Abstract
Purpose
The use of tablet terminals has been explored in various medical settings; however, caution should be exercised when performing image diagnosis using this technology. The present study examined the characteristics of an iPad Air™ monitor and assessed radiographic image interpretations to verify the reliability of the telediagnosis of acute cerebral infarction based on magnetic resonance imaging (MRI) using a tablet terminal.
Materials and methods
The luminance of the iPad Air™ was measured using a UA-10 analyzer, and radiographic image interpretation experiments were performed in 100 patients who underwent MRI within 6 h of symptom onset. Ten physicians viewed the images on the iPad Air™ and a medical monitor, with an interval of 2 months between each interpretation.
Results
When the iPad Air™ screen was pure white, the contour lines revealed nonuniform luminance distribution. In the reading experiment, the areas under the curve of the medical monitor and the iPad Air™ were 0.9311 and 0.9431, respectively. No significant difference was observed between the medical monitor and the iPad Air™ (p = 0.113).
Conclusion
The results of the observer performance studies for detecting acute ischemic cerebrovascular disorders on an iPad Air™ were found to be similar to those on a medical monitor.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Tablets such as iPad™ devices are currently used as mobile terminals and in clinical settings are used in operating theaters and at the patient’s bedside. Because of their excellent portability, tablet terminals have been increasingly used in a variety of settings, including emergency settings, to aid therapeutic decision making [1,2,3,4,5,6].
Several guidelines have been proposed for the use of high-definition medical monitors in image diagnosis [7,8,9]. The sensitivity of the human eye is higher to dark areas of an image than to bright areas; thus, these guidelines recommend the grayscale standard display function (GSDF), which has gradation characteristics that allow the detection of differences in luminosity equally at any gradation [10]. Software calibration with the monitor of the tablet terminal for Digital Imaging and Communications in Medicine (DICOM®) has been previously demonstrated [11, 12].
Certain guidelines recommend limiting the use of tablet terminals to reference images and emergency settings. Yoshimura et al. reported that when diagnosing head computed tomography (CT) images on tablet terminals, the grayscale display of cerebral parenchyma images on general-purpose monitors had better contrast and resolution than on the medical monitors [13]. In a subsequent study, the diagnosis of head CT images made on tablet terminals showed no difference as compared with those made on medical monitors [14]. Unlike medical monitors, it is generally believed that the liquid crystal display (LCD) monitors used on tablet terminals have inconsistent luminance. To the best of our knowledge, no studies have evaluated the use of tablet monitors for the diagnosis of hyperacute ischemic cerebrovascular disorders, which are typically challenging to diagnose, based on magnetic resonance imaging (MRI) scans.
Here, we investigated the use of highly portable tablet terminals as a remote diagnostic system in emergency settings where the use of diagnostic workstations outside the workplace, such as a physician’s home, is not feasible. We assessed nonuniform luminance on the display screens of an iPad Air™ device and a medical monitor using a luminance and chromaticity uniformity analyzer and investigated the validity of the observations of acute ischemic cerebrovascular disorder on the tablet terminal, which had been previously examined by MRI for symptom confirmation in the emergency department. The objective of the present study was to conduct diagnostic imaging using an iPad Air™ and to verify whether diagnoses made on such a tablet terminal monitor are medically valid, with a view to facilitating early diagnosis of acute ischemic cerebrovascular disorders. In the emergency department, emergency personnel decide whether to refer a patient with mild cerebral infarction to a specialist; therefore, the present study was conducted in cases involving mild cerebral infarction [equivalent to a National Institutes of Health Stroke Scale (NIHSS) ≤ 5 diagnosed by an emergency physician]. The present study was based on a previously published study in the Electronic Presentation Online System (EPOS) of the European Congress of Radiology (ECR), 2016 [15]. We included the assessment of luminance uniformity of the display, adding a novel facet to the previous study.
Materials and methods
The present study was approved in advance by the Institutional Review Board of Fujita Health University Hospital (Toyoake, Aichi, Japan), and previous images generated at this facility were utilized. An opt-out methodology was applied; thus, written informed consent of the patients was not obtained; however, a completed informed consent form was obtained from all observers.
Monitors
A first-generation iPad Air™ device and a medical-grade LCD monitor (RX240, Eizo Nanao) were used in the present study. The grayscales of the medical-grade LCD monitor were fitted to the GSDF curve using a calibration software (RadiCS, Eizo Nanao). The manufacturer-specified characteristics of the two displays are summarized in Table 1.
Luminance measurements
In general, the luminance of tablet terminal monitors is nonuniform as compared with LCD medical monitors. In the present study, we measured the screen luminance of an iPad Air™ device using a Luminance and Chromaticity Uniformity Analyzer UA-10 (Topcon Technohouse) in a darkroom (ambient lighting, 0 lx) from a distance of 50 cm. The data obtained using the analyzer included directional data, since all measurements, with the exception of the center point, were obtained at an angle.
First, we created a grayscale image that divided the luminance of the iPad Air™ screen into 18 discrete categories from white to black, and subsequently measured the luminosity of the entire screen. After positioning the analyzer directly above the center point of the iPad Air™ screen, measurements were obtained 4.5 cm to the left and right of the center point. When measurements were obtained from an angle other than 90° (directly above), the data were liable to distortion; thus, we utilized the diagonal correction function of the analyzer to make adjustments. A schematic illustration of the measurement environment is presented in Fig. 1.
Next, we displayed the TG18-UNL80-3MV monitor QC test patterns (made publicly available by JIRA) on the iPad Air™ screen and measured the luminance at the center points of the quadrangle figures located at the center, as well as at each of the four corners, of the screen from a vertical distance of 50 cm (Fig. 2). Since the luminance at the center points of the quadrangles at each of the four corners was measured separately from that at the center of the monitor, we were able to ensure the uniformity of the measured values (Fig. 2). As a reference, we displayed the TG18-UNL80-2MV monitor QC test patterns (JIRA) on the LCD medical monitors and measured the luminance at the above-mentioned five points (center + four corners) at a distance of 80 cm, directly in front of the center point of the monitor.
We determined points 1* through 5*, indicating the center and the four corners of the TG18-UNL80-3MV monitor test pattern displayed on the iPad Air™ device; (ii) and (iii) we subsequently measured the luminance at points 1* through 5* from directly above (vertical) the iPad Air™ device; (iv) once the iPad Air™ device was fixed such that point 3* was in the center, we simultaneously measured the luminance at points 1* through 5*
It has been shown that the center luminance values, obtained using a telescopic luminance meter, are affected by the brightness of the areas surrounding the measurement point [7, 9]. Therefore, we measured the difference in luminance when the JIRA BN-01–18 patterns and the center points of these patterns were placed over the same grayscale image (entire image).
During these reading experiments, the maximum luminance of the LCD medical monitor was set to 400 cd/cm2, as recommended by the manufacturer (the recommended maximum luminance of the LCD medical monitor is 350 cd/cm2 for regular X-rays). The automatic luminance adjustment function of the iPad Air™ was turned off. We also installed an application designed to adjust the brightness level and set the maximum luminance at the center to approximately 400 cd/cm2; thus, the maximum luminance of the iPad Air™ used in the present study was set to 95%. Following completion of the observation experiments, we used the analyzer to confirm, from a distance of 50 cm, that the center luminance of the monitors was indeed 400 cd/cm2 (Fig. 3).
Case selection
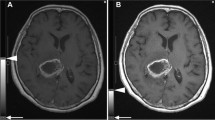
Eligible brain MRI scans were identified from the reporting system and electronic medical charts by two reviewers. One reviewer (reviewer A) is a radiology specialist with 25 years of experience, and the other (reviewer B) is a general radiologist with 14 years of experience. The inclusion criteria were patients who underwent MRI for suspected acute cerebral infarction within 6 h of symptom confirmation between 1 March 2012, and 23 September 2013, at the emergency department of Fujita Health University Hospital (Toyoake, Aichi, Japan). These patients had an NIHSS score ≤ 5, as assessed by emergency personnel. Patients with no identifiable focal lesions, either acute or chronic, served as the control group. Further, we considered patients who were clinically diagnosed with no acute cerebral infarction as healthy controls. A total of 100 patients who underwent MRI were selected, including 49 with proven acute cerebral infarction (34 men and 15 women) and 50 healthy controls (32 men and 18 women); there was some overlap in the selected patients. The average [± standard deviation (SD)] age of patients with cerebral infarction and healthy control subjects was 67.0 ± 12.8 and 63.6 ± 11.8 years, respectively. The acute cerebral infarction group included 18 cases of atherothrombosis, 15 of cardiogenic embolism, 10 of lacunar, 3 of transient ischemic attacks (TIA), and 2 classified as “other.” MRI was performed using a 1.5T MRI scanner (SIGNA EXCITE/XI with 8-channel head coil; GE Healthcare, Chicago, USA), a 1.5T MRI scanner (Achieva 1.5T Nova Dual with an 8-channel brain coil; Philips Healthcare, Best, The Netherlands), a 3T MRI scanner (Ingenia 3.0T with dS Head coil; Philips Healthcare, Best, The Netherlands), or a 3T MRI scanner (Vantage Titan 3T with a 16- or 32-channel coil; Toshiba Medical Systems Corporation, Otawara, Japan). The pulse sequence parameters and scanning conditions for each MRI scanner are shown in Table 2.
Radiographic image interpretation
Four radiologists, three brain surgeons, and three neurologists (mean experience, 16.5 ± 7.9 years; median, 14 years) agreed to participate in the observer performance studies. We ensured that at least 2 months had elapsed between interpretations of the same images. All observers were blinded to the clinical information but were notified that half of the images were from healthy control subjects, whereas the other half were from patients with acute stroke. The observers were provided with all three types of images; T2-weighted images, diffusion-weighted images, and apparent diffusion coefficient images (axial images).
We used a continuous rating scale with a line-marking method to represent each observer’s confidence level [16]. The observers were asked to indicate their confidence level regarding the presence of a cerebral infarction lesion on a linear scale ranging from 0 (left end of the scale) to 100 (right end of the scale). A score of 0 and 100 corresponded to the definite absence or definite presence of cerebral infarction lesions, respectively, whereas ratings between 0 and 100 indicated intermediate levels of confidence.
To compare the LCD medical monitors and the iPad Air™ screen, we used an OsiriX and OsiriX HD version 3.6.4 for each. To determine the average learning effect, the 100 patients were randomly displayed to each observer at each interpretation session. For each observer, the order of the monitor types during the two reading sessions was also random. No training was held prior to any session, and there was at least 2 months’ interval between the sessions. During each session, no time constraints were imposed on any observer. The ambient illumination was set to 80–100 lx at the display center, as measured using a digital photometer.
Data analysis
The detection performance of the observers was assessed using receiver operating characteristic (ROC) curve analysis, which was performed using a continuous scale, and the area under the ROC curve [A(z)] was calculated for each monitor. McNemar’s test was performed to compare the sensitivity and specificity of diagnosis based on observation on the LCD medical monitor and the iPad Air™. All statistical analyses were performed using EZR (Saitama Medical Center, Jichi Medical University), which is a graphical user interface for R (The R Foundation for Statistical Computing, version 2.13.0) [17].
Results
Luminance uniformity measurements
Data were diagonally corrected when the screen was white and displayed on the iPad Air™ device. Contour lines at the center point peak showed nonuniform luminance. When moving the monitor positions and the measurement device, we observed changes in the distribution of nonuniform luminance, as shown by the contour lines (Figs. 4, 5).
Luminance image of the monitor following diagonal correction, with a white display. (1) Measurement at the center of the monitor following diagonal correction, with a white display; (2) after moving the UA-10 analyzer 4.5 cm to the left of the center of the monitor; and (3) after moving the UA-10 analyzer 4.5 cm to the right of the center of the monitor
Using the TG18-UNL80-3MV monitor QC pattern provided by JIRA, we measured the luminance at the center of the iPad Air™ monitor and at the center points of the quadrangles at each corner of the monitor. Next, we designated the maximum luminance value at these points as Lhigh and the minimum as Llow and used Eq (1) to confirm the luminance uniformity:
The luminosity at the center of the iPad Air™ monitor was 6.23%. The luminosity at the five designated points, as assessed at a measuring point directly above the center point of the monitor, was calculated as 15.81%. For both calculations, luminance uniformity ≤ 30% was considered within the range of the reference value based on the JESRA X-0093*B-2017 guidelines. All such instances were considered indicative of maintained uniformity.
Although the guidelines indicate that cases in which the luminance uniformity was ≤ 30% are considered to have maintained uniformity, we found that directionality of the measurements decreased uniformity. We performed the same measurements on the LCD medical monitor, and using Eq (1), we found that the luminance was uniform, despite the fact that the luminance uniformity value was 3.51%. This result shows that the LCD medical monitor was far superior to the iPad Air™ device.
The center luminance measured using a telescopic luminance meter can be affected by the brightness of the areas surrounding the measurement point. We measured the difference in luminance using the JIRA BN-01–18 patterns, and the center points of these patterns were placed over the same grayscale image (entire image); the maximum luminance at the center was 7 cd/cm2 when the screen was white, indicating high luminance.
Observer performance studies
The A(z) values for the GSDF on the LCD medical monitor and the iPad Air™ device were 0.9311 [95% confidence interval (CI) 0.9131–0.9491] and 0.9431 (95% CI 0.927–0.9593), respectively (Fig. 6). The difference between the two monitors was minute. The DeLong test for two correlated ROC curves was performed (z = 1.5846, p = 0.113; Fig. 6), indicating no significant difference between the LCD medical monitor and the iPad Air™ device with respect to GSDF.
ROC curves of the LCD monitor and the iPad Air™ device with regard to the diagnosis of acute ischemic cerebrovascular disorders. There was no statistically significant difference between the LCD medical monitor and the iPad Air™ device with respect to the detection of acute ischemic cerebrovascular disorders. ROC receiver operating characteristic, LCD liquid crystal display
McNemar’s test indicates that the iPad Air™ device exhibited higher specificity than that of the LCD medical monitor for the diagnosis of acute ischemic cerebrovascular disorders using MRI; however, the sensitivity of the two devices was comparable in this respect (Table 3).
Discussion
In the present study, both an iPad Air™ device and a medical LCD monitor were used to read MRI scans and accurately diagnose acute ischemic cerebrovascular disorders. No significant difference was found between the diagnostic results obtained from the scans viewed on an iPad Air™ device as compared with those viewed on an LCD medical monitor. We believe that the excellent contrast in diffusion-weighted images is one of the reasons for the comparable performance of the two devices. Further study regarding the detectability of acute ischemic cerebrovascular disorders on CT images, which is known to be more difficult, is required to determine the degree to which the nonuniformity of luminance due to the directionality of LCD screen backlighting affects the results.
In the present study, we demonstrate that the luminance at a short distance from the screen of the iPad Air™ device is less uniform than that of the LCD medical monitor when used for image interpretation. Major changes in luminance were observed at the margins. We also found that the iPad Air™ screen had a high degree of directionality, since measurements obtained directly above (vertical) had only slight luminance reduction at the measurement point. This indicates that, during the examination of images on a tablet terminal, it is advisable to observe the image from a central point as far above the image as possible. It is difficult to calibrate the gamma value using the iOS operating system owing to legal/licensing/copyright issues, meaning that it is impossible to calibrate the device to the GSDF recommended by DICOM®. One way to avoid this software-specific problem is to create a system that calibrates each application on the tablet terminal. Although this is currently being attempted for some applications, none of the available products are compatible with the iOS operating system. Some commercially available iOS products allow gamma value calibration. As tablet terminal and software development are advancing rapidly, we anticipate an imminent solution to this problem.
In addition to the present study, several other studies have also found no difference between an iPad™ screen and an LCD medical monitor with respect to the display of medical images (excluding mammograms) [14, 18,19,20]. Caffery et al. reported that the backlighting function of mobile terminals deteriorates with long-term use, which decreases the maximum luminance [21], and that the contrast ratio also undergoes significant changes over time. In the present study, the luminance changes at the iPad Air™ monitor margins were in proportion to that at the center [21]; thus, we believe that the luminance at the margins likely undergoes a similar decrease over time. Nonuniformity of the screen luminance occurs on tablet terminals depending on the location and angle of observation. Unlike LCD medical monitors, tablet terminals facilitate observation under various conditions. We believe that this inconsistent observational environment is one of the reasons why multiple studies have reported poor results with the use of tablet terminals. However, tablet terminals are less expensive than LCD medical monitors, and new models are released each year. The problem of the decreased luminance over time of tablet terminals can be solved by need-based replacement of old with new units. The current Japanese guidelines [9] recommend that image observations on a tablet terminal should be performed indoors and that their use should be limited to reference images and clinical images in emergency settings. The results of the present study indicate that, in addition to these stipulations, it is advisable to observe images from a point directly in front of the center of the screen, especially with mobile devices that use LCD screens with a high degree of backlight directionality. However, the aforementioned onset-related problems due to LCD screens were not caused by the OS. Although the brightness of LCD panels has progressively improved over time, similar problems may occur with tablets using iOS and other OSs (e.g., Android and Windows). Products with organic light-emitting diodes may cause problems different from those caused by more commonly used LCD panels; however, this is yet to be confirmed, since these devices have only recently been developed. A product known as FVT-air [22], which was developed for Windows, facilitates the combination of general-use PC monitor gamma guards and DICOM®. On the basis of the author’s experience, this can also be used with tablet terminals.
The present study has some limitations. First, MRI scans were used to diagnose acute cerebral infarction in the image interpretation experiments. Compared with CT scans, MRI scans have better contrast, which could have reduced potential differences in image interpretation. In addition, four different types of MRI scanners were used, and although the characteristics of the control group for each scanner were similar, we cannot eliminate the possibility of selection bias. Secondly, the analyzer used in the present study is the Luminance and Chromaticity Uniformity Analyzer UA-10, and although precision was maintained during assessments and comparisons between similar monitors, it is not a spectral luminance meter. Although luminance was assessed using an iPad Air™ device and an LCD medical monitor, assessment was not performed with the calibration of spectral luminance meters, thereby suggesting that limited comparison of luminance among various monitors should be considered. Furthermore, in the present study, assessments were made using an earlier model iPad Air™ tablet. New tablet models are commercially available each year; hence, our results may not be entirely applicable to all models. Lastly, TIA cases in clinical settings may not always exhibit high signal intensity on diffusion-weighted images. Among those who showed no abnormal MRI findings, we designated subjects who did not experience acute cerebral infarction during the entire clinical presentation as “normal” cases. In contrast, among the subjects in the acute cerebral infarction group, two were discharged because no abnormal findings were noted on MRI scans obtained in the emergency department; and thus, were determined not to have experienced acute cerebral infarction based on clinical signs. After a few days, these two subjects underwent repeated MRI; since these additional studies indicated that the lesions with weak signal intensity on diffusion-weighted images should have been detected, we included the first and second MRI studies in the acute cerebral infarction group. Images of a patient who showed no signs of acute cerebral infarction but experienced one several days later were included. In the present study, no differences were found between the LCD medical monitor and the iPad Air™ device in terms of lesion detection rates as abnormalities. As such, when the detection of abnormalities is impossible or when the diffusion-weighted images show no clear lesions, more attention should be paid to detailed clinical examination. Although we did not assess MR angiography (MRA) in the present study, no contrast- or clarity-related issues have been reported during the use of mobile devices to observe CT angiograms and MRA [23]. Our results suggest that the contrast of the iPad Air™ device does not differ from that of the LCD medical monitor and that the use of the iPad Air™ device to examine MRA studies is unlikely to pose any problems.
With respect to the guidelines on reference imaging using tablet terminals [8, 9], it should be noted that the use of tablet terminals is restricted to reference images and clinical images in an emergency setting. We believe that tablet terminals are not recommended for image diagnosis because of the following three problems: panel calibration, operability, and security. Perhaps the inability to calibrate may be resolved in the near future. With respect to the panel on tablet terminals, organic electroluminescent panels may be adopted, in which case the tablet panels should be physically retested. With respect to operability, the screen size is a bottleneck for tablet-specific operations, image transfer, and display. As a portable device, it is unlikely that the screen size of tablet terminals will change considerably in the future. If there is a significant difference between the operability of the DICOM® viewer used in routine medical practice and that used on a tablet, it could be a major hindrance for users. The DICOM® viewer for tablet terminals should have comparable operability with the standard image interpretation environment. The use of a thin client facilitates the operation of a DICOM® viewer for Windows on a tablet terminal. Network system security with a virtual private network has become standard practice; thus, the possibility of wiretapping and data falsification is reduced during data transfer. However, several problems persist when transferring images to a tablet terminal. With the DICOM® viewer used by most tablet terminals, image data are transferred to the mobile terminal. The direct transfer of personal information to regular mobile tablet terminals poses a security risk. The use of a thin client prevents retention of personal information on the mobile terminal. Furthermore, the transfer of DICOM® images is limited by the data transfer speed. Compared with direct data transfer, DICOM® images can be displayed on the mobile terminal in small packets by selecting the thin client mode. We conducted experiments using a type of DICOM® viewer software that facilitated the transfer of DICOM® images to a tablet terminal for observation. However, in cases where a radiologist or clinician attempts to make a diagnosis based on images on mobile devices, the duration between the initiation and completion of the diagnosis should be as short as possible. In addition, it is critical to ensure the security of the mobile device and data while displaying medical images. Notably, the practical data transmission speed is longer than the normal speed due to the network delays associated with mobile devices; a mobile phone network is used and the data are encrypted. Of note, the use of mobile devices also prevents data leakage; therefore, it is desirable to construct a system that can be used by thin clients, including those with “zero footprint,” due to decreased traffic.
To construct an environment in which images can be easily viewed on a tablet terminal, we believe that introducing thin clients would be useful. As mentioned earlier, using thin clients may help to develop a system that ensures operability and security. In addition, monitor calibration may help to minimize the hurdles of displaying reference images on a tablet terminal. Conversely, in the event that these problems cannot be resolved or if a radiologist cannot be assigned to emergency care, we believe that the quality of medical care needs to be ensured in the future with a diagnostic support system that utilizes artificial intelligence.
Conclusions
The results of the observer performance studies for the detection of acute ischemic cerebrovascular disorders using MRI scans on an iPad Air™ device were similar to those on an LCD medical monitor with GSDF calibration. Furthermore, the diagnosis was performed with high accuracy using both devices and was found not to be significantly different. The accuracy of the diagnosis of other diseases using MRI and other images on the iPad Air™ and other modalities should be investigated.
References
Turney BW, Reynard JM. Obtaining patient feedback in an outpatient lithotripsy service is facilitated by use of a touch-screen tablet (iPad™) survey. Urolithiasis. 2014;42(4):317–21.
Maruyama K, Kin T, Saito T, Suematsu S, Gomyo M, Noguchi A, et al. Neurosurgical simulation by interactive computer graphics on iPad. Int J Comput Assist Radiol Surg. 2014;9(6):1073–8.
Chao C, Tan J, Castillo EM, Zawaideh M, Roberts AC, Kinney TB. Comparative efficacy of new interfaces for intra-procedural imaging review: the Microsoft Kinect, Hillcrest Labs Loop Pointer, and the Apple iPad. J Digit Imaging. 2014;27(4):463–9.
Johnson PT, Zimmerman SL, Heath D, Eng J, Horton KM, Scott WW, et al. The iPad as a mobile device for CT display and interpretation: diagnostic accuracy for identification of pulmonary embolism. Emerg Radiol. 2012;19(4):323–7.
Eguchi T, Takasuna K, Kitazawa A, Fukuzawa Y, Sakaue Y, Yoshida K, et al. Three-dimensional imaging navigation during a lung segmentectomy using an iPad. Eur J Cardiothorac Surg. 2012;41(4):893–7.
McNulty JP, Ryan JT, Evanoff MG, Rainford LA. Flexible image evaluation: iPad versus secondary-class monitors for review of MR spinal emergency cases, a comparative study. Acad Radiol. 2012;19(8):1023–8.
Norweck JT, Seibert JA, Andriole KP, Clunie DA, Curran BH, Flynn MJ, et al. ACR-AAPM-SIIM technical standard for electronic practice of medical imaging. J Digit Imaging. 2013;26(1):38–52.
Japan Radiological Society. Guidelines for the handling of digital images, version 3.0. 2015. http://www.radiology.jp/content/files/20150417.pdf. Accessed 5 May 2018.
JIRA. quality assurance (QA) guideline for medical imaging display systems. 2017. http://www.jira-net.or.jp/publishing/files/jesra/JESRA_X-0093B_2017.pdf. Accessed 5 May 2018.
National Electrical Manufacturers Association. Digital imaging and communications in medicine (DICOM). Part 14. Grayscale standard display function. http://medical.nema.org/Dicom/2011/11_14pu.pdf. Accessed 5 May 2018.
BARCO. MediCal QAWeb Mobile. https://www.barco.com/en/Products/Software/Medical-calibration-and-QA-software/Visual-calibration-and-QA-for-your-tablet.aspx/. Accessed 5 May 2018.
EIZO. RadiCS. http://www.eizoglobal.com/press/releases/htmls/radicsmobile.html. Accessed 5 May 2018.
Yoshimura K, Shimamoto K, Ikeda M, Ichikawa K, Naganawa S. A comparative contrast perception phantom image of brain CT study between high-grade and low-grade liquid crystal displays (LCDs) in electronic medical charts. Phys Med. 2011;27(2):109–16.
Yoshimura K, Nihashi T, Ikeda M, Ando Y, Kawai H, Kawakami K, et al. Comparison of liquid crystal display monitors calibrated with gray-scale standard display function and with γ 2.2 and iPad: observer performance in detection of cerebral infarction on brain CT. AJR. 2013;200(6):1304–9.
Hattori H, Shinpei A, Yoshitaka I, Toyama H. Consideration of reliability in the diagnosis of acute ischemic cerebrovascular disorders about MRI in iPad air. In: EPOS of the ECR, 2016. https://doi.org/10.1594/ecr2016/C-1280.
Kobayashi T, Xu XW, MacMahon H, Metz CE, Doi K. Effect of a computer-aided diagnosis scheme on radiologists’ performance in detection of lung nodules on radiographs. Radiology. 1996;199(3):843–8.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48(3):452–8.
John S, Poh AC, Lim TC, Chan EH, le Chong R. The iPad tablet computer for mobile on-call radiology diagnosis? Auditing discrepancy in CT and MRI reporting. J Digit Imaging. 2012;25(5):628–34.
Park JB, Choi HJ, Lee JH, Kang BS. An assessment of the iPad 2 as a CT teleradiology tool using brain CT with subtle intracranial hemorrhage under conventional illumination. J Digit Imaging. 2013;26(4):683–90.
Caffery LJ, Armfield NR, Smith AC. Radiological interpretation of images displayed on tablet computers: a systematic review. Br J Radiol. 1050;2015(88):20150191.
Caffery LJ, Manthey KL, Sim LH. The effect of time in use on the display performance of the iPad. Br J Radiol. 1063;2016(89):20150657.
RealVision. FVT-air. https://realvision.co.jp/service/fvt_air/. Accessed 5 May 2018.
Randhawa PA, Morrish W, Lysack JT, Hu W, Goyal M, Hill MD. Neuroradiology using secure mobile device review. Can J Neurol Sci. 2016;43(4):529–32.
Acknowledgements
The authors would like to express our gratitude to Kumiko Yoshimura of Nagoya University for her cooperation in the preparatory stage of this study, the doctors from the Department of Radiology, the Department of Neurosurgery and the Department of Neurology of Fujita Health University for their cooperation in the reading experiment, and Masao Ohashi, a radiological technologist in the Department of Radiology at Fujita Health University Hospital, for his cooperation with luminance measurement on the monitors. Special thanks also go to Dr. Shinpei Akiyama of Kyoto Prefectural University of Medicine, Department of Radiology, and Dr. Nobuo Kako of the AICHI Clinic of Healthcare.
This study was announced at the 74th Annual Meeting of the Japan Radiological Society (Yokohama city, Kanagawa prefecture, Pacifico Yokohama, April 16–19, 2015) and the ECR https://doi.org/10.1594/ecr2016/C-1280.
This work was supported by JSPS KAKENHI Grant-in-Aid for Young Scientists (B) 26860407.
This study was approved in advance by the Institutional Review Board of Fujita Health University (Toyoake, Aichi, Japan).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author has no conflict of interest to disclose with respect to this article.
About this article
Cite this article
Hattori, H., Kuwayama, Y., Inui, Y. et al. Reliability of diagnosing acute ischemic cerebrovascular on magnetic resonance imaging disorders using iPads. Jpn J Radiol 36, 726–735 (2018). https://doi.org/10.1007/s11604-018-0763-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-018-0763-y