Abstract
Purpose
This study aimed to assess the feasibility and patient tolerance of a 2-day limited fecal tag bowel preparation in computed tomographic colonography (CTC) performed for incomplete conventional colonoscopy (CC) patients.
Materials and methods
Seventy-five patients who underwent a CTC examination fbecause of incomplete CC were included. A low-residue diet was given for 2 days before CTC. Fecal tagging (FT) was done using a barium sulfate suspension. The quality of the preparation, success of tagging and patient experience with the bowel preparation were investigated.
Results
Four hundred fifty bowel segments were evaluated. The number of solid stool balls of 6–9 mm size was 284; the corresponding figure was 93 for solid stool balls ≥10 mm. Residual fluid was present in about one-third of the segments. The fecal tagging efficacy for ≥6 mm residual stool balls was 92 %. Overall, 16 (21.3 %) patients presented with colonic lesions at CTC. Three out of four colonic mass lesions had not been diagnosed with CC. Most patients reported mild discomfort.
Conclusion
FT-CTC performed after a limited 2-day bowel preparation seems to be a technically feasible, safe and acceptable procedure that allows a complete a colonic study in incomplete CC patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) represents the third most common malignancy worldwide and is the second most common cause of cancer-related deaths in the USA [1]. Although conventional colonoscopy (CC) is the gold standard method for evaluating the colon [2, 3], incomplete examinations failing to reach the level of the cecum comprise 6–26 % of all colonoscopies [4–6] and have been reported to occur in up to 40 % of the very elderly undergoing CC [7]. Causes of incomplete colonoscopy include procedure intolerance, poor bowel preparation, tortuous colonic segments and colonic disease, such as stenosis or obstruction caused by colonic cancer or diverticular disease [8, 9]. Moreover, the risk of complications, mainly electrolyte imbalance, appears to impair the safety profile of bowel preparation for CC [10].
Computed tomographic colonography (CTC) is a noninvasive imaging modality that offers certain advantages over conventional colonoscopy such as rapid data acquisition and minimal patient discomfort [5, 11, 12]. Previous studies of CTC yielded a sensitivity of up to 90 % in the diagnosis of polyps ≥10 mm in size [13–16]. The American Gastroenterological Society recognizes CTC as the imaging modality of choice for cases of incomplete CC [17]. CTC is generally well tolerated by patients [18, 19], although bowel preparation still remains a challenge [19]. Most previous studies used high-dose cathartics to obtain better vision, which potentially impairs patient satisfaction and comfort [20–22].
The use of fecal tagging (FT) before CTC has proven effective in combination with a reduced cathartic cleansing [23]. Currently, non-ionic contrast agents with a small allergic risk and a relatively high cost are used for this purpose. Barium on the other hand is a cheap and well-tolerated fecal-tag agent with almost no allergic potential, representing an alternative to nonionic agents. However, the success of the FT-CTC technique still depends on the quality of the bowel preparation.
We hypothesized that using a less cathartic regimen consisting of a low-fiber diet, bisacodyl and senna but extending the duration of bowel preparation, along with fecal tagging using an agent with a good tolerability profile (barium), would help improve patient comfort and imaging quality. Thus, this study assessed the feasibility and patient tolerance of a 2-day limited fecal-tag bowel preparation in CTC performed for incomplete colonoscopy patients.
Materials and methods
Patients
Seventy-five patients (mean age 58 years, range: 46–84) who underwent a CTC examination between April 2011 and March 2013 were included in this single-center prospective study. Patients had undergone colonoscopy previously, and the procedure was incomplete in all of them. Thirty-three patients were female (44 %) and 42 were male (56 %). The reasons for referral to CTC included incomplete CC due to poor colonic preparation and residual colonic content (n = 28), patient intolerance during CC examination (n = 22), colonic tortuosity (n = 13), sigmoid diverticular disease (n = 10) and adhesions (n = 2). CTC was performed within 2 weeks after incomplete colonoscopy, with a mean interval of 10 days. The study protocol was approved by local ethics committee and conducted in accordance with Declaration of Helsinki. All participants provided written informed consent prior to study entry.
Bowel preparation
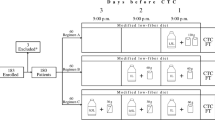
All patients followed a low-residue diet for 2 days before CTC, during which they were instructed to completely avoid consuming fiber-rich food, including fruits, vegetables, whole-grain bread and whole-grain cereals. On the day prior to CTC, only a liquid diet was allowed, which consisted of only clear and opaque liquid foods with a smooth consistency.
Fecal tagging was done using a 225-ml barium sulfate suspension (E.Z.CAT barium sulfate suspension, Opakim Medical Products Inc., E-Z-EM Canada Inc.) diluted with 500 ml of water or fruit juice (2.1 % w/v barium sulfate). The suspension was divided into three equal portions to be taken 15 min after breakfast, lunch and dinner on day 2. In addition, Bekunis tablets (Abdi Ibrahim, Turkey), containing bisacodyl (5 mg) and sennoside B (3 mg) as active ingredients with stool softening properties were used for bowel preparation. All patients were instructed to take two tablets at 7:00 PM on the 1st and 2nd day of their preparation diet (i.e., a total of 4 tablets were taken). In the morning before the procedure, no breakfast was allowed. CTC was performed between 8:30 and 9:30 AM.
CT colonography technique
All CTC examinations were performed using a 64-row scanner (Toshiba Aquillion TSX-101A, Japan) with a 64 × 0.5-mm detector collimation at 120 kV and 100 mAs (0.8 pitch and 0.5 s gantry rotation). In the left lateral decubitus position, the colon was gently insufflated with room air by a radiologist using a lubricated foley catheter placed in the rectum until the patient requested that air insufflation be discontinued or distention was believed to be adequate (30–50 bulb compressions). Colonic distention was assessed on the scout view. In the event of insufficient colonic distention, additional insufflation was performed. In the event of good colonic distention, the patient underwent scanning while supine with the tube still in the rectum. The patient was subsequently turned to the prone position. If necessary, additional inflation of the colon was performed. If the patient was not able to lie in prone position, the patient was scanned in the left decubitus position. To avoid concealment of rectal polyps by the rectal tube, the tube was removed at this time. To reduce radiation exposure, patients were scanned at a reduced dose of 50 mAs when acquiring the images in the prone position. CT images were reconstructed with 5-mm slice thickness at 0.5 mm intervals. The whole abdomen from the diaphragm to the symphysis pubis was scanned in a single breath-hold over an average of 8 s.
CTC image analysis and grading the quality of bowel preparation
The CT data sets were post-processed using commercially available software (Aquarius iStation, TeraRecon, Fostr City, CA, USA). Two radiologists independently analyzed each patient directly on a dedicated workstation, and disagreements were solved by consensus. Both radiologists were experienced in the procedure. K.M and N.B had performed more than 200 and 100 colonographies, respectively. The quality of the preparation and success of tagging was also retrospectively evaluated by the same study team members using a modified grading system originally proposed by Lefere et al. and Taylor et al. [20, 21]. The colon was evaluated per patient and per segment. For the purposes of the analysis, the colon was divided into six segments: the cecum, ascending, transverse, descending and sigmoid colon, and rectum.
Residual solid stool was categorized and scored as follows: 1, no stool; 2, small stool (≤6 mm); 3, moderate-size stool (6–9 mm); 4, large stool (≥10 mm) [24]. Scoring was based on 2D measurements using electronic calipers, and the presence of residual solid stool in colonic segments was evaluated. In segments with different solid stool sizes, only the largest solid stool size was considered.
Residual fluid grading was based on the maximum anterior-posterior (AP) diameter of the colonic lumen that was submerged. For each colonic segment, scores were as follows: 1, no fluid; 2, <25 % of the AP diameter; 3, 25–50 % of the AP diameter; 4, >50 % of AP diameter [21]. In segments with different fluid levels, only the largest fluid level was considered.
Residual tagged solid stool scores were assigned as follows: 1, all residual solid stool untagged; 2, 1 to <25 % tagged; 3, 25 to <50 % tagged; 4, 50 to <75 % tagged; 5, 75–100 % tagged [21]. The tagged appearance of residual fluid was assessed on a visual basis: tagged or non-tagged [20].
All pathologic findings within the colon were documented including all colonic masses (≥30 mm) and large (10–29 mm) and medium-sized (6–9 mm) polyps. The classification of the detected colonic polyps, mass lesions and extracolonic incidental findings was based on the CT Colonography Reporting and Data System (C-RADS) [25]. When a suspected polypoid lesion was detected, coronal, sagittal and oblique multiplanar reconstructions as well as 3D images were analyzed to confirm the lesion and to increase the diagnostic yield. The maximum diameter of all polyps was measured using an electronic ruler on the 2D images.
Patient tolerance
To evaluate patient tolerance to the preparation, all patients were asked to fill a questionnaire the morning before CTC that gathered information on global discomfort and side effects (headache, nausea, vomiting, abdominal cramps and diarrhea) associated with the limited bowel preparation. Global discomfort was rated as follows: 0, none; 1, mild; 2, moderate; 3, severe. After CTC, a second questionnaire was administered that posed the following question: “Which of these two examinations would you prefer if you were to have it again in the future: CC or CTC.”
Results
Evaluation of bowel preparation
A total of 450 bowel segments were evaluated. Table 1 shows the distributions of residual solid stool, residual fluid and tagging quality across these segments. The number of solid stool balls of 6–9 mm size was 284; the corresponding figure was 93 for solid stool balls ≥10 mm. Residual fluid was present in about one-third of the segments. When only segments with residual stool were considered (n = 294), in only 17 of them was stool untagged (5.8 %). The fecal tagging efficacy for ≥6 mm residual stool balls was 92 %. Non-tagged fluid was detected in 10.2 % (15/147) of segments. None of the non-tagged fluid segments covered more than 50 % of the colonic segments. Overall, the tagging percentage of residual fluid in colonic segments was 89.8 % (132/147). Figure 1 shows mean scores for residual solid stool, residual fluid and tagging quality for the entire colon.
Colonic and extracolonic findings
Overall, 16 (21.3 %) patients presented with colonic lesions at CTC. Colonic lesions included four colonic masses (C-RADS category C4), three colonic polyps >10 mm (C-RADS category C3), and nine colonic polyps between 6 and 9 mm (C-RADS category C2). Colonic mass lesions were located in the following locations: two in the sigmoid colon (Fig. 2), one in the descending colon and one in the cecum. Three out of four colonic mass lesions had not been diagnosed with CC. All patients with colonic mass lesions underwent surgery (one case underwent right hemicolectomy and three had left hemicolectomy) and were confirmed to be adenocarcinomas. Two of the three polypoid lesions larger than 10 mm were pedunculated polyps (Fig. 3), and one was a sessile polyp. All colonic polyps larger than 10 mm were confirmed by successive colonoscopies and successfully resected. Two out of three polyps were tubulo-villous adenomas with a high grade of dysplasia upon pathological diagnosis; the remaining polyp was adenocarcinoma. Among the nine 6–9 mm polypoid lesions, two were pedunculated polyps and seven were sessile polyps. Six of nine colonic polyps between 6 and 9 mm underwent CC; five were confirmed and resected by CC, but one 6-mm polyp was not confirmed. Three out of five polyps were tubulo-villous adenoma with low-moderate grade dysplasia at pathological diagnosis; the remaining two were hyperplastic polyps. Diverticular disease was detected in 24 (32 %) patients. To the best of our knowledge based on the medical records of our hospital, none of the negative cases developed into colorectal cancer.
A 67-year-old male with a positive fecal occult blood test and anemia underwent incomplete conventional colonoscopy of the sigmoid because of patient intolerance. a Axial CT scan showing a neoplastic mass (arrow), narrowing the lumen of the sigmoid colon. Enlarged lymph nodes (black arrow) were present. b Three-dimensional threshold-rendered endoluminal CT colonography shows a similar endoscopic appearance of the mass. c Optical colonoscopy image of the neoplastic mass
A 56-year-old female who had an incomplete conventional colonoscopy of the transverse colon because of patient intolerance. a Axial image shows a pedunculated polypoid lesion (arrow) of the ascending colon vegetating within the colonic lumen. Histopathological examination confirmed tubulo-villous adenoma with low-grade dysplasia. b A 3D threshold-rendered endoluminal CT colonography of the ascending colon shows a 15-mm polypoid pedunculated lesion (arrow). c Optical colonoscopy image for polyp
Eighty-nine extracolonic findings were detected with CTC (Table 2). Of these, 7 (7.9 %) were categorized as having high clinical importance (C-RADS category E4), 27 (30.3 %) as having moderate clinical importance (C-RADS category E3) and the remaining 55 (61.8 %) as having low clinical importance (C-RADS category E2). C-RADS category E4 lesions were as follows: pericolonic and parailiac lymph nodes (n = 5) and pulmonary nodules >1 cm (n = 2).
Patient satisfaction
Seventy-five patients completed the questionnaire. Among them, 28 (37.3 %) reported symptoms, the most common being diarrhea (n = 16; 21.4 %) followed by abdominal cramps (n = 5; 6.6 %), headache (n = 5; 6.6 %) and nausea (n = 2; 2.7 %). No major complication was observed during the CTC examination. Fifty-three of the 75 patients (70.6 %) reported mild discomfort, and 22 (29.4 %) reported moderate discomfort (Table 3). None of the patients reported severe discomfort (Table 3). A majority of the patients in the study (69/75, 92 %) stated that they would prefer FT-CTC to CC if they need to have this procedure in the future.
Discussion
The findings of this study show that an FT-CTC using a 2-day limited bowel preparation appears to be feasible and safe in patients with a previous failure in CC. In addition, this 2-day limited bowel preparation of FT-CTC allows accurate visualization of the colon while at the same time avoiding the risks associated with a full cathartic preparation.
Incomplete visualization of the colon with CC is a relatively common occurrence in clinical practice. In a study by Gollub et al. [8], redundant/tortuous colon, patient intolerance and angulation of the colonic loops emerged as the most common causes of incomplete CC, while in a more recent study by Neerincx et al. [26] looping of the scope, patient discomfort and obstructive tumors were identified as the most frequent causes. However, although patient discomfort was also a common reason for incomplete CC in our participants as in other studies, poor preparation/residual colonic content represented the foremost cause of CC failure necessitating CTC among our patient group.
In this study, a markedly reduced cathartic regimen with bisacodyl and senna was used for bowel preparation. The amount of residual solid stool detected by CTC was higher than that reported by previous studies where higher doses of cathartics were used [20, 21]. On the other hand, the amount of residual fluid was lower as compared to previous reports. Given the markedly reduced cathartic regimen, the former observation was an expected outcome. However, the latter finding was quite unexpected. Both cathartics used in this study, i.e., bisacodyl and senna, induce peristalsis through local parasympathetic effects, and this mechanism of action may explain the reduction in residual colonic fluid volume.
In limited bowel preparations, adequate tagging of residual contents becomes increasingly more important when one considers the fact that more fecal residual is expected under these circumstances. In the present study, a barium sulfate suspension was used as a tagging agent, which is well tolerated and carries no risk of allergic reactions [20, 21, 27]. The first ESGAR consensus statement on CTC suggested that polyps less than 5 mm should not be reported in asymptomatic screening examinations. For the symptomatic patients, a reasonable minimum size for polyps to be reported is 5 or 6 mm [28]. Therefore, we assessed the tagging quality for residual stool balls ≥6 mm and found a tagging efficacy of 92 %, which is comparable with previous studies [20, 21]. In addition, the tagging of residual fluid was also good in our study. Non-tagged fluid was mostly negligible. None of the non-tagged fluid segments covered more than 50 % of the colonic segments.
The importance of completing a colonic study cannot be overemphasized. In our study, the detection rate of colorectal cancer that was previously missed by an incomplete CC was 4 % for FT-CTC performed with a 2-day limited bowel preparation. The corresponding figure in the study by Iafrate et al. [22] was 3 %. In this regard, it is important to remember that the results of previous studies have clearly established the diagnostic role of CTC in patients with incomplete CC [29, 30].
CTC also detected the presence of a large polyp in 4 % of the patients in our study. CTC was previously shown to have a diagnostic sensitivity of up to 90 % for polyps of 10 mm or greater [13–15]. It is a well-known fact that a substantial proportion of polyps greater than 1 cm represent cancerous growths [31, 32]. Despite this, only one large polyp was subsequently diagnosed as adenocarcinoma. In addition, nine colonic polyps between 6 and 9 mm were detected, and a subsequent CC was performed for six of them, five of which were confirmed.
Extracolonic findings were reported in 19.8 % of patients (n = 89) in this study. In seven patients, these were deemed clinically significant (C-RADS category E4) [25]. In terms of E4 results, our study is comparable to previous reports [22, 33].
The responses to the questionnaires used for the assessment of patient tolerance showed that the limited bowel preparation regimens utilized in our study were well accepted by the patients. Accordingly, 92 % of the patients stated that they would prefer FT-CTC to CC if they were to have a similar examination in the future. Taylor et al. [21] studied the fecal tagging using four different diet regimens and reported lower patient tolerance than our study. We believe that the lower doses of cathartics used in our study might explain the variance between the results with regard to patient tolerance. To assess patient tolerance without a cathartic agent, Iafrate et al. [22] used diatrizoate meglumine and diatrizoate sodium as the FT agent for bowel preparation. These authors reported that 77 % of the patients would be willing to repeat the test if necessary, again indicating somewhat lower tolerance than in our study. Therefore, our results suggest that a markedly reduced cathartic preparation with barium sulfate as an FT agent is a reasonable approach, particularly in patients with poor tolerance to CC bowel preparations.
Several limitations of this study should be mentioned. First, the sensitivity and specificity of the FT technique for detection of polyps could not be evaluated in this study, since our patient group consisted of incomplete CC patients who were not able to undergo the gold standard CC as to enable a comparison. In addition, patient tolerance was markedly higher than in previous reports, requiring some explanation. This could be partly attributed to the fact that our patients were referred to CTC after an incomplete CC, which could have been associated with certain adverse psychological/physical effects. Another limitation relates to the use of manual room air insufflation in our study. Many authors now advocate carbon dioxide administered via an automated pump to achieve colonic distention and also to allow faster absorption to reduce patient discomfort after CTC [34, 35]. However, others such as Shinners et al. observed no significant overall colonic distention advantage with either gas [34]. Finally, absence of follow-up questionnaire assessments after discharge (e.g., at 2 or 4 weeks post-discharge) may be considered to be another shortcoming regarding the evaluation of patients’ tolerance levels.
In conclusion, our study shows that FT-CTC performed after a limited 2-day bowel preparation is a technically feasible and safe procedure that allows a complete a colonic study in incomplete CC patients. Positive acceptance from the patients without compromising the detection rate of colorectal cancer and colonic polyps of >1 cm suggests that it may be a viable option in clinical practice.
References
Espey DK, Wu XC, Swan J, Wiggins C, Jim MA, Ward E, et al. Annual report to the nation on the status of cancer, 1975–2004, featuring cancer in American Indians and Alaska Natives. Cancer. 2007;110:2119–52.
Smith RA, Cokkinides V, von Eschenbach AC, Levin B, Cohen C, Runowicz CD, et al. American Cancer Society guidelines for the early detection of cancer. CA Cancer J Clin. 2002;52:8–22.
Ransohoff DF, Sandler RS. Clinical practice. Screening for colorectal cancer. N Engl J Med. 2002;346:40–4.
Schrock TR. Colonoscopy for colorectal cancer: too much, too little, just right. ASGE distinguished lecture 1993. Gastrointest Endosc. 1993;39:848–51.
Yucel C, Lev-Toaff AS, Moussa N, Durrani H. CT colonography for incomplete or contraindicated optical colonoscopy in older patients. AJR Am J Roentgenol. 2008;190:145–50.
Kim JH, Kim WH, Kim TI, Kim NK, Lee KY, Kim MJ, et al. Incomplete colonoscopy in patients with occlusive colorectal cancer: usefulness of CT colonography according to tumor location. Yonsei Med J. 2007;48:934–41.
Schmilovitz-Weiss H, Weiss A, Boaz M, Levin I, Chervinski A, Shemesh E. Predictors of failed colonoscopy in nonagenarians: a single-center experience. J Clin Gastroenterol. 2007;41:388–93.
Gollub MJ, Flaherty F. Barium enema following incomplete colonoscopy. Clin Imaging. 1999;23:367–74.
Mitchell RM, McCallion K, Gardiner KR, Watson RG, Collins JS. Successful colonoscopy; completion rates and reasons for incompletion. Ulster Med J. 2002;71:34–7.
Wexner SD, Beck DE, Baron TH, Fanelli RD, Hyman N, Shen B, et al. A consensus document on bowel preparation before colonoscopy: prepared by a task force from the American Society of Colon and Rectal Surgeons (ASCRS), the American Society for Gastrointestinal Endoscopy (ASGE), and the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES). Dis Colon Rectum. 2006;49:792–809.
Macari M, Berman P, Dicker M, Milano A, Megibow AJ. Usefulness of CT colonography in patients with incomplete colonoscopy. AJR Am J Roentgenol. 1999;173:561–4.
Stracci F, Zorzi M, Grazzini G. Colorectal cancer screening: tests, strategies, and perspectives. Front Public Health. 2014;2:210.
Pickhardt PJ. Virtual colonoscopy for primary screening. The future is now. Minerva Chir. 2005;60:139–50.
Fenlon HM, Nunes DP, Schroy PC 3rd, Barish MA, Clarke PD, Ferrucci JT. A comparison of virtual and conventional colonoscopy for the detection of colorectal polyps. N Engl J Med. 1999;341:1496–503.
Yee J, Akerkar GA, Hung RK, Steinauer-Gebauer AM, Wall SD, McQuaid KR. Colorectal neoplasia: performance characteristics of CT colonography for detection in 300 patients. Radiology. 2001;219:685–92.
Bouzas Sierra R. Optical colonoscopy and virtual colonoscopy: the current role of each technique. Radiologia. 2015;57:95–100.
Rex DK, Lieberman D. Acg. ACG colorectal cancer prevention action plan: update on CT-colonography. Am J Gastroenterol. 2006;101:1410–3.
Taylor SA, Halligan S, Saunders BP, Bassett P, Vance M, Bartram CI. Acceptance by patients of multidetector CT colonography compared with barium enema examinations, flexible sigmoidoscopy, and colonoscopy. AJR Am J Roentgenol. 2003;181:913–21.
van Gelder RE, Birnie E, Florie J, Schutter MP, Bartelsman JF, Snel P, et al. CT colonography and colonoscopy: assessment of patient preference in a 5-week follow-up study. Radiology. 2004;233:328–37.
Lefere P, Gryspeerdt S, Marrannes J, Baekelandt M, Van Holsbeeck B. CT colonography after fecal tagging with a reduced cathartic cleansing and a reduced volume of barium. AJR Am J Roentgenol. 2005;184:1836–42.
Taylor SA, Slater A, Burling DN, Tam E, Greenhalgh R, Gartner L, et al. CT colonography: optimisation, diagnostic performance and patient acceptability of reduced-laxative regimens using barium-based faecal tagging. Eur Radiol. 2008;18:32–42.
Iafrate F, Hassan C, Zullo A, Stagnitti A, Ferrari R, Spagnuolo A, et al. CT colonography with reduced bowel preparation after incomplete colonoscopy in the elderly. Eur Radiol. 2008;18:1385–95.
Lefere PA, Gryspeerdt SS, Dewyspelaere J, Baekelandt M, Van Holsbeeck BG. Dietary fecal tagging as a cleansing method before CT colonography: initial results polyp detection and patient acceptance. Radiology. 2002;224:393–403.
Nagata K, Singh AK, Sangwaiya MJ, Nappi J, Zalis ME, Cai W, et al. Comparative evaluation of the fecal-tagging quality in CT colonography: barium vs. iodinated oral contrast agent. Acad Radiol. 2009;16:1393–9.
Zalis ME, Barish MA, Choi JR, Dachman AH, Fenlon HM, Ferrucci JT, et al. CT colonography reporting and data system: a consensus proposal. Radiology. 2005;236:3–9.
Neerincx M, Terhaar sive Droste JS, Mulder CJ, Rakers M, Bartelsman JF, Loffeld RJ, et al. Colonic work-up after incomplete colonoscopy: significant new findings during follow-up. Endoscopy. 2010;42:730–5.
Neri E, Lefere P, Gryspeerdt S, Bemi P, Mantarro A, Bartolozzi C. Bowel preparation for CT colonography. Eur J Radiol. 2013;82:1137–43.
Taylor SA, Laghi A, Lefere P, Halligan S, Stoker J. European Society of Gastrointestinal and Abdominal Radiology (ESGAR): consensus statement on CT colonography. Eur Radiol. 2007;17:575–9.
Gryspeerdt S, Lefere P, Herman M, Deman R, Rutgeerts L, Ghillebert G, et al. CT colonography with fecal tagging after incomplete colonoscopy. Eur Radiol. 2005;15:1192–202.
Copel L, Sosna J, Kruskal JB, Raptopoulos V, Farrell RJ, Morrin MM. CT colonography in 546 patients with incomplete colonoscopy. Radiology. 2007;244:471–8.
Gschwantler M, Kriwanek S, Langner E, Goritzer B, Schrutka-Kolbl C, Brownstone E, et al. High-grade dysplasia and invasive carcinoma in colorectal adenomas: a multivariate analysis of the impact of adenoma and patient characteristics. Eur J Gastroenterol Hepatol. 2002;14:183–8.
Church JM. Clinical significance of small colorectal polyps. Dis Colon Rectum. 2004;47:481–5.
Keeling AN, Slattery MM, Leong S, McCarthy E, Susanto M, Lee MJ, et al. Limited-preparation CT colonography in frail elderly patients: a feasibility study. AJR Am J Roentgenol. 2010;194:1279–87.
Shinners TJ, Pickhardt PJ, Taylor AJ, Jones DA, Olsen CH. Patient-controlled room air insufflation versus automated carbon dioxide delivery for CT colonography. AJR Am J Roentgenol. 2006;186:1491–6.
Kanazawa H, Utano K, Kijima S, Sasaki T, Miyakura Y, Horie H, et al. A comparative study of degree of colorectal distention with manual air insufflation or automated CO(2) insufflation at CT colonography as a preoperative examination. Jpn J Radiol. 2014;32:274–81.
Acknowledgments
The authors thank their colleagues, Zeynep Gamze Kilicoglu and Can Gonen, for their kind assistance in the preparation of the manuscript.
Ethical standard
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Meric, K., Bakal, N., Aydin, S. et al. Fecal tag CT colonography with a limited 2-day bowel preparation following incomplete colonoscopy. Jpn J Radiol 33, 329–335 (2015). https://doi.org/10.1007/s11604-015-0421-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-015-0421-6