Abstract
Purpose
To investigate feasibility of high-pitch acquisition protocol for imaging of pediatric abdomen.
Materials and methods
The study group consisted of 90 patients scanned with high-pitch acquisition protocol (pitch = 3) by 64-slice dual-source CT (DSCT) scanner. Fifty-four patients scanned with standard protocol (pitch = 1.5) by 16-slice single-source CT scanner comprised the control group. Anteroposterior and lateral diameters of abdomen, effective diameter, scan time and length, qualitative and quantitative noise levels, volumetric CT dose index (CTDIvol), dose length product (DLP), and size-specific dose estimations were compared between groups.
Results
The mean scan time of high-pitch CT protocol was shorter than control protocol (1.66 ± 0.31 vs. 4.1 ± 0.75 s; p < 0.001). The high-pitch protocol reduced the radiation dose by 48% (CTDIvol and DLP values 0.94 mGy and 32.2 mGy-cm vs. 1.59 mGy and 61.5 mGy-cm; p < 0.001, respectively). Although image noise was higher with high-pitch acquisition, there was no significant effect on diagnostic confidence. Voluntary and involuntary artifacts were less frequent in high-pitch protocol (p < 0.001). Interobserver agreement was moderate in terms of artifact and very good in terms of diagnostic confidence assessment.
Conclusion
High-pitch acquisition protocol by DSCT yields significant radiation dose reduction without compromising image quality and diagnostic confidence for pediatric abdomen imaging.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
There is a direct relationship between increased number of CT scans and high radiation dose exposure levels. Although the number of CT scans accounts for a small percentage of whole X-ray examinations (10%), it is still responsible for the largest contribution of radiation dose exposure [1, 2]. There is also a growing concern regarding CT-associated increased cancer risk [2, 3]. Furthermore, about 2–5% of CT examinations are performed in pediatric population who are more sensitive to effects of radiation [4, 5]. According to the ALARA (as low as reasonably achievable) principle, the first aim of a CT examination is to achieve adequate image quality with lowest possible radiation dose exposure [6]. Dual-source CT (DSCT) scanners became widely available in clinical use with the advent of CT technology. Unlike previous generations, DSCT scanners consist of two X-ray sources and two detector systems placed in a single gantry. This design makes it possible to perform the high-pitch acquisition protocols in daily routine practice. The second X-ray tube and detector system provide gap-free volume coverage with pitch values as high as 3.4, depending on the desired field of view [7]. The aim of this study was to investigate the feasibility of high-pitch acquisition protocol on a DSCT scanner for imaging of pediatric abdomen.
Materials and methods
Clinical data
A total of 90 patients who underwent abdominal CT scan within a two-year period of time by a DSCT scanner with high-pitch acquisition protocol were enrolled in this institutional review board approved prospective study. An additional 54 patients who underwent standard-pitch mode abdominal CT scans comprised the control group. Patients smaller than 12 months and whose largest body diameter above 26 cm at the level of femur heads were excluded from analyses. The mean (± SD) age was 55.8 ± 30 and 64.4 ± 39 months in the study and control groups, respectively. Study group consists of 70 males and 20 females, whereas control group consists of 37 males and 17 females. In study group, the most common reason (77 out of 90 patients, 85%) for a CT scan was to evaluate disease progress in oncologic patients (neuroblastoma: 32 patients, Wilms tumor: 17 patients, malignant lymphoma: 10 patients, hepatoblastoma: 3 patients, Ewing’s sarcoma: 3 patients, primitive neuroectodermal tumor: 3 patients, rhabdoid tumor: 2 patients, renal cell carcinoma: 1 patient, Langerhans cell histiocytosis: 1 patient, acute myeloid leukemia: 1 patient, chordoma: 1 patient, rhabdomyosarcoma: 1 patient, medulloblastoma: 1 patient, teratoma: 1 patient). The other indications for a CT scan were as follows in decreasing order: clinical suspicion for an abdominal mass (4 patients), fever of unknown origin (3 patients), inflammatory bowel disease (2 patients), urinary infection and vesicoureteral reflux (1 patient), tuberculosis (1 patient), trauma (1 patient), and complicated acute appendicitis (1 patient). In control group, the most common reason (44 out of 54 patients, 81%) for a CT scan was also to evaluate the disease progress in oncologic patients (neuroblastoma: 16 patients, malignant lymphoma: 12 patients, Wilms tumor: 3 patients, rhabdomyosarcoma: 4 patients, gonadal tumor: 2 patients, hepatoblastoma: 1 patient, appendiceal carcinoid tumor: 1 patient, gingival Kaposi’s sarcoma: 1 patient, hepatocellular carcinoma: 1 patient, cardiac tumor: 1 patient, osteosarcoma: 1 patient, renal cell carcinoma: 1 patient). The other indications for a CT scan were as follows in decreasing order: clinical suspicion for an abdominal mass (4 patients), hepatosplenomegaly (1 patient), immunodeficiency (1 patient), intestinal intussusception (1 patient), abdominal pain (1 patient), tuberculosis (1 patient), and ureteropelvic junction obstruction (1 patient).
CT parameters
The first generation DSCT system with high-pitch acquisition protocol (pitch = 3) was used for the study group (Definition, Siemens Medical Systems; Erlangen, Germany). Patients in the control group underwent standard abdominal CT scan (pitch = 1.5) with a 16-slice CT (Sensation 16, Siemens Medical Systems; Erlangen, Germany) scanner. CT parameters are summarized in Table 1. Automatic exposure control system was used in both groups (CARE Dose 4D, Siemens). Iterative reconstruction was not used in both groups. The CT scans included the body area between the diaphragm to the proximal part of both thighs. Contrast-enhanced abdominal CT scans were obtained in the venous phase according to our radiology department’s abdominal imaging protocol. CT scans automatically started 60 s after the intravenous contrast material injection. There was no need for sedation before CT scan in both groups.
Qualitative assessment
Qualitative assessment was made by grading the noise, image quality, and artifacts, which are related to patient, diaphragm, or bowel movements. The images were evaluated by a 3-point scoring system for the assessment of noise (1 = less than usual noise; 2 = optimal noise; 3 = noise affecting interpretation), a 4-point scoring system for the assessment of diagnostic confidence (1 = fully confident; 2 = probably confident; 3 = limited confidence level; 4 = unacceptable), and a 4-point scoring system for the assessment of artifacts (1 = no artifact; 2 = minor artifacts but diagnostic image quality preserved; 3 = moderate artifacts; 4 = severe artifacts).
Quantitative assessment
For quantitative assessment of noise, regions of interests (ROIs) of at least 10 mm2 were drawn in the right liver lobe parenchyma, lumen of abdominal aorta at the level of superior mesenteric artery origin, right psoas muscle at the level of common iliac artery bifurcation, and outside the abdominal wall at the level of umbilicus. Two ROIs were placed for each area. The unit of measurements was Hounsfield unit (HU). The ROIs were manually drawn and care was taken to avoid vessels. Mean and standard deviation (SD) values were recorded for each of the two ROIs, and the average of these values was calculated. The level of noise was defined as the standard deviation of attenuation values of each ROI. Both qualitative and quantitative assessments were made by two radiologists (4 and 8 years of experience in reading pediatric abdominal CT scans). Interobserver agreement was assessed with the results of 30 patients evaluated by the second observer.
Scanning time, length, and radiation dose
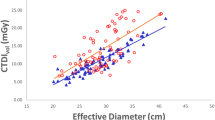
The scan times were recorded after each examination from the CT panel. The scan length was calculated by dividing the dose length product (DLP) by volumetric computed tomography dose index (CTDIvol). CTDIvol and DLP values were extracted from CT acquisition protocols. The anteroposterior diameter (APD) and lateral diameters (LD) of the abdomen were measured at the level of the umbilicus in all patients. The effective diameter (ED) and size-specific dose estimates (SSDE) related to APD, LD, APD + LD, and ED were calculated using conversion factors according to AAPM (The American Association of Physicists in Medicine) Report 204 [8].
Statistical analysis
All parameters were compared among both groups using Chi-squared test, independent sample t test, Fisher’s exact test, and Mann–Whitney U test. Interobserver agreement was assessed using kappa statistic and intraclass correlation reliability (ICR). The correlation was classified as poor (κ < 0.20), fair (κ = 0.21–0.40), moderate (κ = 0.41–0.60), good (κ = 0.61–0.80), and very good (κ = 0.81–1.00). Statistical package for social sciences (SPSS) version 18.0 (SPSS Inc.) was used for statistical analysis. A value of p < 0.05 was considered a statistically significant difference.
Results
Demographic data
The mean values of APD, LD, APD + LD, and ED for both groups are presented in Table 2. There was no significant difference between both groups regarding the age (p = 0.176) and abdominal circumference measurements (APD, LD, and ED; p > 0.05). Interobserver ICR was 0.987 and 0.986 in terms of APD and LD measurements, respectively (p < 0.001).
Qualitative assessment
In the study group, all CT examinations (90 scans) had a noise level of two (optimal noise; Fig. 1a). In control group, 41 of 54 CT scans (76%) had a noise level of one (less than usual noise; Fig. 1b) and residual 13 CT scans (24%) had a noise level of two. There were no CT scan with a noise of level of three (noise affecting interpretation) in both groups. The noise levels between both groups demonstrated statistically significant difference (p < 0.001). Qualitative assessment of noise and artifact scores in both groups is summarized in Table 3. The artifacts were more commonly encountered in the control group compared study group (p < 0.001) (Fig. 2). The diagnostic confidence was rated as 1 (fully confident) for both groups. Interobserver agreement was poor in terms of noise levels (κ = 0.199); however, there was no case with noise level of 3 (noise affecting interpretation) for both observers. Interobserver agreement was moderate in terms of artifact and was very good in terms of diagnostic confidence assessment (κ = 0.565 for artifact assessment; κ value could not be calculated in terms of diagnostic confidence because > 90% of CT examinations were rated as 1 by two observers).
A boy with left adrenal neuroblastoma. a Axial contrast-enhanced CT scan obtained with high-pitch acquisition protocol (CTDIvol: 0.76 mGy, DLP: 26 mGy cm) when he was 5-year old. b Follow-up CT scan obtained with standard-pitch acquisition protocol (CTDIvol: 1.61 mGy, DLP: 63 mGy cm) when he was 7-year old. In addition (b) was rated as 1 (less than usual noise) and (a) was rated as 2 (optimal noise) in terms of noise. None of the CT scans rated as 3 (noise affecting interpretation). Despite increased level of noise with high-pitch acquisition protocol, CT image was adequate to evaluate the left adrenal mass (arrowhead, a) and also liver metastases (arrows, a) with lower radiation dose in 5-year old infant
Quantitative assessment
The mean values and SDs of CT densities (HU) are presented in Table 4. There was no statistically significant difference between both groups regarding the mean densities obtained from psoas muscle and liver, and regarding the SD values of abdominal aorta and outside the abdominal wall at the level of umbilicus as well. The study group had lower mean density values than control group obtained from abdominal aorta and outside the abdominal wall at the level of umbilicus. The study group had higher SD values than control group obtained from psoas muscle and liver. Interobserver ICR was > 0.7 in terms of quantitative assessment (p < 0.05).
Scanning time, length, and radiation dose
The mean scan time was significantly lower in the study group compared to control group (1.66 ± 0.31 vs 4.1 ± 0.75 s; p < 0.001). There was significant difference between both groups in the terms of scan length (study group: 33.2 ± 4.7 cm, control group: 37.3 ± 4.7 cm; p < 0.001). Forty-eight percent of radiation dose reduction was achieved in the study group compared to control group (Table 5, Fig. 1).
Discussion
The increased number of CT scans particularly in pediatric population has raised concerns due to possibility of increased rate of carcinogenesis. Pearce et al. [9] reported increased risk of leukemia and brain tumor as a consequence of radiation exposure in childhood. The alliance for radiation safety in pediatric imaging group has launched “Image gently campaign” to draw attention on this issue [10]. The level of radiation dose exposure by CT scans can be reduced by various methods such as avoiding unnecessary examinations, tube current and voltage modulation, limiting of the scan range in the z-axis and number of CT phases, noise reduction filters, and iterative reconstructions [11,12,13,14,15]. The automated tube current modulation (ATCM) technique is one of the most effective methods to decrease the radiation dose exposure levels. ATCM system automatically decreases or increases the tube current in proportion to tissue thickness of the scanning area. On the other hand, the exposed radiation level by a CT scan could also be significantly reduced with a shorter scanning time. The high-pitch acquisition protocols can reduce scanning time due to rapid table movement through the gantry. The high-pitch imaging protocol has been more effectively used, initially, in cardiac imaging. In patients with lower heart rates (< 70 beats per min), the whole heart can be imaged at a low radiation dose [7, 16]. Subsequently, various anatomic regions such as head and neck, trunk, and vascular compartments were also effectively imaged by high-pitch acquisition protocols. The primary gain of this method is to achieve diagnostic images with a lower radiation dose and shorter scanning time compared to standard imaging protocols [17,18,19,20,21,22,23,24,25,26]. In this study, we investigated the value of high-pitch acquisition protocol (pitch = 3) on a first-generation DSCT scanner for imaging of pediatric abdomen, and our results demonstrated a significant radiation dose reduction (48% according to DLP, 42% according to SSDE of effective diameter) without hampering image quality compared to standard-pitch mode CT protocol. Although scan length of control group is 10% longer than the study group, this finding does not explain about 50% reduction in radiation dose.
Technical anatomy of the DSCT scanner played a major role for radiation dose reduction in this study. The DSCT scanners consist of two X-ray tubes and two detector systems placed in a single gantry. The lower temporal resolution of the standard CT scanners is the major obstacle for high-pitch imaging. The gantry rotation time limits maximum table speed. Nevertheless, DSCT scanners obtain higher temporal resolutions due to faster gantry rotation times compared to standard CT scanners. Therefore, high-pitch imaging is more feasible on DSCT scanners compared to standard CT machines. The second X-ray tube and detector system provide gap-free volume coverage with pitch values as high as 3.4, depending on the desired field of view [7].
In the present study, the average CTDIvol and DLP values of the high-pitch abdominal CT acquisition protocol were significantly lower than the standard abdominal CT protocol (0.94 mGy and 32.2 mGy cm vs 1.59 mGy and 61.5 mGy cm; p < 0.001, respectively). Vorona et al. [27] reported average CTDIvol and DLP values for standard abdominal CT scans as 6.75 mGy and 275.7 mGy cm, respectively. Reid et al. [28] concluded that pediatric abdominal CT scans could be obtained at a dose range (CTDIvol) of 10–15 mGy without using tube current modulation techniques while preserving diagnostic image quality. The average CTDIvol and DLP values of standard abdominal CT scans were lower in our study compared to previously mentioned studies [27, 28]. Small abdominal circumference of our patients and ATCM system used in our study may explain the lower DLP values. In the present study, abdominal CT scans acquired with high-pitch acquisition protocol on a DSCT scanner were about 2.5 times faster than standard abdominal CT scans. This finding was consistent with the previous literature [17, 21, 23, 29, 30]. The artifacts caused by either voluntary (patient based) or involuntary (movement of internal organs) motions, which are more commonly seen in pediatric population, can be significantly reduced with rapid scanning protocols. In the present study, motion artifacts were more commonly encountered in the control group than the study group (p < 0.001). However, it should be emphasized that rapid movement of the table through the gantry may increase the level of noise, due to attenuation of X-ray beam. The images acquired with high-pitch acquisition protocol showed slightly higher noise levels in our study as expected, however, did not influence the diagnostic confidence. Although interobserver agreement was low in terms of noise, this discordance did not influence interpretation adversely, and the diagnostic confidence as well. In helical CT scans, reconstruction algorithms require additional data which are obtained at the beginning and end of the scan region. The X-ray tube–detector pair needs to turn an extra half or full rotation to acquire the required data, since these areas are out of the planned scan region. This phenomenon is called over-ranging which results in redundant radiation dose burden. The amount of the over-ranging increases with higher table speed and pitch values [31]. New techniques such as dynamic or adaptive collimation can reduce this effect [11]. Furthermore, CT scanners automatically increase the mA as a compensation mechanism to the rapid table speed and pitch values [32]. Despite these drawbacks, significant radiation dose reduction was achieved by high-pitch acquisition protocol in our study, which is also in line with the literature as well [23, 33].
Study limitations
Our study had several limitations that should be addressed. First of all, the first-generation DSCT scanner used in this study has a limited field of view of 26 cm due to the compact geometry of the machine. Second, the age of the patients had a wide range which could influence the individual exposed radiation dose level, yet mean age of the patients between both groups was similar. Third, we did not evaluate alternative radiation dose reduction strategies (e.g., modulation of kVp and mAs values, iterative reconstruction, and dynamic or adaptive collimation algorithms). Fourth, we did not evaluate optimal bolus timing for high-pitch protocol. The correct bolus timing may influence enhancement pattern in high-pitch protocol due to faster table movement. The time interval between the contrast injection and scanning may be longer for high-pitch protocol compared to standard scan. However, further studies are warranted to investigate optimal bolus timing for high-pitch imaging protocols. Finally, we did not evaluate the diagnostic performance of high-pitch acquisition protocol. This could be a subject for further study.
Conclusion
Our results demonstrate that high-pitch acquisition protocol is a feasible method in pediatric abdominal imaging. High-pitch acquisition protocol by a DSCT yields significant radiation dose reduction without compromising image quality and diagnostic confidence for imaging of the pediatric abdomen.
References
Charles M. UNSCEAR report 2000: sources and effects of ionizing radiation. United Nations Scientific Committee on the effects of atomic radiation. J Radiol Prot. 2001;21:83–6.
Smith-Bindman R, Lipson J, Marcus R, Kim KP, Mahesh M, Gould R, et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med. 2009;169:2078–86.
Berrington de González A, Mahesh M, Kim KP, Bhargavan M, Lewis R, Mettler F, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009;169:2071–7.
Brenner DJ, Hall EJ. Computed tomography—an increasing source of radiation exposure. N Engl J Med. 2007;357:2277–84.
UNSCotEoAR. Sources and effects of ionizing radiation UNSCEAR 2008. Report to the general assembly with scientific annexes. United Nations 2010.
Mettler FA Jr, Thomadsen BR, Bhargavan M, Gilley DB, Gray JE, Lipoti JA, et al. Medical radiation exposure in the U.S. in, 2006: preliminary results. Health Phys. 2008;2008(95):502–7.
Berdon EW, Brenner DJ, Brody AJ. The ALARA (as low as reasonably achievable) concept in pediatric CT intelligent dose reduction. Multidisciplinary conference organized by the Society of Pediatric Radiology. August 18–19. Pediatr Radiol. 2001;32:217–313.
Petersilka M, Bruder H, Krauss B, Stierstorfer K, Flohr TG. Technical principles of dual source CT. Eur J Radiol. 2008;68:362–8.
Boone J, Strauss K, Cody D, McCollough C, McNitt-Gray M, Toth T, et al. Size-specific dose estimates (SSDE) in pediatric and adult body CT examinations (Task Group 204). College Park, Md: American Association of Physicists in Medicine. 2011.
Pearce MS, Salotti JA, Little MP, McHugh K, Lee C, Kim KP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012;380:499–505.
The Image Gently Alliance. Image gently campaign. 2007. Available via https://www.imagegently.org/About-Us/The-Alliance. Accessed 28 Dec 2014.
Deak PD, Langner O, Lell M, Kalender WA. Effects of adaptive section collimation on patient radiation dose in multisection spiral CT. Radiology. 2009;252:140–7.
Greess H, Nömayr A, Wolf H, Baum U, Lell M, Böwing B, et al. Dose reduction in CT examination of children by an attenuation-based on-line modulation of tube current (CARE Dose). Eur Radiol. 2002;12:1571–6.
Greess H, Wolf H, Baum U, Lell M, Pirkl M, Kalender W, et al. Dose reduction in computed tomography by attenuation-based on-line modulation of tube current: evaluation of six anatomical regions. Eur Radiol. 2000;10:391–4.
Hara AK, Paden RG, Silva AC, Kujak JL, Lawder HJ, Pavlicek W. Iterative reconstruction technique for reducing body radiation dose at CT: feasibility study. AJR Am J Roentgenol. 2009;193:764–71.
Kalender WA, Wolf H, Suess C, Gies M, Greess H, Bautz WA. Dose reduction in CT by on-line tube current control: principles and validation on phantoms and cadavers. Eur Radiol. 1999;9:323–8.
Leschka S, Stolzmann P, Desbiolles L, Baumueller S, Goetti R, Schertler T, et al. Diagnostic accuracy of high-pitch dual source CT for the assessment of coronary stenoses: first experience. Eur Radiol. 2009;19:2896–3903.
Amacker NA, Mader C, Alkadhi H, Leschka S, Frauenfelder T. Routine chest and abdominal high-pitch CT: an alternative low dose protocol with preserved image quality. Eur J Radiol. 2012;81:392–7.
Bauer RW, Schell B, Beeres M, Wichmann JL, Bodelle B, Vogl TJ, et al. High-pitch dual-source computed tomography pulmonary angiography in freely breathing patients. J Thorac Imaging. 2012;27:376–81.
Beeres M, Schell B, Mastragelopoulos A, Herrmann E, Kerl JM, Gruber-Rouh T, et al. High-pitch dual-source CT angiography of the whole aorta without ECG synchronisation: initial experience. Eur Radiol. 2012;22:129–37.
Goetti R, Baumuller S, Feuchtner G, Stolzmann P, Karlo C, Alkadhi H, et al. High-pitch dual-source CT angiography of the thoracic and abdominal aorta: is simultaneous coronary artery assessment possible? AJR Am J Roentgenol. 2010;194:938–44.
Han BK, Lindberg J, Grant K, Schwartz RS, Lesser JR. Accuracy and safety of high pitch computed tomography imaging in young children with complex congenital heart disease. Am J Cardiol. 2011;107:1541–6.
Korn A, Fenchel M, Bender B, Danz S, Thomas C, Ketelsen D, Claussen CD, et al. High-pitch dual-source CT angiography of supraaortic arteries: assessment of image quality and radiation dose. Neuroradiology. 2013;55:423–30.
Lell MM, May M, Deak P, Alibek S, Kuefner M, Kuettner A, et al. High-pitch spiral computed tomography: effect on image quality and radiation dose in pediatric chest computed tomography. Invest Radiol. 2011;46:116–23.
Schell B, Bauer RW, Lehnert T, Kerl JM, Hambek M, May A, et al. Low-dose computed tomography of the paranasal sinus and facial skull using a high-pitch dual-source system—first clinical results. Eur Radiol. 2011;21:107–12.
Schulz B, Jacobi V, Beeres M, Bodelle B, Gruber T, Lee C, et al. Quantitative analysis of motion artifacts in high-pitch dual-source computed tomography of the thorax. J Thorac Imaging. 2012;27:382–6.
Schulz B, Potente S, Zangos S, Friedrichs I, Bauer RW, Kerl M, et al. Ultra-low dose dual-source high-pitch computed tomography of the paranasal sinus: diagnostic sensitivity and radiation dose. Acta Radiol. 2012;53:435–40.
Vorona GA, Ceschin RC, Clayton BL, Sutcavage T, Tadros SS, Panigraphy A. Reducing abdominal CT radiation dose with the adaptive statistical iterative reconstruction technique in children: a feasibility study. Pediatr Radiol. 2011;41:1174–82.
Reid J, Gamberoni J, Dong F, Davros W. Optimization of kVp and mAs for pediatric low dose simulated abdominal CT: is it best to base parameter selection on object circumference? AJR Am J Roentgenol. 2010;195:1015–20.
Hardie AD, Mayes N, Boulter DJ. Use of high-pitch dual-source computed tomography of the abdomen and pelvis to markedly reduce scan time: clinical feasibility study. J Comput Assist Tomogr. 2011;35:353–5.
Nie P, Wang X, Cheng Z, Ji X, Duan Y, Chen J. Accuracy, image quality and radiation dose comparison of high-pitch spiral and sequential acquisition on 128-slice dual source CT angiography in children with congenital heart disease. Eur Radiol. 2012;22:2057–66.
van der Molen AJ, Geleijns J. Overranging in multisection CT: quantification and relative contribution to dose—comparison of four 16-section CT scanners. Radiology. 2007;242:208–16.
Bulla S, Blanke P, Langer M, Pache G. Letter to the editor re: low-dose computed tomography of the paranasal sinus and facial skull using a high-pitch dual-source system first clinical results. Eur Radiol. 2011;21:1447–8 (author reply 1451).
Koh H, Ong CC, Choo YS, Liang CR, Tan GH, Lim TC, et al. Radiation dose and image quality in pediatric cardiac Computed tomography: a comparison between sequential and third-generation dual-source high-pitch spiral techniques. Pediatr Cardiol. 2016;37:1397–403.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Written informed consent was waived by IRB in this study.
About this article
Cite this article
Atlı, E., Akpınar, E., Ünal, E. et al. The feasibility of high-pitch acquisition protocol for imaging of the pediatric abdomen by dual-source CT. Jpn J Radiol 36, 437–443 (2018). https://doi.org/10.1007/s11604-018-0744-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-018-0744-1