Abstract
Purpose
To investigate a method for optimizing the display conditions of brain magnetic resonance (MR) images.
Materials and methods
We retrospectively analyzed brain MR images of 120 adults classified into screening, acute cerebral infarction, and brain tumor groups (n = 40 each). Two observers independently displayed the images on a monitor and optimized the display conditions using the W/L and U/L methods. In the W/L method, the observers manipulated the width and level of the display window, while in the U/L method they manipulated the upper and lower levels of the window. The times required were compared between the two methods. Additionally, the appropriateness of the determined window setting was evaluated visually by the respective observer to exclude the possibility that rough, suboptimal adjustment shortened the adjustment time.
Results
For both observers and all groups, the time required for optimization was significantly shorter for the U/L method than for the W/L method. The appropriateness of the window setting for the U/L method was equal to or better than that for the W/L method.
Conclusion
Manipulating the upper and lower levels of the display window appears to improve the efficiency of interpreting brain MR images through rapid optimization of the display condition.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Medical images such as plain radiographs, computed tomography (CT) images, and magnetic resonance (MR) images are displayed on the monitor of a picture archiving and communication system (PACS) viewer for image interpretation. Unlike images displayed on film, the interpreter can adjust the monitor display conditions, which are crucial for the visual interpretation of medical images. In CT, the display window can be standardized for each organ (the brain, lungs, solid organs, and bone) because the pixel value expressed using Hounsfield units (HU) is calibrated, such that water shows 0 HU and air shows −1000 HU, and has quantitative meaning [1, 2]. In contrast, standardizing the display condition of MR images is difficult because the signal intensities are not normalized and vary greatly depending on scanners, imaging parameters, and patients [3]. Although standardization has been attempted [3,4,5,6,7], interpreters commonly adjust the display conditions of MR images during interpretation subjectively and manually.
The window width (difference between the upper and lower limits of the display window) and window level (average of the upper and lower limits of the window) are frequently used as parameters for adjusting the display condition [8], which is defined by the combination of these two parameters. On most current PACS viewers, these two parameters are manipulated by dragging the mouse to adjust the display condition [width and level (W/L) method].
Although the signal intensities of MR images vary depending on various conditions, the pixel values are generally zero or greater. It is supposed that an appropriate display can be achieved efficiently in most cases by manipulating only the upper limit of the window while fixing the lower limit at zero. The lower limit should be increased only to darken the background regions or to emphasize the display contrast. When using the conventional W/L method, the upper and lower limits of the window are changed simultaneously. Widening the window width increases the upper limit and decreases the lower limit. Raising the window level increases both the upper and lower limits of the window. It is difficult to fix the lower limit at zero during adjustment procedures, which may cause difficulty in optimizing the display condition. A method that manipulates the upper and lower limits of the window independently [upper and lower (U/L) method] has the potential to achieve an appropriate display more rapidly and to improve the efficiency of image interpretation compared with the conventional W/L method.
In this study, we compared the U/L and W/L methods for optimizing the display of brain MR images in terms of the time required for adjustment. Two observers independently displayed the images on a monitor and optimized the display conditions for visual interpretation using the U/L and W/L methods. The time required for adjustment was recorded and compared between the two methods. It should be noted that the adjustment time can be shortened if the observer quits adjustment before carefully determining the ideal display conditions for the observer. Therefore, the appropriateness of the determined window setting was evaluated by the respective observer to exclude the possibility that a short adjustment time is derived from rough, suboptimal adjustment. The purpose of this study was to determine whether the U/L method allows shortening the adjustment time without compromising the subjective appropriateness of the resultant display condition.
Materials and methods
Subjects
We retrospectively analyzed patients who underwent brain MR imaging for clinical indications. We selected 120 adults consisting of three groups of 40 patients each. Group 1 included 13 males and 27 females, aged 48.3 ± 15.1 (mean ± SD) years, who underwent brain MR imaging for screening. Group 2 included 30 males and 10 females (67.9 ± 15.1 years) reported to have acute cerebral infarction. Group 3 included 26 males and 14 females (57.5 ± 14.6 years) who underwent brain MR imaging for evaluation of a diagnosed or suspected primary intraparenchymal brain tumor. The Institutional Review Board at our facility approved this retrospective study, and the need for informed consent was waived.
MR imaging
All brain MR imaging studies were performed on a 1.5-T clinical scanner (Signa HDxt; GE Healthcare, Milwaukee, WI) with the 12-channel head component of the head-neck-spine coil. In groups 1 and 2, T1-weighted (T1w) spin echo images, T2-weighted fast spin echo images, diffusion-weighted echo planar images, and fluid-attenuated inversion recovery images were evaluated. In group 3, contrast-enhanced T1w spin echo images and three-dimensional, fat-saturated, contrast-enhanced T1w images using a fast spoiled gradient recalled acquisition in the steady-state sequence were also evaluated. All images evaluated were acquired in the axial plane. Gadoteridol (Eisai, Tokyo, Japan) was used as contrast medium at a dose of 0.1 mmol/kg.
Methods to optimize display conditions
Two board-certified diagnostic radiologists with 8 and 18 years’ experience in the interpretation of brain MR images independently optimized the display conditions of the images displayed on a PACS monitor (EV Insite Net; PSP Corp., Tokyo, Japan) using the W/L and U/L methods. The display conditions were adjusted visually by radiological technologists in advance, and the images were transferred to the PACS with the information about the determined window center and window width. When the radiologists opened the image file, the images were initially displayed using the predefined window center and width. Subsequently, the radiologists changed the display conditions using the W/L and U/L methods to make them appropriate for diagnosis subjectively.
In the W/L method, the window width and level were manipulated by mouse dragging. The window level was changed by moving up and down, and the window width was changed by moving right and left.
In the U/L method, the display condition was adjusted by manipulating a scale bar presented beside the image (Fig. 1). A reference value was automatically calculated from the window center and window width registered as the DICOM tags as follows: (window center + window width/2). On the scale bar, the signal intensity was expressed as the percentage of the reference value, and the initial display window had a range of 0–100%. The image display was optimized by independently manipulating the upper end of the scale bar, representing the upper limit of the window, and the lower end, representing the lower limit of window. The upper limit was adjusted first, and the lower limit was changed if needed.
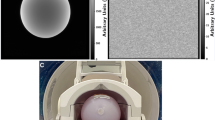
Appearance on the PACS monitor presenting a contrast-enhanced T1w image before (a) and after (b) optimization of the display condition. The scale bar is set on the left side of the image. In the U/L method, the upper end of the scale bar (arrowhead), representing the upper limit of the window, is adjusted first. The lower end of the bar (arrow), representing the lower limit of the window, is manipulated when necessary
The display conditions of all image series for each patient were optimized using the W/L and U/L methods. One condition, the combination of the window level and width, was determined for each series. The time required to optimize all series for each patient and the determined window settings were recorded. The optimization procedures using the two methods were performed on separate occasions at 2-week or longer intervals. In each patient group, the W/L method was used first for half of the patients, and the U/L method was used first for the remaining half.
After optimization using the W/L and U/L methods had been completed for all patients, the appropriateness of the determined display conditions was compared visually between the two methods. Images were displayed side by side using the window level and width determined by the two methods, and the appropriateness for diagnosis was judged by the respective observer who determined the display condition: observers 1 and 2 evaluated the appropriateness of the display conditions determined by observers 1 and 2, respectively. Images acquired using different techniques (T1w images, T2-weighted images, etc.) were evaluated separately. The observers were blinded to the methods used for optimization and classified the comparison into one of the following five categories: left is definitely better, left is possibly better, equal, right is possibly better, and right is definitely better.
Statistical analysis
The Wilcoxon signed-rank test was used to compare the time required for optimization between the two methods. The sign test was used to compare the appropriateness of the window setting between the two methods. A P value <0.05 was deemed to indicate a statistically significant difference.
Results
Figure 2 shows the time required to optimize the displays of all image series for each patient. For observer 1, median times for the W/L and U/L methods were 50 and 37 s, respectively, in group 1, 56.5 and 43.5 s, respectively, in group 2, and 82 and 72.5 s, respectively, in group 3. For observer 2, median times for the W/L and U/L methods were 55 and 39 s, respectively, in group 1, 65.5 and 49.5 s, respectively, in group 2, and 128.5 and 84.5 s, respectively, in group 3. For both observers, the time required for optimization using the U/L method was significantly shorter than that using the U/L method in all subject groups (P < 0.001).
For observer 1, the display condition determined by the U/L method was significantly more appropriate for T1w images in group 3 than that determined by the W/L method (Table 1). No other significant differences were found between the two methods. For observer 2, the U/L method was judged significantly better than the W/L method for five comparisons. The display condition determined by the W/L method was not judged better for any comparisons.
Discussion
In this study, we compared the U/L method (manipulating each of the upper and lower limits of the display window independently) and the conventional W/L method (manipulating the window width and level to optimize the display condition) for interpretation of brain MR images.
The U/L method required less time to optimize the display than the W/L method. The adjustment time can be shortened if the observer does not perform thorough optimization and quits adjustment before deciding about the ideal display conditions for the observer. However, the appropriateness of the display condition was judged to be similar for both methods by observer 1, and the display condition determined by the U/L method tended to be judged as more appropriate than that determined by the W/L method by observer 2. Better or comparable appropriateness achieved by the U/L method indicates that shortening of the time required is not due to rough, suboptimal adjustment. Considering the time shortening without compromising the subjective appropriateness of the resultant display condition, the U/L method appears to be superior to the conventional W/L method for optimizing the display of brain MR images and would permit improving the efficiency of image interpretation.
It is desirable to change the display condition during interpretation of one image series. For example, the upper level of the display window should be increased, resulting in a darker appearance, when evaluating the internal structure of a strongly enhanced lesion on contrast-enhanced T1w images. In contrast, the upper limit should be lowered, resulting in a brighter appearance, to detect more weakly enhanced lesions. Convenience in achieving the display preferred by an interpreter would encourage the interpreter to optimize the display condition frequently, improving the quality of image interpretation.
To optimize the display using the U/L method, when an interpreter feels that the target region for visual evaluation appears too dark, he/she can lower the upper limit of the window and make the appearance brighter. When an interpreter feels that the target region appears too bright, he/she can increase the upper limit of the window. The lower limit of the window is manipulated only when it is necessary to darken background regions or to enhance image contrast. In this study, the lower limit of the window was left at zero in most cases, and the display condition was optimized only by manipulating the upper limit. This simplicity of manipulation appeared to have contributed to shortening the time required for optimization.
Generally, the pixel values in MR images are zero or greater, and background signals outside the body are zero, except for noise. Setting the lower limit at a positive value may eliminate information in hypointense regions, while a negative lower limit reduces image contrast. Fixing the lower limit at zero preserves information in hypointense regions without unnecessarily reducing image contrast. The lower limit may be manipulated when interpreting MR angiograms. Contrast between the arterial lumen and brain parenchyma in MR angiography is enhanced using various data-acquisition techniques [9, 10], and the following adjustment scheme may further improve the clarity of the arteries. First, the upper limit is adjusted to enhance the brightness of the arteries properly. Next, the lower limit is increased to depress the brightness of brain parenchyma. These two steps with different target regions (arteries vs. brain parenchyma) and different manipulations (changing the upper limit vs. changing the lower limit) can be clearly separated using the U/L method. Generally, the U/L method allows the standardization of optimization procedures, and only the upper limit needs to be manipulated in most cases.
Using the W/L method, image contrast is defined by the window width while brightness is defined by the window level. Actually, it is not clear how to determine the appropriate contrast for an image. A different window width may be appropriate for a given image when a different window level is used. It is necessary to search for the appropriate combination of window width and window level by trial and error. To reduce the brightness in background regions, a procedure must be selected from two alternatives: narrowing the window width or increasing the window level. Use of a combination of the two parameters and difficulty in standardizing the procedures appear to make optimization of the display by the W/L method complicated and time-consuming.
Introduction of the U/L method does not preclude use of the W/L method. When a scale bar is provided for the U/L method, mouse dragging can be still used for the W/L method. An interpreter can usually optimize the display condition by the U/L method and select the W/L method optionally with no additional manipulation for conversion between the two methods. For example, the W/L method may be used for detailed evaluation of a particular lesion. The window level is fixed to appropriately display the lesion, and the window width is manipulated to change the contrast within the lesion or against the surrounding tissues.
In this study, the initial display condition was adjusted visually by radiological technologists in advance. The appropriateness of adjustment by technologists may have influenced the results. In many facilities, the window setting determined automatically by the MR scanner is used as the initial display condition without visual adjustment. In automatic adjustment, the display condition may be influenced by the presence of profound hyperintensity caused by artifacts, leading to a large discrepancy from the appropriate display condition. Without visual adjustment performed by the technologists, optimization of the display condition might be more time-consuming, possibly increasing differences between the W/L and U/L methods. In this preliminary study we only evaluated brain MR images, and the usefulness of the U/L method in optimizing the display of various MR images, including MR angiograms and images of other regions, should be studied in the future. Although shortening of the time required using the U/L method was shown for both observers, the absolute values of the times and the results of the appropriateness of the display conditions were different between them. The actual optimization process would vary among observers, and further investigation involving many observers is desired.
Conclusion
We compared the U/L and W/L methods for optimizing the display condition for the interpretation of brain MR images. The U/L method manipulating the upper and lower limits of the window independently required less time to determine the appropriate display condition compared with the conventional W/L method manipulating the window width and window level. The U/L method appears to improve the efficiency of interpreting MR images through rapid optimization of the display condition.
References
Pomerantz SM, White CS, Krebs TL, Daly B, Sukumar SA, Hooper F, et al. Liver and bone window settings for soft-copy interpretation of chest and abdominal CT. AJR Am J Roentgenol. 2000;174:311–4.
Lamba R, McGahan JP, Corwin MT, Li CS, Tran T, Seibert JA, et al. CT Hounsfield numbers of soft tissues on unenhanced abdominal CT scans: variability between two different manufacturers’ MDCT scanners. AJR Am J Roentgenol. 2014;203:1013–20.
Nyúl LG, Udupa JK. On standardizing the MR image intensity scale. Magn Reson Med. 1999;42:1072–81.
Robitaille N, Mouiha A, Crépeault B, Valdivia F, Duchesne S. The Alzheimer’s disease neuroimaging initiative. Tissue-based MRI intensity standardization: application to multicentric datasets. Int J Biomed Imaging. 2012;2012:347120.
Sasaki M, Ida M, Yamada K, Watanabe Y, Matsui M. Standardizing display conditions of diffusion-weighted images using concurrent b0 images: a multi-vendor multi-institutional study. Magn Reson Med Sci. 2007;6:133–7.
Hirai T, Sasaki M, Maeda M, Ida M, Katsuragawa S, Sakoh M, et al. Diffusion-weighted imaging in ischemic stroke: effect of display method on observers’ diagnostic performance. Acad Radiol. 2009;16:305–12.
Nagashima H, Doi K, Ogura T, Fujita H. Automated adjustment of display conditions in brain MR images: diffusion-weighted MRIs and apparent diffusion coefficient maps for hyperacute ischemic stroke. Radiol Phys Technol. 2013;6:202–9.
Gillespy T 3rd, Rowberg AH. Displaying radiologic images on personal computers. J Digit Imaging. 1993;6:151–63.
Graves MJ. Magnetic resonance angiography. Br J Radiol. 1997;70:6–28.
Wheaton AJ, Miyazaki M. Non-contrast enhanced MR angiography: physical principles. J Magn Reson Imaging. 2012;36:286–304.
Acknowledgements
We thank Mr. Hiroki Miyatake for his cooperation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest in relation to the present study.
About this article
Cite this article
Hara, T., Inoue, Y., Ukisu, R. et al. Methods for optimizing the display conditions of brain magnetic resonance images. Jpn J Radiol 35, 622–627 (2017). https://doi.org/10.1007/s11604-017-0669-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-017-0669-0