82 ± 3.21 μSv, 35.68 ± 3.64 μSv, 10.53 ± 2.28 μSv, respectively (Table 1).
Discussion
Radiation exposure to patients has received more attention for the past few years, as excess cancer risks are closely associated to radiation dose [13, 14]. However, the quality of image diagnosis is considered generally in emergency department therapy, which presents a challenge to imaging equipment. Recent studies have looked investigating ways to lower CT radiation exposure while maintaining image quality. According to Yi et al. [15], a 50% reduction in radiation dose did not influence image quality or fracture detection performance by utilizing a 64 row multi-detector CT scanner, when compared to standard-dose CT. Previous studies have revealed that while examining tissues surrounding bone fractures with “high-end” CT equipment, the average low-dose CT radiation exposure was 0.53–800 μSv for various single joints, which is comparable or slightly more than that of DR [9, 16, 17].
We have already had the experience of using a 320-row detector CT scanner to diagnose distal radial fractures at ultra-low-dose protocol (80 kV, 4 mAs) that the radiation dose was less than DR [18]. Following previous experience, we set the scanning scheme of 80 kV tube voltages and corresponding appropriate low tube currents to the limb joints in accordance with the “ALARA” radiation safety guiding concept, which stands for “as low as reasonably achievable” (Table 1). In this study, the effective radiation doses to the shoulder, knee, ankle, and wrist joints on ULD-CT were 228.91 ± 26.25 μSv, 2.13 ± 0.18 μSv, 1.06 ± 0.11 μSv and 0.29 ± 0.07 μSv, respectively; and equivalent to only 7.68%, 4.41%, 2.97%, and 2.73% of the conventional radiation doses (p < 0.001). Furthermore, except for shoulder imaging, the abovementioned ULD-CT has a comparable or even lower (wrist imaging) radiation dose than the matching site DR [9, 19].
In emergency practice, image quality and radiation dose must be considered, which not only protects patients and radiologists, but also improves the accuracy of future clinical decisions. CT scan image quality is likely to be altered not just by mechanical parameters such as kVp or mAs, but also by biological factors such as bone density or soft tissue thickness [9]. In general, the bone algorithm image is employed for bone disease detection and has a higher image contrast. The soft tissue algorithm focuses on soft tissue presentation, consequently image noise is reduced. Therefore, we are working to improve the diagnostic performance of ULD-CT by integrating bone algorithm and soft tissue algorithm reconstruction to mitigate the effect of high images noise generated by low dose. In the study, the image noise increased and objective image values decreased at each joint as the radiation dose was reduced significantly of ULD-CT with the conventional bone algorithm reconstruction, when compared to CD-CT group. Soft algorithm reconstruction, on the other hand, improved the objective image quality (Table 3), and when combining soft tissue algorithm, all ULD-CT images were assigned ≥ 3 points (3.74 ± 0.46), indicating that they satisfied the clinical diagnosis requirements, whereas six cases received a score of two points based on ULD-CT bone algorithm reconstruction images alone. There was no significant difference of preoperative plan scores among CD-CT, ULD-CT bone algorithm and ULD-CT soft tissue algorithm (5.00 ± 0.00, 4.98 ± 0.12, 4.96 ± 0.19, respectively, all p < 0.01). The ICCs showed near-perfect agreement between readers for evaluating subjective image quality and preoperative plan for all joints (ICCs, 0.81–0.99).
Previous research comparing the diagnostic performance of ultra-low-dose and conventional-dose emergency department CT in the diagnosis of extremity fractures has been lacking. Our results showed that reader 1 and reader 2 missed five and six fractures on ULD-CT bone algorithm, respectively; while they missed six and five fractures on ULD-CT soft tissue algorithm, respectively. However, the cases missed by the bone algorithm and the soft tissue algorithm; on the other hand, do not overlap (Figs. 1, 2 and 3). The combination of bone algorithm and soft tissue algorithm improved the diagnostic performance on ULD-CT, when compared to bone algorithm and soft algorithm alone; and the diagnostic performance was comparable to the CD-CT (Table 2). Furthermore, our ULD-CT reports description were generated from the combination of bone and soft tissue algorithms reconstruction images. Considering that we reviewed the reports retrospectively, therefore, we did not focus on the impact of the separate report generated from each algorithm on treatment selection. However, in our case, if an individual algorithm of ULD-CT is employed to generate a report, clinical decision-making is likely to change (Figs. 2 and 3). The missed fractures of the actual ULD-CT reports, on the other hand, were subtle fractures that were accompanied by other fractures in the same case in our study. A change in treatment strategy is unlikely as a result of this missed diagnosis. Therefore, based on our experience, ULD-CT combined with the two reconstruction algorithms may have a high chance of avoiding treatment options changes, when CD-CT reports were regarded as reference standard.
A 32-year-old man had sprained his right ankle 10 h before and presented to the emergency department with swelling and limited movement. CD-CT images showed the displacement fracture of the lateral malleolus (white arrow). However, reader 1 and reader 2 both missed the avulsion fracture of lateral margin of the talus (red arrows), which were confirmed by the subsequent surgery. (A-1) Coronal image of CD-CT. (A-2) Partial enlargement image of A-1. B Axial image of CD-CT
A 42-year-old woman fell from a great height, landing on his right hand and hip, developing pain in his lower back and right wrist, as well as limited movement, and presenting 3 days later to the emergency department. Reader 1 missed the avulsion fracture of scaphoid of wrist (white arrows) on ULD-CT soft tissue algorithm reconstruction images (A). However, he did not miss the diagnosis on ULD-CT bone algorithm reconstruction images (B) and the CD-CT images (C)
After a fall, a 54-year-old male reported to the emergency department with right shoulder joint pain and limited mobility for 1 day. On ULD-CT bone reconstruction images (A) reader 2 missed the avulsion fracture of the humeral head (white arrows), but not on ULD-CT soft tissue reconstruction images (B) or the CD-CT images (C)
Both algorithms have benefits and drawbacks. Soft tissue algorithms have poor spatial resolution but benefit from reduced noise, whereas bone algorithm offers high spatial resolution but suffers from more noise. The use of both techniques together can expand the range of low-dose scans, optimize image quality, and benefit both patients and radiologists. This is the only study that we are aware of that uses a soft tissue algorithm for emergency department to diagnosis fracture at a lower radiation CT dosage than previous research [2, 9,10,11, 18,19,20,21,22]. The excellent diagnostic performance of this study provides clinical evidence for the use of ultra-low-dose protocol on 320-row detector CT in the ED for the diagnosis of limb joint fractures.
There were certain limitations to our research. First, we did not compare CT to DR in this study. The certain flaw in this research methodology is that the examination cost is larger than DR. Second, we did not compare the operative quality and postoperative recovery condition of CD-CT and ULD-CT surgical patients, and the impact of ULD-CT on the quality and flow of surgery are unknown. Third, visual assessment was not performed in the real ER scenario due to the retrospective analysis. Results may have been biased by the current readers in the 'peaceful' environment. At last, the reading time was not recorded and compared in this study. The time it takes to diagnose a patient with an ultra-low-dose CT with different reconstruction algorithms may be affected.
Conclusions
In conclusion, the ultra-low-dose protocol can successfully minimize the radiation dose, which is comparable to DR, while maintaining diagnostic image quality for limb joint fracture detection. Furthermore, by combining the bone and soft tissue algorithms on ULD-CT, the diagnostic performance of CD-CT can be achieved. This ultra-low-dose imaging technique using a 320-row detector CT may be able to substitute CD-CT in the emergency department for the diagnosis of limb joint fractures.
Abbreviations
- CT:
-
Computed tomography
- DR:
-
Digital radiography
- ULD-CT:
-
Ultra-low-dose CT
- CD-CT:
-
Conventional dose CT
- ED:
-
Emergency department
- DLP:
-
Dose-length product
- SD:
-
Standard deviation
- ROI:
-
Region of interest
- CNR:
-
Contrast-to-noise
- SNR:
-
Signal-to-noise
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
- ICC:
-
Intra-class correlation coefficient
References
Guly HR. Diagnostic errors in an accident and emergency department. Emerg Med J. 2001;18(4):263–9.
Cuddy K, et al. Use of intraoperative computed tomography in craniomaxillofacial trauma surgery. J Oral Maxillofac Surg. 2018;76(5):1016–25.
Matsuoka S, et al. Three-dimensional computed tomography and indocyanine green-guided technique for pulmonary sequestration surgery. Gen Thorac Cardiovasc Surg. 2021;69(3):621–4.
Xia H, et al. Application of rib surface positioning ruler combined with volumetric CT measurement technique in endoscopic minimally invasive thoracic wall fixation surgery. Exp Ther Med. 2020;20(2):1616–20.
Morshed S, et al. Outcome assessment in clinical trials of fracture-healing. J Bone Joint Surg Am. 2008;90(Suppl 1):62–7.
Larson DB, et al. National trends in CT use in the emergency department: 1995–2007. Radiology. 2011;258(1):164–73.
Azman RR, Shah MNM, Ng KH. Radiation safety in emergency medicine: balancing the benefits and risks. Korean J Radiol. 2019;20(3):399–404.
Griffey RT, Sodickson A. Cumulative radiation exposure and cancer risk estimates in emergency department patients undergoing repeat or multiple CT. AJR Am J Roentgenol. 2009;192(4):887–92.
Alagic Z, et al. Ultra-low-dose CT for extremities in an acute setting: initial experience with 203 subjects. Skeletal Radiol. 2020;49(4):531–9.
Hamard A, et al. Ultra-low-dose CT versus radiographs for minor spine and pelvis trauma: a Bayesian analysis of accuracy. Eur Radiol. 2021;31(4):2621–33.
Weinrich JM, et al. MDCT in suspected lumbar spine fracture: comparison of standard and reduced dose settings using iterative reconstruction. Clin Radiol. 2018;73(7):675 e9-e15.
Saltybaeva N, et al. Estimates of effective dose for CT scans of the lower extremities. Radiology. 2014;273(1):153–9.
Brenner DJ, Hall EJ. Computed tomography–an increasing source of radiation exposure. N Engl J Med. 2007;357(22):2277–84.
Lin EC. Radiation risk from medical imaging. Mayo Clin Proc. 2010;85(12):1142–6.
Yi JW, et al. Radiation dose reduction in multidetector CT in fracture evaluation. Br J Radiol. 2017;90(1077):20170240.
Mansfield C, et al. Optimizing radiation dose in computed tomography of articular fractures. J Orthop Trauma. 2017;31(8):401–6.
Konda SR, et al. Ultralow-dose CT (reduction protocol) for extremity fracture evaluation is as safe and effective as conventional CT: an evaluation of quality outcomes. J Orthop Trauma. 2018;32(5):216–22.
Xiao M, et al. Application of ultra-low-dose CT in 3D printing of distal radial fractures. Eur J Radiol. 2021;135:109488.
Brink M, et al. Single-shot CT after wrist trauma: impact on detection accuracy and treatment of fractures. Skeletal Radiol. 2019;48(6):949–57.
Halvachizadeh S, et al. Is the additional effort for an intraoperative CT scan justified for distal radius fracture fixations? A comparative clinical feasibility study. J Clin Med. 2020;9(7):2254.
Elegbede A, et al. Low-dose computed tomographic scans for postoperative evaluation of craniomaxillofacial fractures: a pilot clinical study. Plast Reconstr Surg. 2020;146(2):366–70.
Konda SR, et al. The use of ultra-low-dose CT scans for the evaluation of limb fractures: is the reduced effective dose using ct in orthopaedic injury (REDUCTION) protocol effective? Bone Joint J. 2016;98B(12):1668–73.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Lei, M., Zhang, M., Li, H. et al. The diagnostic performance of ultra-low-dose 320-row detector CT with different reconstruction algorithms on limb joint fractures in the emergency department. Jpn J Radiol 40, 1079–1086 (2022). https://doi.org/10.1007/s11604-022-01290-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-022-01290-1