Abstract
Purpose
To test the tagging efficacy, patient acceptability, and accuracy of computed tomographic colonography (CTC) with a reduced dose of laxative using a novel barium sulfate (BaSO4) contrast agent.
Materials and methods
CTC followed by optical colonoscopy (OC) was performed on 73 patients with positive results in fecal occult blood tests. They were administrated a BaSO4 suspension and a magnesium citrate solution for bowel preparation. Patients completed a questionnaire about the acceptability of bowel preparation. Tagging efficacy was estimated using a novel categorization system, which classified all segments into 8 categories. The accuracy of detecting protruded lesions ≥ 6 mm was calculated from the comparison of CTC and OC results, using the latter as a reference standard.
Results
Tagging efficacy was good in 77.3% of colonic segments where residue was observed. The acceptability of bowel preparation for CTC was significantly higher than that for OC. The sensitivity, specificity, and positive and negative predictive values were 0.778, 0.945, 0.824, and 0.929, respectively. All lesions ≥ 7 mm were successfully detected by CTC.
Conclusion
CTC with a reduced dose of laxative using a novel BaSO4 contrast agent has a favorable tagging efficacy, patient acceptability, and accuracy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Computed tomographic (CT) colonography (CTC) has recently received considerable attention as a novel imaging technique for colorectal cancer (CRC). With the advancement of CT scanners and computer processing, CTC use has spread rapidly since its first report in 1994 [1]. CTC has become the key CRC screening tool based on the results of a large-scale national trial (ACRIN6664) in the United States [2], where per-patient sensitivities were reported to be 78% and 90% for lesions sized ≥ 6 mm and ≥ 10 mm, respectively, which are almost comparable to those of optical colonoscopy (OC). Some multicenter studies have reported detection rates for colorectal neoplastic lesions using CTC rather than OC [3,4,5,6,7].
Besides accuracy, patient acceptability determines the effectiveness of CTC. Full cathartic bowel preparation leaves few solid residues in the lower digestive tract, leading to a high diagnostic accuracy, but the heavy burden on the patient lowers the acceptability of CTC. In CRC screening, bowel preparation has been reported to be a significant factor affecting acceptability [8,9,10], with higher patient acceptancy being associated with higher participation rates. In CTC, fecal tagging with an oral contrast agent and bowel preparation with a reduced dose of laxative have been studied, and this bowel preparation is expected to reduce the burden on the patients while maintaining diagnostic accuracy. However, different from the situation in Europe and the United States, barium sulfate contrast agent for tagging had not been approved in Japan and it could not be used in daily clinical practice. Thus, a barium sulfate suspension was developed to be used as a tagging agent with approval in Japan. The present study reports the tagging efficacy and the accuracy of CTC with a reduced dose of laxative and using a novel barium sulfate tagging agent, developed to improve acceptability.
Materials and methods
Study design
Institutional review board approval was obtained for the study. Between March 2013 and May 2014, 78 participants aged 35–75 years who were scheduled to undergo OC due to a positive fecal occult blood test results at our institution were recruited. Of these, 3 withdrew from the study for personal reasons and 2 withdrew due to protocol violations. Finally, 73 patients were included in the study. All patients provided written informed consent before enrollment.
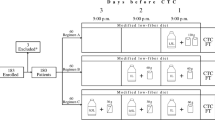
Bowel preparation
Patients had a low-fiber diet for breakfast, meals out of a package (FG-one; S&B Foods, Tokyo, Japan) for lunch and supper the day before the procedure, and for breakfast on the day of the procedure. They took BaSO4 contrast agent (8 g) in an aqueous suspension (25% w/v, 32 mL; ColomforT; Fushimi Pharmaceutical, Marugame, Japan) as a fecal tagging agent after every meal the day before the procedure. This novel formulation is easy to swallow and allows BaSO4 particles to be stably suspended in digestive fluid. Sennoside (Senevacul; Seiko-Eiyo Yakuhin, Osaka, Japan) 24 mg and magnesium citrate (Magcorol; Horii Pharmaceutical, Osaka, Japan) 34 g in an aqueous solution (180 mL) were orally administered to each patient at bedtime 2 days before the procedure and between 19:00 and 21:00 on the day before the procedure, respectively. Sodium picosulfate (Laxoberon; Teijin Pharma, Tokyo, Japan) 7.5–15 mg was administered at bedtime (Table 1).
Computed tomographic colonography study technique
A 64-row multi-slice CT (Aquilion 64; Toshiba, Tokyo, Japan) was performed using the following parameters: tube voltage, 120 kVp; X-ray tube current with automatic exposure control (AEC), SD30; slice thickness, 0.5 mm; beam pitch, 0.83; and reconstruction slice thickness, 0.5 mm. An anti-spasmodic drug, timepidium bromide 7.5 mg (Sesuden; Tanabeseiyaku Hanbai, Osaka, Japan) or glucagon 1 mg (G novo; Novo Nordisk Pharma, Tokyo, Japan) if the former was contraindicated, was injected intramuscularly before insufflation of the colon. An automated carbon dioxide insufflator (PROTOCO2L colon insufflator; Eidia, Tokyo, Japan) was used for colonic distension.
Interpretation of computed tomographic colonography
CTC readings were performed according to the indications of the central reading committee. Three diagnostic radiologists, members of the committee who were board-certified by the Japan Radiological Society and with experience in reading over 500 CTC cases, performed the CTC readings. They were blinded to OC results. Each radiologist independently interpreted all CT images using a workstation (Ziostation 2; Ziosoft, Tokyo, Japan) providing a simultaneous 3-dimensional (3D) endoluminal view and 2-dimensional (2D) multiplanar reconstruction (MPR) view (Fig. 1). Segment (cecum, ascending, transverse, descending, sigmoid, or rectum), location (distance from anus and xyz-coordinates), size, and macroscopic classification were recorded for each detected lesion. Lesion size was measured in the MPR view.
Three-dimensional (3D) simultaneous endoluminal view and 2-dimensional (2D) multiplanar reconstruction (MPR) view. Although it is difficult to distinguish the polyp from a residue using the 3D endoluminal view alone, the 3D endoluminal view (a) and the 2D MPR view (b) simultaneously enables recognition of the pedunculated structure as a residue due to its high attenuation
All readers independently interpreted all the images. Next, they evaluated the size of the lesion and determined the segment where it was detected. If 2 or 3 readers agreed on the identity of a detected lesion, the segment and average size of the majority were employed. If none agreed, adjacent segments were checked; if an unidentified lesion was detected there, the identity of these lesions was determined based on the segment, size, and macroscopic classification.
Assessment of tagging image quality
To evaluate the ability of the tagging agent in the differentiation of residues from surrounding tissues, a new categorization was designed specifically for this study: category 1 (residues/surrounding tissue differentiation, good; tagging status, homogeneous), 2 (good; heterogeneous), 3 (good; layered), 4 (poor; excessively tagged), 5 (poor; insufficiently tagged), 6 (poor; heterogeneous), 7 (poor; layered), and 8 (no residue) (Fig. 2). Differentiation was considered good regardless of heterogeneous (category 2) or layered (category 3) tagging status, as long as the tagging agent served its purpose, i.e., enabled readers to differentiate residues from the surrounding tissue.
Patient acceptability of bowel preparation
To compare patient acceptability of bowel preparations for CTC and OC, a patient self-reported questionnaire survey using the visual analog scale (VAS) was conducted [11], with scores ranging from 0 (no burden) to 100 (worst possible burden). We also assessed ease in swallowing the contrast agent (BaSO4) using the following 4 categories: category 1 (very easy), 2 (easy), 3 (difficult), and 4 (very difficult).
Optical colonoscopy
OC was conducted on the same day as the CTC, except for the one conducted 10 days after CTC. For both of the OC examinations, bowel preparation using 2 L of polyethylene glycol solution was used. A board-certified specialist of the Japan Gastroentrological Endoscopy Society blinded to the CTC results performed the OC. The specialist observed lesions while pulling an endoscope back, and recorded lesions sized ≥ 2 mm. Segment, distance from the anus, size, height, and macroscopic classification were recorded for each detected lesion. Its size and height were measured with a ruler attached to the endoscope. For lesions ≥ 6 mm, a dye (indigo carmine) was sprayed; if the lesion was suspected to be an advanced neoplasia or carcinoma, biopsy was performed for histopathological evaluation.
Lesion matching between computed tomographic colonography and optical colonoscopy
All lesions detected by both CTC and OC were mechanically matched. A lesion in the same segment and with a size measured by CTC 50–150% of that measured by OC was considered matched; otherwise, it was considered unmatched. All lesions detected by either CTC or OC alone were considered to be unmatched. After the mechanical matching, the 3 radiologists and the gastroenterologist reviewed the CTC data (2D and 3D views) and OC data (videos and still images) and arrived at a final conclusion.
Statistical analysis
Efficacy of tagging was defined as the ratio of well-differentiated segments (categories 1, 2, and 3) to the number of segments with residues, which was obtained by subtraction of the number of segments without residues (category 8) from the total number of segments. Tagging efficacy was calculated per segment and per reader. The inter-reader agreement of category was calculated as a ratio of the number of segments which 2 readers assigned the to the same category, compared to the total number of segments. The inter-reader agreement on efficacy was calculated in the same manner.
To evaluate patient acceptability for bowel preparation, a two-sided paired t test was conducted on log-transformed VAS values.
Diagnostic results for each patient were determined based on the results for each lesion for each patient. The per-lesion results were defined as follows: the presence of a lesion in both procedures (true positive), the presence of a lesion in the CTC only (false positive); and the presence of a lesion in the OC only (false negative). True negatives for a lesion cannot be defined, because the judgment cannot be carried out without a lesion to be judged. The per-patient results were defined as follows: for a patient with only 1 type of per-lesion result, the per-patient result was determined to be the same as the per-lesion result; otherwise, the per-patient result was determined to be a “true positive” when there was at least 1 true positive per-lesion result, as CTC would appropriately lead to necessary OC. When a patient had false positive and false negative per-lesion results, the per-patient result was determined to be “false positive,” because CTC would inappropriately lead to unnecessary OC. The remaining results were defined as true negative.
Based on the per-patient results, per-patient sensitivity, specificity, correct diagnostic rate, positive predictive value (PPV), negative predictive value (NPV), and 95% confidence interval (CI) for each parameter were calculated for lesions with height ≥ 2 mm (protruded) and size ≥ 6 mm. As secondary outcome measures, per-lesion sensitivity, the PPV, and the 95% CI were calculated for each lesion size.
Results
The baseline characteristics of 73 patients were as follows: 62 males; 11 females; mean age, 49.6 (35–70) years. No complications related to the procedures were observed. OC successfully reached the cecum and allowed observation of all segments for all patients.
In OC, 89 lesions were detected in 36 patients (49.3%, 36/73). Among these lesions, 59 protruded lesions were found in 30 patients (41.1%, 30/73), and of these patients, 26 lesions sized ≥ 6 mm were found in 18 patients (24.7%, 18/73). Of the latter, 16 and 2 lesions were histopathologically diagnosed as adenoma and carcinoma, respectively. Table 2 shows the classification of the 26 lesions endoscopically sized ≥ 6 mm following segment and macroscopic classification, respectively. They were observed more frequently in the sigmoid colon; sessile and pedunculated lesions predominated.
Tagging image quality
The mean tagging efficacy was 0.773 (95% CI = 0.730–0.816) (Table 3). Tagging efficacy by segment was lower in the cecum (0.630) and the ascending colon (0.683), but was higher in the transverse (0.871), descending (0.868), and sigmoid colons (0.852). Almost all cases with low efficacy resulted from heterogeneous and insufficient tagging, with the latter more frequently observed in the deep colon. Tagging efficacies for the three readers were 0.735, 0.745, 0.839, respectively (Table 3), while the inter-reader agreement for tagging evaluations for each pair of readers was 0.829, 0.845, and 0.845 (Table 4).
Patient acceptability of bowel preparation
The mean and standard deviation (mean ± SD) values of VAS were 49.7 ± 23.3 for OC and 33.2 ± 22.4 for CTC. The 95% CI of the log-transformed ratio of the VAS value for OC to that of CTC (log VASOC/VASCTC) was log 1.32 to log 2.47, with its antilogarithm exceeding 1, showing statistically significant difference (P = 0.0003). Thus, bowel preparation for CTC was more acceptable than that for OC.
The efficacy of the contrast agent (BaSO4) in improving the ease of swallowing was 0.986 (95% CI = 0.926–1.000), when the responses “very easy” and “easy” were regarded as indicators of efficacy. This indicates that administration of BaSO4 contrast agent was less burdensome.
Per-patient and per-lesion assessment
Table 5 shows the overall diagnostic accuracy of CTC for detecting at least 1 protruded lesion sized ≥ 6 mm. Per-patient sensitivity, specificity, correct diagnostic rate, PPVs and NPVs were 0.778 (95% CI = 0.524–0.936), 0.945 (0.849–0.989), 0.904 (0.837–0.972), 0.824 (0.566–0.962), and 0.929 (0.827–0.980), respectively. The sensitivity by lesion size threshold (PPV) was 0.808 (0.875), 1.00 (0.850), 1.00 (0.938), 1.00 (0.917), and 1.00 (0.917) for protruded lesions sized ≥ 6, ≥ 7, ≥ 8, ≥ 9, and ≥ 10 mm, respectively; thus, all protruded lesions sized ≥ 7 mm were detected by CTC (Table 6). Invasive carcinomas were detected in 2 patients (Fig. 3). There were 5 false-negative patients with 1 lesion each undetected by CTC but detected by OC: 3 lesions in the sigmoid, and 1 each in the transverse and descending colons. None of the lesions were found in poorly tagged segments. On macroscopic classification, 3 lesions were protruded sessile lesions and 2 were flat, protruded lesions. All lesions had relatively low tumor heights and were as small as 6 mm in diameter.
Early asymptomatic carcinoma detected in the rectum of a 70-year-old male. computed tomographic colonography image shows a sessile polyp with well-circumscribed depression (a). Endoscopic image confirms the presence and morphology of the 15-mm lesion, which contained a focus of invasive carcinoma at biopsy (b)
Discussion
Image quality in CTC has generally been evaluated based on parameters such as the size of residual stool and the amount of residual fluid in each segment, absorbance (CT values) of residual fluid and residual stool, and ratio of tagged residual stool to residual fluid [12, 13]. Herein, we assumed that the most important role of the tagging agent is the precise differentiation of residual stool and fluid from colonic structures like lesions and folds. Thus, we devised a novel method that considered tagging performance as effective, even when a small amount of residue was present or if the absorbance was somewhat low or heterogeneous, as long as precise differentiation was possible. Tagging efficacy was high in all colonic segments (77.3%); inter-reader agreement was above 80%, which was favorable. Hence, the tagging regimen used in this study is a useful bowel preparation for CTC and has high reproducibility.
As BaSO4 is insoluble, a potential concern may be heterogeneous tagging statuses such as “layering”, which is composed of tagged stool and/or fluid and weakly tagged supernatant fluid. Herein, layered areas were only 3.6%. Furthermore, almost no excessively tagged areas were detected (category 4). It is speculated that this regimen is appropriate to ensure that the colon is sufficiently dry to remove excess fluid, and yet wet enough to prevent excess concentration of BaSO4. The tagging efficacy of the right colon tended to be lower than other sites. In the proximal colon, residues are generally likely to remain, and it is thought that residues that are not tagged remain not excreted by laxatives.
A key issue in CRC screening is how to reduce the patient burden associated with bowel cleansing to improve acceptability [14]. Thus, CTC in combination with reduced laxative regimens or no laxative has been investigated [15,16,17,18,19]. However, in the case of not using any laxatives, to tag all residues remaining in the colon, it is necessary to take the contrast agent over multiple days according to the defecation cycle of the patient, so that the regimen would become cumbersome. In addition, because individual differences are large for bowel conditions, there is a possibility that performing bowel preparations without any laxatives could not guarantee the quality of the examination at present. Therefore, we examined bowel preparation with a small amount of laxative and the novel barium sulfate contrast agent. Taylor et al. also reported the usage of barium sulfate as a tagging agent for bowel preparations using 18 g of magnesium citrate and 13 g of senna [12]. In this study, we used 34 g of magnesium citrate and a small amount of senna, sodium picosulfate. Using CTC with the conditions mentioned above, OC with 2 L of polyethylene glycol solution was carried out in a short term, and then the patient’s acceptability was compared. Bowel preparation used for CTC had significantly higher patient acceptability than that used for OC. Furthermore, 98.6% of respondents reported that the BaSO4 contrast agent was easy to swallow. Meglumine diatrizoate is used widely as an oral contrast agent for fecal/fluid tagging in current CTC practice, but it has an unpleasant taste and may cause adverse effects such as nausea, diarrhea [20, 21], or abdominal cramps owing to its high osmolality and potential for allergic reactions [22, 23]. We believe that CTC with BaSO4, which is easy to swallow and has fewer adverse effects, can be valuable in increasing the screening rate for CRC.
In a meta-analysis of CTC diagnostic accuracy based on aggregate results of 6 CTC screening studies in asymptomatic patients, the per-patient sensitivities for detecting lesions sized ≥ 6 mm and ≥ 10 mm were 80% and 88%, respectively [2, 3, 24,25,26,27]. Similarly, in a study in which diagnostic accuracy and patient acceptability of bowel preparation for CTC were investigated with reduced laxative regimens using BaSO4 as a tagging agent, the per-patient sensitivity, specificity, PPV, and NPV for lesions sized ≥ 6 mm were 96%, 97%, 0.90, and 0.96, respectively [12]. A meta-analysis of CRC detection showed that the sensitivities of CTC, of CTC using laxative and tagging agents, and of OC were 96.1, 100.0, and 94.7%, respectively [28]. Herein, the per-patient sensitivities for protruded lesions sized ≥ 6 mm and ≥ 7 mm were 77.8% and 100%, respectively. The former is comparable to and the latter equivalent to or greater than previous results. CTC successfully detected all the 2 invasive carcinomas found by OC. Five lesions, 2 of which were adenomas, were found to be false negative; all were as small as 6 mm and had relatively low tumor heights compared to their diameters. There was no lesion sized ≥ 10 mm with false-negative result. As demonstrated in the ACRIN 6664 trial [2], in which the size of lesions to be detected was limited to ≥ 10 mm, CTC is useful for detecting adenoma and cancer. Similar conclusions may be drawn in this study.
This study has a few limitations. First, this study differs greatly in the amount of laxative used for bowel preparation the day before CTC, from the previous study by Taylor et al., who used BaSO4-based fecal tagging. We administered 34 g of magnesium citrate, according to its indication for a hyperosmolar solution, and administered sodium picosulfate solution orally at bedtime. Further studies are required to elucidate the relationship between bowel preparation regimens and colonic conditions. Second, we did not conduct histopathological evaluation for any lesion sized ≥ 6 mm detected by OC. Colonoscopists can determine empirically the clinical significance of a lesion based on its size, morphology, color, and surface structure, after the application of spraying dye [29, 30]. In this study, all lesions sized ≥ 6 mm were sprayed with a dye and then carefully inspected with OC. For lesions suspected to be hyperplastic polyps, biopsy was not performed to avoid the risk of bleeding.
In conclusion, bowel preparation using a combination of a reduced dose of laxative and a novel 25% BaSO4 contrast agent has favorable tagging efficacy, reproducibility, and patient acceptability. Furthermore, the diagnostic accuracy of CTC with this regimen for detecting protruded lesions sized ≥ 6 mm was as high as that of OC.
References
Vining DJ, Gelfand DW, Bechtold RE, Scharling ES, Grishaw EK, Shifrin RY. Technical feasibility of colon imaging with helical CT and virtual reality. AJR Am J Roentgenol. 1994;162:S104.
Johnson CD, Chen MH, Toledano AY, Heiken JP, Dachman A, Kuo MD, et al. Accuracy of CT colonography for detection of large adenomas and cancers. N Engl J Med. 2008;359:1207–17.
Pickhardt PJ, Choi JR, Hwang I, Butler MD, Puckett ML, Hildebrandt HA, et al. Computed tomographic virtual colonoscopy to screen for colorectal neoplasia in asymptomatic adults. N Engl J Med. 2003;349:2191–200.
Cotton PB, Durkalski VL, Pineau BC, Palcsch YY, Mauldin PD, Hoffman B, et al. Computed tomographic colonography (virtual colonoscopy): a multicenter comparison with standard colonoscopy for detection of colorectal neoplasia. JAMA. 2004;291:1713–9.
Rockey DC, Paulson E, Niedzwiecki D, Davis W, Bosworth HB, Sanders L, et al. Analysis of air contrast barium enema, computed tomographic colonography, and colonoscopy: prospective comparison. Lancet. 2005;365:305–11.
Liedenbaum MH, van Rijn AF, de Vries AH, Dekker MH, Thomeer M, van Marrewijk CJ, et al. Using CT colonography as a triage technique after a positive faecal occult blood test in colorectal cancer screening. Gut. 2009;58:1242–9.
Regge D, Laudi C, Galatola G, Monica PD, Bonelli L, Angelelli G, et al. Diagnostic accuracy of computed tomographic colonography for the detection of advanced neoplasia in individuals at increased risk of colorectal cancer. JAMA. 2009;301:2453–61.
Harewood GC, Wiersema MJ, Melton LJ 3rd. A prospective, controlled assessment of factors influencing acceptance of screening colonoscopy. Am J Gastroenterol. 2002;97:3186–94.
Ristvedt SL, McFarland EG, Weinstock LB, Thyssen EP. Patient preferences for CT colonography, conventional colonoscopy, and bowel preparation. Am J Gastroenterol. 2003;98:578–85.
Zalis ME, Perumpillichira JJ, Magee C, Kohlberg G, Hahn PF. Tagging-based, electronically cleansed CT colonography: evaluation of patient comfort and image readability. Radiology. 2006;239:149–59.
Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health. 1990;13:227–36.
Taylor SA, Slater A, Burling DN, Tam E, Greenhalgh R, Gartner L, et al. CT colonography: optimisation, diagnostic performance and patient acceptability of reduced-laxative regimens using barium-based faecal tagging. Eur Radiol. 2008;18:32–42.
Fletcher JG, Silva AC, Fidler JL, Cernigliaro JG, Manduca A, Limburg PJ, et al. Noncathartic CT colonography: image quality assessment and performance and in a screening cohort. AJR Am J Roentgenol. 2013;201:787–94.
Weitzman ER, Zapka J, Estabrook B, Goins KV. Risk and reluctance: understanding impediments to colorectal cancer screening. Prev Med. 2001;32:502–13.
Lefere P, Gryspeerdt S, Marrannes J, Baekelandt M, Van Holsbeeck B. CT colonography after fecal tagging with a reduced cathartic cleansing and a reduced volume of barium. AJR Am J Roentgenol. 2005;184:1836–42.
Liedenbaum MH, de Vries AH, Gouw CIBF, van Rijn AF, Bipat S, Dekker E, et al. CT colonography with minimal bowel preparation: evaluation of tagging quality, patient acceptance and diagnostic accuracy in two iodine-based preparation schemes. Eur Radiol. 2010;20:367–76.
Stoop EM, de Haan MC, de Wijkerslooth TR, Bossuyt PM, van Ballegooijen M, van de Vijver MJ, et al. Participation and yield of colonoscopy versus non-cathartic CT colonography in population-based screening for colorectal cancer: a randomised controlled trial. Lancet Oncol. 2012;13:55–64.
Zalis ME, Blake MA, Cai W, Hahn PF, Halpem EF, Kazam IG, et al. Diagnostic accuracy of laxative-free computed tomographic colonography for detection of adenomatous polyps in asymptomatic adults—a prospective evaluation. Ann Intern Med. 2012;156:692–702.
Iafrate F, Iannitti M, Ciolina M, Baldassari P, Pichi A, Laghi A. Bowel cleansing before CT colonography: comparison between two minimal-preparation regimens. Eur Radiol. 2015;25:203–10.
Iannaccone R, Laghi A, Catalano C, Mangiapane F, Lamazza A, Schillaci A, et al. Computed tomographic colonography without cathartic preparation for the detection of colorectal polyps. Gastroenterology. 2004;127:1300–11.
Jensch S, Bipat S, Peringa J, de Vries AH, Heutinck A, Dekker E, et al. CT colonography with limited bowel preparation: prospective assessment of patient experience and preference in comparison to optical colonoscopy with cathartic bowel preparation. Eur Radiol. 2010;20:146–56.
Skucas J. Anaphylactoid reactions with gastrointestinal contrast media. AJR Am J Roentgenol. 1997;168:962–4.
Davis PL. Anaphylactoid reactions to the nonvascular administration of water-soluble iodinated contrast media. AJR Am J Roentgenol. 2015;204:1140–5.
De Haan MC, van Gelder RE, Graser A, Bipat S, Stoker J. Diagnostic value of CT-colonography as compared to colonoscopy in an asymptomatic screening population: a meta-analysis. Eur Radiol. 2011;21:1747–63.
Graser A, Stieber P, Nagel D, Schäfer C, Horst D, Becker CR, et al. Comparison of CT colonography, colonoscopy, sigmoidoscopy and faecal occult blood tests for the detection of advanced adenoma in an average risk population. Gut. 2009;58:241–8.
Kim YS, Kim N, Kim SH, Park MJ, Lim SH, Yim JY, et al. The efficacy of intravenous contrast-enhanced 16-raw multidetector CT colonography for detecting patients with colorectal polyps in an asymptomatic population in Korea. J Clin Gastroenterol. 2008;42:791–8.
Macari M, Bini EJ, Jacobs SL, Nalk S, Lui YW, Milano A, et al. Colorectal polyps and cancers in asymptomatic average-risk patients: evaluation with CT colonography. Radiology. 2004;230:629–36.
Pickhardt PJ, Hassan C, Halligan S, Marmo R. Colorectal Cancer: CT colonography and colonoscopy for detection—systematic review and meta-analysis. Radiology. 2011;259:393–405.
Axelrad AM, Fleischer DE, Geller AJ, Nguyen CC, Lewis JH, Al-Kawas FH, et al. High-resolution chromoendoscopy for the diagnosis of diminutive colon polyps: implications for colon cancer screening. Gastroenterology. 1996;110:1253–8.
Apel D, Jakobs R, Schilling D, Weickert U, Teichmann J, Bohrer MH, et al. Accuracy of high-resolution chromoendoscopy in prediction of histologic findings in diminutive lesions of the rectosigmoid. Gastrointest Endosc. 2006;63:824–8.
Acknowledgements
The scientific guarantor of this publication is K. Mitsuzaki, MD, PhD. This study was funded by Fushimi Pharmaceutical Co., Ltd. for the approval of a pharmaceutical product, and conducted in compliance with GCP (ICH-G6). Akira Yoshino of Fushimi Pharmaceutical Co., Ltd. conducted the statistical analysis.
Funding
This study was funded by Fushimi Pharmaceutical Co., Ltd. for the approval of a pharmaceutical product, and conducted in compliance with GCP (ICH-G6).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors of this manuscript declare no relationship with any companies.
Research ethics and patient consent
Saiseikai Kumamoto Hospital Institutional Review Board approved this study (CTC-2310/P301). Written informed consent was obtained from all patients in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Mitsuzaki, K., Iinuma, G., Morimoto, T. et al. Computed tomographic colonography with a reduced dose of laxative using a novel barium sulfate contrast agent in Japan. Jpn J Radiol 37, 245–254 (2019). https://doi.org/10.1007/s11604-018-0800-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-018-0800-x