Abstract
Research in public health, epidemiology, and medical sociology has debated the health impacts of income inequality. A common hypothesis is that socioeconomic contexts in neighborhoods, regions, or entire nation states shape individuals’ health and inequalities in health. Several reviews have concluded that the distribution of income within a society contributes to poor health. More recent research has focused on welfare state arrangements and their relevance to cross-national variations in health and inequalities in health. We argue that the welfare state determines and mediates the extent of inequalities in health through healthcare, social policy and public health. Many studies have been published in the last decade that have tried to examine the role played by these influences on health and health inequalities. This review will (1) summarize the extant research on the association between welfare state factors and health outcomes, (2) discuss how research theorizes the role of welfare state characteristics for between- and within-country differences in health, (3) present different approaches to empirically investigate the association between welfare state, health and inequalities in health, and (4) provide methodological considerations in this field of research.
Zusammenfassung
Sowohl in der medizinischen Soziologie, Public-Health-Forschung als auch in der Epidemiologie wird seit Jahrzehnten diskutiert, inwieweit eine ungleiche Einkommensverteilung mit der gesundheitlichen Lage von Individuen und gesamten Gesellschaften zusammenhängt. Auf der Ebene von Nachbarschaften, Regionen oder Nationalstaaten soll der sozioökonomische Kontext einerseits die Gesundheit einzelner, andererseits auch die ungleiche Verteilung von Gesundheit insgesamt maßgeblich bestimmen. Empirische Studien zeigen, dass die Einkommensungleichheit mit einer schlechteren Gesundheit auf der Individual- wie Populationsebene assoziiert ist. Neuere Forschungsarbeiten konzentrieren sich auf den Wohlfahrtsstaat und auf wohlfahrtsstaatliche Arrangements als Determinanten von Gesundheit und gesundheitlicher Ungleichheit. Neben wohlfahrtsstaatlichen Arrangements haben nach Ansicht jüngerer Forschungsansätze das Gesundheitswesen wie auch Public-Health-Programme wesentlichen Einfluss auf die Verteilung von Gesundheit innerhalb von Nationen. In den letzten Jahren sind zahlreiche Studien veröffentlicht worden, die sich mit dem Stellenwert wohlfahrtsstaatlicher Arrangenemts, des Gesundheitswesens und von Public-Health-Programme für die Gesundheit und gesundheitliche Ungleichheit befasst haben. Der vorliegende Beitrag fasst die vorliegende Studienlage zum Stellenwert von Wohlfahrtsstaat und wohlfahrtsstaatlichen Arrangements, des Gesundheitswesens und von Public-Health-Programmen für die Verteilung von Gesundheit innerhalb und zwischen Nationen zusammen. Hierbei wird die Studienlage dargestellt und diskutiert. Darüber hinaus werden methodische Forschungsansätze zur Thematik vorgestellt und kritisch evaluiert.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Societies throughout the developed and developing world have made dramatic progress in health over the past 100 years. Mortality rates have fallen sharply, and life expectancy has increased in most countries. According to the UN’s World Population Prospects, life expectancy has increased since the 1950s, and will continue to increase on every continent (see Fig. 1). However, significant differences in life expectancy both between and within societies illustrate the importance of context in a population’s health. One of the first scholars to focus on welfare state outcomes in the explanation of national differences in population health was Richard G. Wilkinson (1990, p. 392), who stated in the light of his own findings and findings from Rodgers (1979) that “as countries get richer the relationship between life expectancy and average income appears to weaken and be replaced by the growing influence of income distribution”. According to Wilkinson, this “epidemiological transition” marks a point in global development when the material conditions that support health are sufficient for rifts to emerge between socioeconomic strata due to psychosocial consequences of inequality.
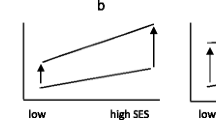
To explain differences in population health, Wilkinson and Pickett (2011) suggests that, among affluent nations, life expectancy is lower in more unequal societies because income inequality in itself has a negative effect on members’ health. In contrast to this contextual effect of income inequality, others have suggested that the relationship between income inequality and life expectancy results from a composition effect where the income inequality level of a country embodies the sum of individual life chances within a society (Gravelle 1998; Jen et al. 2009). This composition effect pointed to an important determinant of health on the individual level: socioeconomic status. Socioeconomic status reflects a variety of resources such as money, knowledge, prestige, power, and beneficial social connections that make it possible to protect and improve health, and is often measured by income, education and occupational status (Link and Phelan 1995). Therefore, less privileged members of a society live in worse health than more privileged members due to the difference in resource ownership (Phelan et al. 2010), which in turn is reflected by the level of income inequality. According to general medical sociological theories, socioeconomic status contributes to individual health through material (e. g. physical working conditions, neighborhood conditions), psychosocial (e. g. financial strain, deprivation, psychosocial working conditions), and behavioral pathways (e. g. smoking behavior, physical activity, nutrition) (see Fig. 2) (Galobardes et al. 2006; Elo 2009; Braveman et al. 2011; Braveman and Gottlieb 2014; Moor et al. 2017). While this debate is mainly about the mechanisms explaining differences in population health by means of macro-level (income inequality) and micro-level factors (socioeconomic status)Footnote 1, only a few studies have investigated the underlying patterns of socioeconomic inequalities (Maio 2012, p. 41). Coburn (2000, p. 136) criticized the narrow focus on the social determinants of health by arguing that there is “an overwhelming tendency to focus on the possible social/psycho-biological mechanisms through which social factors might be tied to health … [and] a startling lack of attention to the social/political/economic context of SES or income inequality-health status relationships”.
In line with Coburn’s criticism, the body of cross-national research into health and health inequalities has placed a larger focus on the wider policy context determining education, work and income within a country (Bergqvist et al. 2013, pp. 1–2; Woolf and Braveman 2011). In particular, a welfare state perspective has been developed to understand the causes of the causes of health and health inequalities (Beckfield et al. 2015, p. 228). The welfare state has been considered as a relevant macro-level factor determining and mediating the extent of socioeconomic inequalities in health by healthcare, social policy and public health (Thomson et al. 2016). Many studies have been published in the last decade trying to unravel the role of welfare states for health and health inequalities. The current review summarizes the extant research on the association between welfare state factors and health outcomes, discusses how research theorizes the role of welfare state characteristics for between- and within-country differences in health and inequalities in health, presents different approaches to empirically unravel the association between welfare state, health and inequalities in health, and provides methodological considerations in this field of research.
2 Public Health and the “Three Worlds of Welfare”
Cross-national research into health and health inequalities has increasingly examined the role of the welfare state as a broad determinant of health. Based on Esping-Andersen’s “welfare state as a system of stratification” (Esping-Andersen 1990, pp. 69–77), studies on adults and adolescents have investigated whether and how the welfare state is linked to within- and between-country differences in health and inequalities in health. Although researchers have suggested various classifications and approaches to measure welfare states (Bambra 2007), Esping-Andersen’s ‘three worlds of welfare’ are still highly influential in the literature because it explains how the welfare state shapes population health and socioeconomic inequalities in health by mediating individuals’ life chances via the welfare services that they receive (see Fig. 2).
In his influential work, Esping-Andersen (1990) provides a typology of welfare states based on three dimensions: decommodification (the extent and generosity of welfare state services that determine individuals’ dependency on the market, particularly in terms of pensions, unemployment benefit and sickness insurance), social stratification (conditions under which welfare state policies contribute to an equalization of opportunity structures), and the private–public mix (the relative contributions of the state, family, the voluntary sector and the market in welfare state provision) (Bambra 2007; Hurrelmann et al. 2011; Schröder 2019). By applying these dimensions, Esping-Andersen was able to define three ideal regime types: liberal, conservative and social democratic. In liberal-regime countriesFootnote 2 (such as Australia, New Zealand, Canada, Ireland, the UK and the USA), decommodification is minimal, and welfare benefits are modest, often based on strict entitlement criteria and means tested. The conservative regime type (including countries such as Finland, France, Germany, Italy or Switzerland) is characterized by its “status-differentiating” welfare programs, in which welfare benefits depend on work-based insurance contributions. These status-differentiating welfare programs result in differing decommodification effects and contribute to the consolidation of social stratification. Finally, the social democratic regime typeFootnote 3 (including countries such as Austria, Belgium, Denmark, Norway or Sweden) provides universal and comparatively generous benefits, and the state plays a strong interventional role promoting equality in different forms of income redistribution (such as progressive taxation, minimum wage policies, tax credits, and cash transfers to lower income groups).
Researchers have suggested modifications to Esping-Andersen’s regime typology (Arts and Gelissen 2002, 2010; Bambra 2007; Eikemo and Bambra 2008). One of the most important modifications relates to the inclusion of other regime types such as the ‘Latin-rim’ (Leibfried 1992) or ‘Southern’ regime type (Bonoli 1997; Ferrera 1996; Saint-Arnaud and Bernard 2003) (characterized by a fragmented system of welfare provision and high reliance on the family and voluntary sector), the ‘Confucian’ regime type (Karim et al. 2010) (characterized by a minimal welfare state with a strong emphasis placed on the family and on the voluntary sector based on Confucian ethics), and the ‘Eastern European’ regime type (Fenger 2007) (characterized by its unique political background and a shift from a Communist towards a somewhat more liberal welfare state focusing on marketization and decentralization). Further modifications of the regime typology have been made in public health using the actual extent of services provided by different welfare states (Bambra 2005a, 2005b), or extending the focus to politics and policies as determinants of welfare state programs (Navarro 1999; Navarro and Shi 2001; Navarro et al. 2006).
Although the regime typology of Esping-Andersen has been modified and extended, the logic linking welfare state characteristics with population health and inequalities in health is still based on the idea of the welfare state as a system of stratification. For example, in a study by Eikemo et al. (2008b, p. 2282), the authors state that “welfare states provide a variety of social transfers (such as housing-related benefits, unemployment, pensions, and sickness and disability benefits) as well as key services (most notably healthcare or social services), which together mediate the relationship between socioeconomic position and health.” Accordingly, it has been assumed that population health and inequalities in health vary by welfare regime type with better health outcomes in the most generous regime (social democratic regime) compared to types with lower levels of decommodification and welfare benefits (such as in the liberal regime type).
A number of empirical reviews have focused on the association of welfare regime types with health and inequalities in health (Beckfield and Krieger 2009; Bergqvist et al. 2013; Brennenstuhl et al. 2012; Muntaner et al. 2011). On a national level, reviews indicate that the Scandinavian regime type generally shows better health outcomes than other regime types in infant and child mortality, but not in other health outcomes such as in (working-age/old-age/all-age) mortality, life expectancy or self-rated health. Moreover, given studies thus far, early research reviews conclude that although the Scandinavian regime type has relatively low levels of economic inequality, it does not consistently have low levels of socioeconomic inequalities in health. According to a review by Bergqvist et al. (2013), only one out of four studies using Esping-Andersen’s typology or a modified typology found the smallest inequalities in health in social democratic countries in men but not in women. In other studies, inequalities in mortality and self-rated health were lower in the conservative-regime countries compared to the social democratic countries. This “Scandinavian welfare paradox of health” was also found in other studies using different regime typologies (Beckfield and Krieger 2009; Bergqvist et al. 2013; Brennenstuhl et al. 2012; Muntaner et al. 2011). When explaining this empirical puzzle, several theories have been proposed, drawing on methodological issues (see Sect. 5) and existing theories of inequalities in health (Mackenbach 2012; Bambra 2011). Therefore, although the application of welfare regime typologies is still very popular, the evidence regarding the influence of welfare regimes on health and inequalities in health is inconclusive and mixed.
3 Going Beyond the Regime Typology—The Institutional Approach
The ‘Scandinavian Puzzle’ and the general criticism towards using regime typologies have led to alternative approaches towards unraveling the role of welfare state characteristics for health and inequalities in health. As Lundberg (2008, p. 1106) puts it, using regime typologies “may be helpful for descriptive purposes, they are much less useful if we really want to open the black box and analyze what aspects of welfare state are of importance”. Instead, Lundberg (2008) suggests studying specific welfare programs and their influences on health and inequalities in health. Therefore, it is necessary to consider the link between specific welfare institutions (e. g. unemployment benefits) and the health of specific social groups (e. g. the unemployed). Studies on specific welfare programs (social policy, healthcare and public health) could be classified into five groups: studies focusing on family benefits, pension benefits, economic assistance and unemployment benefits, access to health/medical care and public health interventions.
The first group analyzes the relevance of family benefits (e. g. family cash and tax benefits, paid parental leave, childcare support, child allowance, parental insurance, childcare leave) for the individual health of specific social groups such as lone mothers or children in poor households (Bergqvist et al. 2013 ; Hank and Steinbach 2019). For example, Aitken et al. (2015) reviewed seven studies analyzing the relevance of paid maternity leave for mothers’ health, and found a positive correlation between paid maternity leave and mental and physical health. They conclude that paid leave may protect mothers from financial strain and enables them to spend more time away from the workplace and to recover from the physical effects of childbirth. Similar studies indicate that generous and universal family policies are beneficial for family members’ health and socioeconomic living conditions (Bergqvist et al. 2013). In contrast, recent studies focusing on the impact of income support programs for low-income families (e. g. the Earned Income Tax Credit (EITC) in the USA or the Family Tax Credit (FTC) in New Zealand) on individual health found contradictory results. Studies showed a positive effect of income support programs on maternal and child health (Hamad and Rehkopf 2016; Strully et al. 2010), whereas others revealed no or only moderate effects for adult health (Larrimore 2011; Pega et al. 2013, 2014, 2016). For example, Wicks-Lim and Arno (2017) applied difference-in-difference analysis to measure low birth weight rate, prenatal health and asthma-related pediatric hospitalization in 90 low- and middle-income neighborhoods before and after the expansion of the New York State and New York City EITC policy between 1997 and 2010. The results showed contradictory findings of reduction on low birth weight rate by increasing EITC benefits, but no effects for prenatal health or asthma-related pediatric hospitalization.
The second group of studies focuses on the relevance of pension benefits for individual health in old ages (Bergqvist et al. 2013). Studies hypothesized that the level of generosity and kind of public benefits (basic pensions of persons with no or low earnings; income pensions given on the basis of work contribution) are related to the health of the older people and retirees in particular. Accordingly, it is proposed that more generous pension benefits and universal basic pensions relate to higher incomes that enable investing in health-enhancing products and protect against poverty-related health burdens (Norström and Palme 2010; Esser and Palme 2010). The few studies published so far indicate that more generous pensions and universal basic pensions (in particular for women) predict better self-rated health and well-being (Esser and Palme 2010). Only few studies have yet been published focusing on the role of pension benefits for the individual health of different socioeconomic groups in old age. Farrants (2017) investigated associations of net replacement rates of pensions with inequalities in the self-rated health of pensioners using the Health Survey for England and the Swedish Study of Income and Living Conditions from 1991 to 2011. Accordingly, annual inequalities in self-rated health by education of pensioners (log odds) were modeled against net replacement rates in pensions by linear regression. Results were contradictory, and indicated a negative association between the net replacement rates of pensions and the magnitude of inequalities in health in England, but no significant association for Sweden. In an ecological studyFootnote 4 of 16 European countries that was carried out from 2004 to 2014, Reeves et al. (2017) found that greater public pensions entitlement is associated with decreased unmet medical need due to financial reasons. This was observed in particular among the poorest income group. Results also showed that the association between out-of-pocket payment and unmet medical need due to financial reasons was mitigated by higher levels of public pensions entitlement. Therefore, public pensions enable people to meet the various costs involved in seeking healthcare and in keeping healthy, particularly for the lowest socioeconomic groups in old age.
The third group of studies analyzes the influence of economic assistance and unemployment benefits on the health of the unemployed and of those in financial need (Bergqvist et al. 2013). The rationale behind these studies is that the mechanisms linked to the generosity of unemployment benefits (e. g. wage replacement rate, duration of coverage, flexibility in the entitlement and maintenance of unemployment benefits) could act as a buffer against loss of wages, alleviate poverty, and subsequently protect individuals from the negative health consequences of unemployment (Cylus et al. 2015). According to a recent review, the generosity of unemployment benefits does have a positive effect on the health of the unemployed, as is shown for mental health, subjective well-being and financial strain (O’Campo et al. 2015). For example, in a current study by Vahid Shahidi et al. (2016) using the European Sociological Survey from 2012, the association of national unemployment insurance replacement rates with the self-rated health of the unemployed and the employed was analyzed using cross-level interactions in a multilevel framework. Study results indicated that more generous levels of unemployment benefits were significantly associated with narrowed inequality in self-rated health between the unemployed and those in employment. Therefore, the increased risks of a poor self-rated health status among the unemployed were lower in those countries that have higher levels of unemployment benefits.
Bergqvist et al. (2013) identified a fourth group of studies that analyze inequalities in access to health/medical care. Several determinants on the country level have been found to be associated with decreased socioeconomic inequalities in access to healthcare such as public financing and provision of services, medical density and the existence of a gatekeeping system that coordinates patients’ care paths via general practitioners (Or et al. 2008). Further, Jones et al. (2006) found with data from the European Community Household Panel (1994–1997) that supplementary private insurances are associated with income, better self-rated health and higher rates of specialist visits indicating that those on a high income might benefit from the existence of private supplementary insurance when it comes to access to healthcare systems as well as to health. According to a review from Huber and Mielck (2010), a similar situation is observable for Germany that allows people to opt out of public insurance and into private insurance if their income exceeds a certain level. Accordingly, the review indicates that the benefits of private insurance with regard to new, innovative drugs, organ transplantations, financial burden due to copayments, waiting times, and communication between patient and physician compared to those with public insurance are more generous. However, whether these observed benefits in access and use of healthcare of higher socioeconomic groups affect inequalities in health is highly debated in public health and health services research, and existing evidence is limited (Davis 1991; Oliver and Mossialos 2004; Pfaff and Pförtner 2016). An exemplary study that tries to unravel the relevance of healthcare-related factors for inequalities in health has been conducted by Klein et al. (2016). They analyzed the influence of disease-related (tumor stage, biological characteristics), patient-related (comorbidity, health behavior, psychosocial characteristics), and healthcare-related factors (treatment, screening uptake, medical expertise) on socioeconomic inequalities in health-related quality of life among patients with prostate cancer six months after radical prostatectomy using a prospective observational study among 246 patients. A stepwise approach was conducted comparing changes in the association between socioeconomic status and health-related quality of life when explanatory factors were included in the regression model. The result indicated a strong association between health-related quality of life six months after treatment and lower socioeconomic status measured by income, occupation and education. Socioeconomic inequalities in quality of life changed only slightly when explanatory factors were considered in the regression model with stronger explanatory power of patient- and healthcare-related factors. Thus, other potential social determinants of health might play an important role in inequalities in patient health which are not related to the healthcare system, such as equity in early life, labor market disadvantages, psychosocial burdens at work, and material deprivation. Therefore, public health research describes the healthcare system not as the primary factor accounting for inequalities in health, but rather as a moderator of levels of inequalities in health (Marmot and Allen 2014). For example, Banks et al. (2006) showed with cross-national data from England and the US that universal access to health/medical care is associated with better health outcomes, but nonetheless found differences in health outcomes in the top socioeconomic groups in England and the US. They concluded that other social factors might contribute to inequalities in health that cannot be explained by the healthcare system alone.
Additionally, as a fifth stream, research aims to assess how welfare states influence inequalities in health institutionally through public health interventions (Thomson et al. 2016). Public health interventions play an important role in reducing inequalities in health, as they aim to prevent the occurrence (primary prevention) or the development (secondary prevention) of specific diseases. They are implemented at different levels (national, regional, local, or individual level), focusing on upstream or downstream determinants of public health. Accordingly, upstream interventions focus on fundamental structures and economic conditions influencing individuals’ health and health behavior by state or institutional regulations (e. g. tobacco price regulations or smoking bans). Downstream interventions focus directly on the individual and include behavioral approaches for prevention or disease management (e. g. media campaigns against smoking, and smoking cessation programs).Footnote 5 Although public health interventions are intended to improve or sustain health, they can also have unintended adverse effects. According to Lorenc and Oliver (2014), public health interventions could lead to direct harm, psychological harm, group and social harm, opportunity cost harm and equity harm. The latter is of particular interest as some interventions may generate socioeconomic inequalities in health when privileged groups benefit from interventions more than disadvantaged ones do.Footnote 6 According to a rapid overview of systematic reviews by Lorenc et al. (2013), downstream preventive interventions (media campaigns on smoking, and workplace smoking bans) seemed to be more likely to increase health inequalities than upstream interventions (structural workplace interventions; provision of resources; and fiscal interventions, such as tobacco pricing). Similarly, in a recent systematic review by McGill et al. (2015), they found that price interventions (upstream) to promote healthy eating are more effective among socioeconomically disadvantaged groups than are person-specific interventions (downstream), which were more effective among higher socioeconomic groups. Similar conclusions on the equity effect of interventions were made from systematic reviews on interventions tackling obesity (Beauchamp et al. 2014) or smoking (Hill et al. 2014).
The application of specific welfare programs (social policy, healthcare and public health) are an adequate answer to the use of welfare regime typologies, which are rather unspecific when it comes to explaining health and inequalities in health. Although the application of the institutional approach is very complex and broad, it overcomes the strong theoretical and methodological amendments that are necessary when applying welfare regime typologies. The focus on specific policies allows more precise conclusions to be drawn about their role in affecting the health of different socioeconomic groups. The evidence on social policies indicates that generous benefits are associated with better health, and with lower inequalities in health, whereas empirical findings on the effect of the healthcare system on inequalities in health are rather small and inconclusive. The same is true for the role of public health interventions, which is also a very broad and complex topic with mixed findings for different settings, risks behaviors, and health outcomes.
4 New Developments in Theorizing the Association Between Welfare States and Inequalities in Health
In theorizing the association between welfare state arrangements and inequalities in health, new explanatory approaches have emerged that consider the complex structure and processes linking different welfare policies to health and inequalities in health (Hurrelmann et al. 2011; Beckfield et al. 2015; Gkiouleka et al. 2018). These approaches take into account multiple levels, the specificity of diseases and social groups, and the interdependence of welfare state arrangements in their effect on the health of different social groups. Therefore, these approaches overcome the abovementioned linear logic in the relationship between welfare state arrangements, socioeconomic conditions and health, and the narrowed focus on distal variables on a high level of aggregation (Hurrelmann et al. 2011).
Beckfield et al. (2015) present an institutional theory of the welfare state that simultaneously considers welfare state effects of redistribution, compression and mediation on health and its social determinants. Accordingly, inequalities in health are a function of the institutional welfare effects of redistribution (institutional arrangements which redistribute the social determinants of health such as income, wealth, living standards or education), compression (institutional arrangements providing a limit of healthcare for citizens), and mediation (reducing/limiting inequalities in the social determinants of health such as income or education). These institutional effects of welfare state arrangements on health and its social determinants could interact and operate in multiple domains and at multiple levels (‘institutional imbrications’). They might also overlap and interact, and could have a direct effect on health, but could also indirectly influence health via the socioeconomic living conditions. For example, the distribution of health within a society can be influenced directly through healthcare institutions (healthcare and public health), and indirectly through institutional effects on the social determinants of health such as on income via economic assistance and unemployment benefits (social policy). Importantly, Beckfield et al. (2015) emphasize that the specific effects of institutions need to consider knowledge obtained from disease etiology, life course research, and (historical) institutional changes, which assigns individuals with a specific disease to a specific welfare state life course (Halfon and Hochstein 2002; Bambra et al. 2010; Levecque et al. 2011). The institutional effects of healthcare should thus be restricted to avoidable diseases that can be avoided through optimal-quality healthcare.Footnote 7 When considering the multiple and complex mechanisms of welfare arrangements on health and its social determinants, they also suggested considering resources and barriers on the individual (e. g. knowledge with regard to taking up welfare state benefits) and social levels (e. g. stigmatization of welfare recipients) that enable specific social groups to benefit from welfare arrangements, or hinder them from doing so.
In addition, Hurrelmann et al. (2011) proposed a comprehensive model to explain the association between welfare state regimes and inequalities in health, based on the previous work of Navarro et al. (2006) and Esping-Andersen (1990). This model considers a structural (macro), organizational (meso) and individual (micro) level. On the macro-level, the architecture of welfare policy is characterized by the dominance of market, civil networks or state, egalitarianism in civil and human rights, universalism in the provision of social services for citizens, and the level of decommodification. The meso-level is directly influenced by the architecture of welfare policy, and mediates the relationship between the macro and individual levels. It is characterized by several factors such as economic inequality, levels and availability of educational and occupational training, social integration and cohesion, degree of political participation, cultural integration of migrants, religious tolerance, criminality and antisocial behaviors, sense of control of social environment, availability of good food and water, and shelter from environmental contaminants. On the micro-level, the health status of individuals and populations is located and characterized by the quality of the objective and subjective well-being of the entire population, the health quality of disadvantaged and vulnerable groups, and levels of health inequality. Furthermore, Hurrelmann et al. (2011) take into account an intermediate entity that represents general welfare policy (public policy) and healthcare, as well as their combination and where they overlap. The specific characteristics of welfare state and healthcare policies are determined by the type of welfare regimes, and could have both a direct and an indirect effect on health by shaping healthcare institutions and organizations, as well as by influencing individuals’ social determinants of health.
5 Methodological Considerations in Research into the Role Played by Welfare State Characteristics for Health and Inequalities in Health
The empirical evaluation of the role of welfare state characteristics for health and inequalities in health is associated with several methodological and theoretical shortcomings which restrict the comparability of the high number of existing studies in this field (Bergqvist et al. 2013). Accordingly, we observed strong variations in the contextual levels, statistical methods, health outcomes and indicators of socioeconomic status in existing studies (detailed information about the reviewed articles can be found in the Appendix Tables). Although a large number of studies have been published so far, there still is a lack of sufficient data making it possible to empirically unravel the role of the welfare state and welfare state arrangements for the individual health of different socioeconomic groups.
This insufficiency of data availability is in particular observable in ecological studies (Navarro and Shi 2001; Navarro et al. 2003; Bambra 2006; Kangas 2010; Karim et al. 2010; Granados 2010; Regidor et al. 2011). Almost all existing ecological studies relied on data from the OECD, UN or WHO, which are restricted to a specific set of countries and health outcomes such as life expectancy or (infant) mortality. For example, most ecological studies relied on data from the OECD, which is currently one of the best data sources for this kind of study. Having said that, and similar to the field of psychology drawing most samples from Western, Industrialized, Rich, and Democratic (WEIRD) societies with the critical assumption that members of WEIRD societies are representative populations (Henrich et al. 2010), the generalizability of OECD-based studies in the field of public health should also be approached with caution.
Moreover, as most ecological studies rely on small sample sizes, results are often sensitive toward outliers (see also Goerres et al. 2019). For example, the US has been identified as a statistical outlier as many values, such as for healthcare expenditures, differ considerably from other societies (Lorenzoni et al. 2014). Chung and Muntaner (2006) discussed this issue extensively, and decided to include the US as these outlying values are not the result of any fault in the sampling process. However, the effect of outliers should not be underestimated when it comes to interpreting the results, as these can change dramatically if outliers are excluded from the analyses.Footnote 8 In addition, a small sample size in ecological studies increases the statistical relevance of single countries. For example, in the ecological study by Bambra (2006), analyzing the association between welfare state regime types and infant mortality, the liberal regime type was measured by only one country (UK), and the generalizability to other countries clustered into the liberal welfare regime type should therefore be made with caution.
Furthermore, the restrictions in the availability of adequate health outcomes result in theoretical amendments that are highly debatable (Bergqvist et al. 2013). For example, linking welfare regime types and infant mortality needs strong theoretical presumptions with regard to the mechanisms on the individual level, which most studies do not sufficiently present. However, even with the existence of good theoretical justifications, ecological studies are subject to a fundamental problem: the ecological bias. The ecological bias describes an information loss in the aggregation process that reduces information and prevents associations of interest being identified in the underlying individual-level model (Wakefield 2008). In terms of health inequality research, average levels are not able to provide information on health and its socioeconomic determinants on the individual level, as these aggregate measures mask part of the range of inequality present in the population (Murray et al. 1999). Therefore, critical reviewers might perceive these ecological studies as rather data driven, not taking into account adequate theoretical justifications, confounding factors, and the possibility of an ecological bias.
Although the application of multilevel analyses in ecological studies allows one to control for confounding factors to a certain extent (Chung and Muntaner 2007), ecological studies are still faced by the problem of strong theoretical presumptions when it comes to explaining how welfare regimes might influence the health of certain social groups. Therefore, the consideration of individual-level data that make it possible to empirically model the association between indicators of socioeconomic status and health by welfare regime types and facets has been conducted by several studies. These studies were most often based on individual-level data taken from the European Sociological Survey (ESS), the European Union Statistics on Income and Living Conditions (EU-SILC), the World Health Survey (WHS), the Survey of Health, Ageing and Retirement in Europe (SHARE) for Elderly (aged 50+), and the Health Behaviour in School-aged Children (HBSC) for adolescents (aged 11–15 years).
A first type of studies using individual-level data rather descriptively compares inequalities in health by welfare regime types, without controlling for the within-country correlation of observations and other important determinants of health on the contextual level, which increase the risks of biased standard errors (‘pooled regression studies’) (Zambon et al. 2006; Eikemo et al. 2008a, 2008c; Bambra et al. 2009, 2010; Guarnizo-Herreño et al. 2013, 2014; Alvarez-Galvez et al. 2014; Bambra and Eikemo 2009; Moortel et al. 2015). An exemplary study has been published by Eikemo et al. (2008a). They analyzed income-related inequalities in self-reported health with individual-level data of the ESS from 2004. Individual-level data of countries were pooled by regime types, and income-related inequalities in health (odds ratios) were descriptively compared between regime types. Although the authors highlighted the problem of the within-country correlation of observations, and applied sensitivity analyses by means of multilevel analysis, the final models were conducted without controlling for within-county correlation and, therefore, the results should be interpreted with caution. Moreover, these kinds of studies are unable to empirically quantify differences between welfare regime types in the association of socioeconomic status with individual health, and are unable to control for important control factors on the contextual level.
Therefore, multilevel analysis was conducted by novel studies identified as a second type of studies using individual-level data and the welfare regime type approachFootnote 9 (Eikemo et al. 2008b; Dragano et al. 2011; Richter et al. 2012; van der Wel et al. 2012; Witvliet et al. 2012; Chung et al. 2013; van de Velde et al. 2014; Niedzwiedz et al. 2014a, 2014b, 2015; Rathmann et al. 2015; Alvarez-Galvez 2016; Leão et al. 2018). Although the application of a multilevel approach overcomes the abovementioned methodological shortages, other general methodological issues do arise. The application of multilevel analyses is based on strong assumptions that are most often not discussed in studies from the field of public health or epidemiology. For example, it is assumed that errors on the macro level are normally distributed, are independent across contexts and are not correlated with individual-level errors (Diez-Roux 2000). This implies that the countries that are under consideration in the data were selected at random, which is most often not the case. For example, the EU-SILC predominantly considered EU Member States, and countries are therefore closely related to each other, thus violating the assumption of independency in multilevel analyses. Bryan and Jenkins (2016) discussed a further problem that arises in most multilevel studies. They argue that the small number of countries in most ‘multicountry data sets’ limits the ability to detect robust country (cross-level) effects, such as of welfare regime types or other institutional characteristics (see also Schmidt-Catran et al. 2019). These methodological problems should be at least considered when conducting multilevel analyses with data sets which have a small sample size on the contextual level.Footnote 10
Furthermore, analyses based on individual-level data relied most often on self-reported health. A very large number of studies in this field have focused on self-rated health and/or chronic illness. Although self-reported health indicators have been shown to be valid and reliable indicators for mortality (Benyamini 2011; Lima-Costa et al. 2012), research indicates that also social, psychosocial, and survey measurement factors are associated with respondents’ self-rated health responses (also described as Measurement Invariance, Reporting Heterogeneity or Different Item Functioning) (Garbarski 2016; see also Cieciuch et al. 2019). A similar issue is true for the measurement and understanding of indicators of socioeconomic status in cross-national research, such as for educational attainment in adult cross-country surveys (Schneider 2010), or for family affluence in cross-country surveys among adolescents (Makransky et al. 2014).
The lack of adequate data is a fundamental problem of the interdisciplinary research into the role of welfare characteristics for health and inequalities in health. For individual-level data, we observe a general inconsistency in the availability of adequate data sources that include objective health measures and data from social sciences. Most analyses in this context stem from social science data that do no not include objective health data for several reasons such as a lack of financial, personal or structural resources to survey such measures. In contrast, epidemiological data most frequently include objective health measures, but contain insufficient information on the socioeconomic living contexts of respondents. Against this background, the cross-national SHARE data are innovative as they provide both socioeconomic background information, and subjective and objective health measures from a number of countries. This allows one to analyze associations between welfare state policies/regimes and inequalities in subjective and objective health. Romaniuk (2014) analyzed differences in socioeconomic inequalities in subjective (self-rated health) and objective health (handgrip strength) from a welfare state regime perspective, including 16 countries from SHARE. Results of multilevel analyses suggested only weak variation for good self-rated health (4.7%) and for normal/strong hand grip strength (0.8%) across countries. Socioeconomic inequality in objective health and its association with welfare regime types were lower compared to subjective health, which might be related to cultural differences in answering questions on self-rated health. However, this is the first known study focusing on differences in socioeconomic inequalities in objective and subjective health by welfare regime types, and is associated with the abovementioned methodological shortages such as a low number of observations on the country level.
These methodological shortages must be acknowledged when interpreting and comparing study results relating to the role of welfare characteristics for health and inequalities in health. In particular, ecological studies and pooled regression studies suffer from severe methodological limitations when attempting to explain and empirically unravel the association between welfare characteristics, population health, and the health of specific social groups. Although the application of advanced methods such as multilevel analysis is more accurate for proofing the specific theoretical assumptions on the influence of welfare characteristics on individuals’ health, they are nonetheless faced by methodological issues that need to be considered when interpreting study results such as the limited number of countries on the contextual level or the lack of adequate health data.
6 Discussion
In the explanation of between- and within-country differences in health, theories from medical sociology (including areas from public health research, epidemiology, political economy of health and health services research) offer new insights into the causes of the causes of health inequalities: the welfare state. The welfare state has been identified as a relevant macro-level determinant of health that shapes individuals’ lives and health chances through healthcare, social policy and public health (Thomson et al. 2016). Several approaches have been proposed with a view to linking welfare state characteristics with health and inequalities in health.
According to the regime approach, the welfare state shapes population health and inequalities in health by mediating market-derived socioeconomic inequalities in individuals’ life chances via welfare services. It has been assumed that more generous welfare state regime types such as the Scandinavian regime type show better population health and have the smallest inequalities in health compared to all other regime types (liberal, conservative, southern or eastern regime type) (Eikemo et al. 2008b). However, the evidence does not consistently show smaller inequalities in health in the Scandinavian regime type. Given this Scandinavian puzzle (Mackenbach 2012; Bambra 2011), and the general critique of aggregating countries into different regime types (Lundberg 2008; Hurrelmann et al. 2011) by distal variables, an institutional approach has been developed. Accordingly, empirical research focused on the influence of specific welfare institutions (social policy, healthcare and public health) on the health of specific vulnerable groups. The evidence has shown a beneficial effect of family benefits, pension benefits and economic assistance and unemployment benefits for the health of vulnerable groups.Footnote 11 Moreover, research discussed the importance of access to healthcare and public health interventions, and found that universal access to healthcare and upstream public health interventions are associated with lower inequalities in health.
As both approaches lack a strong theoretical foundation on how welfare states’ policies are historically established and intertwined, influenced and determined by political, economic and social dynamics, and are most often not able to explain the extent and social distribution of specific diseases, new complex theoretical approaches have emerged. The innovative approaches of Beckfield et al. (2015) and Hurrelmann et al. (2011) combine the influence of different welfare state and public health interventions in one approach, and describe their interconnectedness and simultaneous influence on health and the social determinants of health. Moreover, they also take into account different contextual levels in the explanation of the influence of welfare state characteristics on health and inequalities in health, and focus on the influence of healthcare on amendable diseases.
These complex approaches might be interpreted as a further step into the theoretical foundation on how the welfare state—including social policy, healthcare and public health—is responsible for shaping and constraining population health, and the extent of social inequalities in health.Footnote 12 Further theoretical debates should explore how to include factors such as life course transitions (Bambra et al. 2010), gender (Bambra et al. 2009), migration (Castañeda et al. 2015), adolescence, and later life (Rathmann et al. 2015; Richter et al. 2012; Dahl and Birkelund 1997). Moreover, as most welfare approaches on health and health inequalities focus on income-relevant issues, there is still a need to take into account the impact had by welfare policies on other relevant determinants of health such as the education system (Allmendinger and Leibfried 2016; Rathmann et al. 2016) or the labor market (Muntaner et al. 2010; Julià et al. 2017) for inequalities in health by educational status, occupation or employment status. However, we need to acknowledge that these approaches are empirically tested and proposed only for developed (Western) countries, and therefore the generalizability to other countries such as in Asia, South America or Africa is limited, and needs to be addressed by further theoretical debates (Karim et al. 2010; Chung et al. 2013; Ng et al. 2016).
Finally, the empirical verification of mechanisms linking welfare state characteristics with the health of specific social groups requires advanced methods. Looking back into history in this field of research, a development in the application of methods is visible. Most studies initially relied on aggregate data and conducted rather descriptive and bivariate analyses. These ecological and pooled regression studies have been replaced by conducting advanced studies that allow one to explicitly model associations between different contextual levels or over time. In particular, the application of multilevel analysis has become popular, as it allows one to empirically meet the requirements from theory by modeling the association of welfare state characteristics on the contextual level with the health of different socioeconomic groups on the individual level. By doing so, research has shown that the welfare regime and the generosity of social benefits matters for inequalities in health and with regard to socioeconomically disadvantaged groups. Moreover, they also highlighted the strong theoretical and methodological amendments of past studies that were not able to conduct multilevel analyses, and also point to the general issue in this field of research: the limited availability of adequate data and the theoretical shortages. To further improve this field of research, the interdisciplinary work between scholars from public health, epidemiology, political economy of health, and health services research needs to be intensified and supported by scholars from sociology, political science, and psychology.
Notes
The validity of Wilkinson’s inequality-hypothesis is still highly debated (Lynch et al. 2004; Macinko et al. 2003; Maio 2012; Pickett and Wilkinson 2015; Subramanian and Kawachi 2004; Wilkinson and Pickett 2007), and more sophisticated studies indicate that the relationship between income inequality and health at the individual level is at least small or inconsistent (Leigh et al. 2011). In particular, social epidemiologists doubt that there is a context effect of income inequality on individual health, and emphasize the need for better data and methods (Leigh et al. 2011; Subramanian and Kawachi 2004).
Clustering the Antipodean countries (e. g. Australia and New Zealand) into the liberal regime type has been criticized due to a more particular and a more inclusive approach to social protection than the standard liberal form (Arts and Gelissen 2002).
Other welfare state typologies cluster the Scandinavian countries (Norway, Finland, Sweden and Denmark) into a single “Scandinavian” regime type (Leibfried 1992; Ferrera 1996; Bonoli 1997) to emphasize their exceptional universalistic and generous welfare regimes aiming to provide full employment and social equality.
According to Levin (2003, p. 108), an ecological study is “an observational study defined by the level at which data are analyzed, namely at the population or group level, rather than individual level.”
In 1975, John McKinlay (1979) introduced the terms upstream and downstream when describing his frustration with medical practice. In his analogy of a river that represents diseases, he said that physicians are so busy constantly rescuing victims from the river that they have no time to look upstream to check who is pushing their patients into the river. Instead, health professionals face challenges with downstream endeavors that are short-term, problem-specific and individual-based.
According to the inverse equity hypothesis of Victora et al. (2000), which is related to Rogers’ theory of diffusion (2005), when new public health interventions are implemented, higher socioeconomic groups will initially benefit, and health inequities will widen, but if coverage increases over time, the disadvantaged groups can eventually catch up and health inequities can be decreased.
To capture the contribution of healthcare to population health, the American Working Group on Preventable and Manageable Diseases introduced the concept of amendable mortality, which refers to deaths that could have been avoided by providing effective medical care in good time. In contrast, preventable (causes of) mortality refers to deaths that could have been avoided through timely and effective public health interventions (Nolte and McKee 2004).
Therefore, in the study by Chung and Muntaner (2006) that relies on time-series data from 19 wealthy OECD countries for the years from 1960 to 1994, analyses were conducted with and without the US to detect possible outlier effects.
The institutional approach is subject to similar methodological shortages when it comes to the application of individual-level data, ecological data or multilevel data analyses. However, studies using an institutional approach are superior to studies using the typology approach as they allow one to analyze the association and causal influence of specific welfare programs on specific health outcomes of certain social groups. The application of the institutional approach is still in its infancy, and various studies have been published so far that differ in their methodological and theoretical settings. This diversity complicates the interpretation and comparison of findings from these studies, and further research needs a stronger theoretical justification with regard to how specific welfare programs influence the health of specific social groups.
Bryan and Jenkins (2016) suggest considering at least 25 countries for linear models and at least 30 countries for logit models in order to derive accurate estimates. However, they also add that this rule of thumb should not be applied blindly but on the basis of the model that is being estimated and the effects in which the researcher is primarily interested. Complicated models that include multiple country-level or cross-level effects should include more countries in order to obtain unbiased and accurate effects.
According to Bergqvist et al. (2013), an alternative approach (expenditure approach) focuses on the influence of welfare state spending (social and health spending) on health and inequalities in health. According to their review, welfare state spending contributes to a specific level of spending on health, and is beneficial in terms of bringing about lower levels of inequalities in health.
A project on Health inequalities in European welfare states (HiNEWS) (2015–2018) that is currently underway focuses on the determinants of inequalities in health in European welfare states, the refinement, testing and development of social inequalities in health theory, the identification of policies and interventions with the potential of reducing health inequalities, and a new policy agenda on how health inequalities can be reduced most effectively.
References
Aitken, Zoe, Cameryn C. Garrett, Belinda Hewitt, Louise Keogh, Jane S. Hocking and Anne M. Kavanagh. 2015. The maternal health outcomes of paid maternity leave: a systematic review. Social Science and Medicine 130:32–41.
Allmendinger, Jutta, and Stephan Leibfried. 2016. Education and the welfare state: the four worlds of competence production. Journal of European Social Policy 13:63–81.
Alvarez-Galvez, Javier. 2016. Discovering complex interrelationships between socioeconomic status and health in Europe. A case study applying Bayesian Networks. Social Science Research 56:133–143.
Alvarez-Galvez, Javier, Maria L. Rodero-Cosano, Carlos García-Alonso and Luis Salvador-Carulla. 2014. Changes in socioeconomic determinants of health. Comparing the effect of social and economic indicators through European welfare state regimes. Journal of Public Health 22:305–311.
Arts, Will, and John Gelissen. 2002. Three worlds of welfare capitalism or more? A state-of-the-art report. Journal of European Social Policy 12:137–158.
Arts, Will, and John Gelissen. 2010. Models of the Welfare State. In The Oxford Handbook of the Welfare State, eds. Francis G. Castles, Stephan Leibfried, Jane Lewis, Herbert Obinger and Christopher Pierson, p. 569-583. Oxford: Oxford University Press.
Bambra, Clare. 2005a. Cash versus services. Worlds of welfare and the decommodification of cash benefits and health care services. Journal of Social Policy 34:195–213.
Bambra, Clare. 2005b. Worlds of welfare and the health care discrepancy. Social Policy and Society 4:31–41.
Bambra, Clare. 2006. Health status and the worlds of welfare. Social Policy and Society 5:53.
Bambra, C. 2007. Going beyond The three worlds of welfare capitalism: Regime theory and public health research. Journal of Epidemiology and Community Health 61:1098–1102.
Bambra, Clare. 2011. Health inequalities and welfare state regimes: Theoretical insights on a public health ‘puzzle’. Journal of Epidemiology and Community Health 65:740–745.
Bambra, C., and T. A. Eikemo. 2009. Welfare state regimes, unemployment and health. A comparative study of the relationship between unemployment and self-reported health in 23 European countries. Journal of Epidemiology and Community Health 63:92–98.
Bambra, Clare, Gopalakrishnan Netuveli and Terje A. Eikemo. 2010. Welfare state regime life courses: The development of western European welfare state regimes and age-related patterns of educational inequalities in self-reported health. International Journal of Health Services 40:399–420.
Bambra, C., D. Pope, V. Swami, D. Stanistreet, A. Roskam, A. Kunst and A. Scott-Samuel. 2009. Gender, health inequalities and welfare state regimes: a cross-national study of 13 European countries. Journal of Epidemiology and Community Health 63:38–44.
Banks, James, Michael Marmot, Zoe Oldfield and James P. Smith. 2006. Disease and disadvantage in the United States and in England. JAMA 295:2037–2045.
Beauchamp, A., K. Backholer, D. Magliano and A. Peeters. 2014. The effect of obesity prevention interventions according to socioeconomic position. A systematic review. Obesity Reviews 15:541–554.
Beckfield, Jason, and Nancy Krieger. 2009. Epi + demos + cracy: linking political systems and priorities to the magnitude of health inequities—evidence, gaps, and a research agenda. Epidemiologic Reviews 31:152–177.
Beckfield, Jason, Clare Bambra, Terje A. Eikemo, Tim Huijts, Courtney McNamara and Claus Wendt. 2015. An institutional theory of welfare state effects on the distribution of population health. Social Theory and Health 13:227–244.
Benyamini, Yael. 2011. Why does self-rated health predict mortality? An update on current knowledge and a research agenda for psychologists. Psychology and Health 26:1407–1413.
Bergqvist, Kersti, Monica A. Yngwe and Olle Lundberg. 2013. Understanding the role of welfare state characteristics for health and inequalities—an analytical review. BMC Public Health 13:1234.
Bonoli, Giuliano. 1997. Classifying welfare states. A two-dimension approach. Journal of Social Policy 26:351–372.
Braveman, Paula, and Laura Gottlieb. 2014. The social determinants of health: It’s time to consider the causes of the causes. Public Health Reports 129:19–31.
Braveman, Paula, Susan Egerter and David R. Williams. 2011. The social determinants of health: Coming of age. Annual Review of Public Health 32:381–398.
Brennenstuhl, Sarah, Amélie Quesnel-Vallée and Peggy McDonough. 2012. Welfare regimes, population health and health inequalities: A research synthesis. Journal of Epidemiology and Community Health 66:397–409.
Bryan, Mark L., and Stephen P. Jenkins. 2016. Multilevel modelling of country effects. A cautionary tale. European Sociological Review 32:3–22.
Castañeda, Heide, Seth M. Holmes, Daniel S. Madrigal, Maria-Elena D. Young, Naomi Beyeler and James Quesada. 2015. Immigration as a social determinant of health. Annual Review of Public Health 36:375–392.
Chung, Haejoo, and Carles Muntaner. 2006. Political and welfare state determinants of infant and child health indicators. An analysis of wealthy countries. Social Science and Medicine 63:829–842.
Chung, Haejoo, and Carles Muntaner. 2007. Welfare state matters: A typological multilevel analysis of wealthy countries. Health Policy 80:328–339.
Chung, Haejoo, Edwin Ng, Selahadin Ibrahim, Björn Karlsson, Joan Benach, Albert Espelt and Carles Muntaner. 2013. Welfare state regimes, gender, and depression: A multilevel analysis of middle and high income countries. International Journal of Environmental Research and Public Health 10:1324–1341.
Cieciuch, Jan, Eldad Davidov, Peter Schmidt and René Algesheimer. 2019. How to obtain comparable measures for cross-national comparisons. In Cross-national comparative research – analytical strategies, results and explanations. Sonderheft Kölner Zeitschrift für Soziologie und Sozialpsychologie. Eds. Hans-Jürgen Andreß, Detlef Fetchenhauer and Heiner Meulemann. Wiesbaden: Springer VS. https://doi.org/10.1007/s11577-019-00598-7.
Coburn, David. 2000. Income inequality, social cohesion and the health status of populations. The role of neo-liberalism. Social Science and Medicine 51:135–146.
Cylus, Jonathan, Maria Glymour and Mauricio Avendano. 2015. Health effects of unemployment benefit program generosity. American Journal of Public Health 105:317–323.
Dahl, Espen, and Gunn E. Birkelund. 1997. Health inequalities in later life in a social democratic welfare state. Social Science and Medicine 44:871–881.
Davis, Karen. 1991. Inequality and access to health care. The Milbank Quarterly 69:253.
Diez-Roux, A. V. 2000. Multilevel analysis in public health research. Annual Review of Public Health 21:171–192.
Dragano, Nico, Johannes Siegrist and Morten Wahrendorf. 2011. Welfare regimes, labour policies and unhealthy psychosocial working conditions. A comparative study with 9917 older employees from 12 European countries. Journal of Epidemiology and Community Health 65:793–799.
Eikemo, T. A., and C. Bambra. 2008. The welfare state: A glossary for public health. Journal of Epidemiology and Community Health 62:3–6.
Eikemo, T. A., C. Bambra, K. Joyce and Espen Dahl. 2008a. Welfare state regimes and income-related health inequalities. A comparison of 23 European countries. European Journal of Public Health 18:593–599.
Eikemo, Terje A., Clare Bambra, Ken Judge and Kristen Ringdal. 2008b. Welfare state regimes and differences in self-perceived health in Europe: A multilevel analysis. Social Science and Medicine 66:2281–2295.
Eikemo, Terje A., Martijn Huisman, Clare Bambra and Anton E. Kunst. 2008c. Health inequalities according to educational level in different welfare regimes. A comparison of 23 European countries. Sociology of Health and Illness 30:565–582.
Elo, Irma T. 2009. Social class differentials in health and mortality. Patterns and explanations in comparative perspective. Annual Review of Sociology 35:553–572.
Esping-Andersen, Gosta. 1990. The three worlds of welfare capitalism. London: Polity Press.
Esser, Ingrid, and Joakim Palme. 2010. Do public pensions matter for health and wellbeing among retired persons? Basic and income security pensions across 13 Western European countries. International Journal of Social Welfare 19:S103–S120.
Farrants, Kristin. 2017. Recommodification and the social determinants of health. Unemployment benefits, pensions and health inequalities in Sweden and England, 1991–2011. Journal of Public Health 39:661–667.
Fenger, H. J. Menno. 2007. Welfare regimes in Central and Eastern Europe: Incorporating post-communist countries in a welfare regime typology. Contemporary Issues and Ideas in Social Sciences 3:1–30.
Ferrera, Maurizio. 1996. The ‘Southern Model’ of welfare in social Europe. Journal of European Social Policy 6:17–37.
Galobardes, Bruna, Mary Shaw, Debbie A. Lawlor, John W. Lynch and George Davey Smith. 2006. Indicators of socioeconomic position (part 1). Journal of Epidemiology and Community Health 60:7–12.
Garbarski, Dana. 2016. Research in and prospects for the measurement of health using self-rated health. Public Opinion Quarterly 80:977–997.
Gkiouleka, Anna, Tim Huijts, Jason Beckfield and Clare Bambra. 2018. Understanding the micro and macro politics of health. Inequalities, intersectionality & institutions—A research agenda. Social Science and Medicine 200:92–98.
Goerres, Achim, Markus B. Siewert and Claudius Wagemann. 2019. Internationally comparative research designs in the social sciences: Fundamental issues, case selection logics, and research limitations. In Cross-national comparative research – analytical strategies, results and explanations. Sonderheft Kölner Zeitschrift für Soziologie und Sozialpsychologie. Eds. Hans-Jürgen Andreß, Detlef Fetchenhauer and Heiner Meulemann. Wiesbaden: Springer VS. https://doi.org/10.1007/s11577-019-00600-2.
Granados, José A. T. 2010. Politics and health in eight European countries. A comparative study of mortality decline under social democracies and right-wing governments. Social Science and Medicine 71:841–850.
Gravelle, H. 1998. How much of the relation between population mortality and unequal distribution of income is a statistical artefact? British Medical Journal 316:382–385.
Guarnizo-Herreño, Carol C., Richard G. Watt, Hynek Pikhart, Aubrey Sheiham and Georgios Tsakos. 2013. Socioeconomic inequalities in oral health in different European welfare state regimes. Journal of Epidemiology and Community Health 67:728–735.
Guarnizo-Herreño, Carol C., Richard G. Watt, Hynek Pikhart, Aubrey Sheiham and Georgios Tsakos. 2014. Inequalities in oral impacts and welfare regimes. Analysis of 21 European countries. Community Dentistry and Oral Epidemiology 42:517–525.
Halfon, Neal, and Miles Hochstein. 2002. Life course health development. An integrated framework for developing health, policy, and research. The Milbank Quarterly 80:433–479.
Hamad, Rita, and David H. Rehkopf. 2016. Poverty and child development: A longitudinal study of the impact of the earned income tax credit. American Journal of Epidemiology 183:775–784.
Hank, Karsten, and Anja Steinbach. 2019. Families and their institutional contexts: The role of family policies and legal regulations. In Cross-national comparative research – analytical strategies, results and explanations. Sonderheft Kölner Zeitschrift für Soziologie und Sozialpsychologie. Eds. Hans-Jürgen Andreß, Detlef Fetchenhauer and Heiner Meulemann. Wiesbaden: Springer VS. https://doi.org/10.1007/s11577-019-00603-z.
Henrich, Joseph, Steven J. Heine and Ara Norenzayan. 2010. Most people are not WEIRD. Nature 466:29.
Hill, Sarah, Amanda Amos, David Clifford and Stephen Platt. 2014. Impact of tobacco control interventions on socioeconomic inequalities in smoking. Review of the evidence. Tobacco Control 23:e89–97.
Huber, J., and A. Mielck. 2010. Morbidität und Gesundheitsversorgung bei GKV- und PKV-Versicherten. Forschungsstand empirischer Studien (Comparing statutory and private health insurance in terms of morbidity and healthcare. A stocktake of empirical research). Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz 53:925–938.
Hurrelmann, Klaus, Katharina Rathmann and Matthias Richter. 2011. Health inequalities and welfare state regimes. A research note. Journal of Public Health 19:3–13.
Jen, Min H., Kelvyn Jones and Ron Johnston. 2009. Compositional and contextual approaches to the study of health behaviour and outcomes: Using multi-level modelling to evaluate Wilkinson’s income inequality hypothesis. Health and Place 15:198–203.
Jones, Koolman, and van Doorslaer. 2006. The impact of having supplementary private health insurance on the use of specialists. Annales d’Économie et de Statistique 83/84:251–275.
Julià, Mireia, Laia Ollé-Espluga, Christophe Vanroelen, Deborah de Moortel, Sarah Mousaid, Stig Vinberg, Vanessa Puig-Barrachina, Esther Sánchez, Carles Muntaner, Lucía Artazcoz and Joan Benach. 2017. Employment and labor market results of the SOPHIE project: Concepts, analyses, and policies. International Journal of Health Services 47:18–39.
Kangas, Olli. 2010. One hundred years of money, welfare and death. Mortality, economic growth and the development of the welfare state in 17 OECD countries 1900–2000. International Journal of Social Welfare 19:S42–S59.
Karim, Syahirah A., Terje A. Eikemo and Clare Bambra. 2010. Welfare state regimes and population health: integrating the East Asian welfare states. Health Policy 94:45–53.
Klein, Jens, Kerstin Hofreuter-Gätgens, Daniel Lüdecke, Margit Fisch, Markus Graefen and von dem Knesebeck, Olaf. 2016. Socioeconomic status and health-related quality of life among patients with prostate cancer 6 months after radical prostatectomy: A longitudinal analysis. BMJ Open 6:e010968.
Larrimore, Jeff. 2011. Does a higher income have positive health effects? Using the earned income tax credit to explore the income-health gradient. The Milbank Quarterly 89:694–727.
Leibfried, Stephan. 1992. Towards a European Welfare State? On integrating poverty regimes into the European community. In Social policy in a changing world, eds. Zsuzsa Ferge and Jon E. Kolberg, pp. 245–279. Frankfurt a. M.: Campus.
Leigh, Andrew, Christopher Jencks and Smeeding, Timothy M. 2011. Health and economic inequality. In The Oxford handbook of economic inequality, eds. Brian Nolan, Wiemer Salverda and Timothy M. Smeeding, pp. 384–404. Oxford: Oxford University Press.
Levecque, Katia, Ronan van Rossem, Katrien de Boyser, Sarah van de Velde and Piet Bracke. 2011. Economic hardship and depression across the life course: The impact of welfare state regimes. Journal of Health and Social Behavior 52:262–276.
Levin, Kate A. 2003. Study design VI—Ecological studies. Evidence-based dentistry 7:108.
Leão, Teresa, Inês Campos-Matos, Clare Bambra, Giuliano Russo and Julian Perelman. 2018. Welfare states, the Great Recession and health. Trends in educational inequalities in self-reported health in 26 European countries. PloS one 13:e0193165.
Lima-Costa, Maria F., Cibele C. Cesar, Dora Chor and Fernando A. Proietti. 2012. Self-rated health compared with objectively measured health status as a tool for mortality risk screening in older adults: 10-year follow-up of the Bambuí Cohort Study of Aging. American Journal of Epidemiology 175:228–235.
Link, Bruce G., and Jo Phelan. 1995. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior extra issue, 80–94.
Lorenc, Theo, and Kathryn Oliver. 2014. Adverse effects of public health interventions. A conceptual framework. Journal of Epidemiology and Community Health 68:288–290.
Lorenc, Theo, Mark Petticrew, Vivian Welch and Peter Tugwell. 2013. What types of interventions generate inequalities? Evidence from systematic reviews. Journal of Epidemiology and Community Health 67:190–193.
Lorenzoni, Luca, Annalisa Belloni and Franco Sassi. 2014. Health-care expenditure and health policy in the USA versus other high-spending OECD countries. The Lancet 384:83–92.
Lundberg, Olle. 2008. Commentary: Politics and public health—some conceptual considerations concerning welfare state characteristics and public health outcomes. International Journal of Epidemiology 37:1105–1108.
Lynch, John, George D. Smith, Sam Harper, Marianne Hillemeier, Ross, Nancy, Kaplan, George A and Michael Wolfson. 2004. Is income inequality a determinant of population health? Part 1. A Systematic Review. The Milbank Quarterly 82:5–99.
Macinko, James A., Leiyu Shi, Barbara Starfield and John T. Wulu. 2003. Income inequality and health: A critical review of the literature. Medical Care Research and Review 60:407–452.
Mackenbach, Johan P. 2012. The persistence of health inequalities in modern welfare states: The explanation of a paradox. Social Science and Medicine 75:761–769.
Maio, Fernando de. 2012. Advancing the income inequality—health hypothesis. Critical Public Health 22:39–46.
Makransky, Guido, Christina W. Schnohr, Torbjørn Torsheim and Candace Currie. 2014. Equating the HBSC Family Affluence Scale across survey years. A method to account for item parameter drift using the Rasch model. Quality of Life Research 23:2899–2907.
Marmot, Michael, and Jessica J. Allen. 2014. Social determinants of health equity. American Journal of Public Health 104 Suppl 4:S517–9.
McGill, Rory, Elspeth Anwar, Lois Orton, Helen Bromley, Ffion Lloyd-Williams, Martin O’Flaherty, David Taylor-Robinson, Maria Guzman-Castillo, Duncan Gillespie, Patricia Moreira, Kirk Allen, Lirije Hyseni, Nicola Calder, Mark Petticrew, Martin White, Margaret Whitehead and Simon Capewell. 2015. Are interventions to promote healthy eating equally effective for all? Systematic review of socioeconomic inequalities in impact. BMC Public Health 15:457.
McKinlay, James. 1979. A case for refocusing upstream: The political economy of illness. In Patients, physicians and illness: A sourcebook in behavioral science and health, ed. J. Gartley, pp. 9–25. New York: Free Press.
Moor, Irene, Jacob Spallek and Matthias Richter. 2017. Explaining socioeconomic inequalities in self-rated health: A systematic review of the relative contribution of material, psychosocial and behavioural factors. Journal of Epidemiology and Community Health 71:565–575.
Moortel, Deborah de, Laia Palència, Lucía Artazcoz, Carme Borrell and Christophe Vanroelen. 2015. Neo-Marxian social class inequalities in the mental well-being of employed men and women. The role of European welfare regimes. Social Science and Medicine 128:188–200.
Muntaner, Carles, Joan Benach, Haejoo Chung, N. G. Edwin and Ted Schrecker. 2010. Welfare state, labour market inequalities and health. In a global context: An integrated framework. SESPAS report 2010. Gaceta sanitaria 24 Suppl 1:56–61.
Muntaner, Carles, Carme Borrell, Edwin Ng, Haejoo Chung, Albert Espelt, Maica Rodriguez-Sanz, Joan Benach and Patricia O’Campo. 2011. Politics, welfare regimes, and population health: Controversies and evidence. Sociology of Health and Illness 33:946–964.
Murray, Christopher J.L., Gakidou, Emmanuela, E. and Julio Frenk. 1999. Health Inequalities and Social Group Differences: What Should We Measure? Bulletin of the World Health Organization 77:537–543.
Navarro, Vicente. 1999. The political economy of the welfare state in developed capitalist countries. International Journal of Health Services 29:1–50.
Navarro, Vicente, and Leiyu Shi. 2001. The political context of social inequalities in health. International Journal of Health Services 31:1–21.
Navarro, Vicente, Carme Borrell, Joan Benach, Carles Muntaner, Agueda Quiroga, Maica Rodríguez-Sanz, Nuria Vergés, Jordi Gumá and M. I. Pasarín. 2003. The importance of the political and the social in explaining mortality differentials among the countries of the OECD, 1950–1998. International Journal of Health Services 33:419–494.
Navarro, Vicente, Carles Muntaner, Carme Borrell, Joan Benach, Águeda Quiroga, Maica Rodríguez-Sanz, Núria Vergés and M. I. Pasarín. 2006. Politics and health outcomes. The Lancet 368:1033–1037.
Ng, Edwin, Carles Muntaner and Haejoo Chung. 2016. Welfare states, labor markets, political dynamics, and population health: A time-series cross-sectional analysis among East and Southeast Asian nations. Asia-Pacific Journal of Public Health 28:219–231.
Niedzwiedz, Claire L., Srinivasa V. Katikireddi, Jill P. Pell and Richard Mitchell. 2014a. Socioeconomic inequalities in the quality of life of older Europeans in different welfare regimes. European Journal of Public Health 24:364–370.
Niedzwiedz, Claire L., Srinivasa V. Katikireddi, Jill P. Pell and Richard Mitchell. 2014b. The association between life course socioeconomic position and life satisfaction in different welfare states. European comparative study of individuals in early old age. Age and Ageing 43:431–436.
Niedzwiedz, Claire L., Jill P. Pell and Richard Mitchell. 2015. The relationship between financial distress and life-course socioeconomic inequalities in well-being. Cross-national analysis of European welfare states. American Journal of Public Health 105:2090–2098.
Nolte, Ellen, and McKee, Martin. 2004. Does health care save lives? Avoidable mortality revisited. London: Nuffield Trust.
Norström, Thor, and Joakim Palme. 2010. Public pension institutions and old-age mortality in a comparative perspective. International Journal of Social Welfare 19:S121–S130.
O’Campo, Patricia, Agnes Molnar, Edwin Ng, Emilie Renahy, Christiane Mitchell, Ketan Shankardass, Alexander St John, Clare Bambra and Carles Muntaner. 2015. Social welfare matters: A realist review of when, how, and why unemployment insurance impacts poverty and health. Social Science and Medicine 132:88–94.
Oliver, Adam, and Elias Mossialos. 2004. Equity of access to health care. Outlining the foundations for action. Journal of Epidemiology and Community Health 58:655–658.
Or, Zeynep, Florence Jusot and Yilmaz, Engin. 2008. Impact of health care system on socioeconomic inequalities in doctor use. IRDES Working Paper No 17.
Pega, Frank, Kristie Carter, Ichiro Kawachi, Peter Davis, Fiona I. Gunasekara, Olle Lundberg and Tony Blakely. 2013. The impact of in-work tax credit for families on self-rated health in adults: A cohort study of 6,900 New Zealanders. Journal of Epidemiology and Community Health 67:682–688.
Pega, Frank, Kristie Carter, Ichiro Kawachi, Peter Davis and Tony Blakely. 2014. The impact of an unconditional tax credit for families on self-rated health in adults: Further evidence from the cohort study of 6,900 New Zealanders. Social Science and Medicine 108:115–119.
Pega, Frank, Tony Blakely, Maria M. Glymour, Kristie N. Carter and Ichiro Kawachi. 2016. Using marginal structural modeling to estimate the cumulative impact of an unconditional tax credit on self-rated health. American Journal of Epidemiology 183:315–324.
Pfaff, Holger, and Timo-Kolja Pförtner. 2016. Der Beitrag der Versorgungsforschung zur Chancengerechtigkeit in der Gesundheit und in der Versorgung. (The contribution made by healthcare research to equal opportunities in health and healthcare) Das Gesundheitswesen 78:91–96.
Phelan, Jo C., Bruce G. Link and Parisa Tehranifar. 2010. Social conditions as fundamental causes of health inequalities: Theory, evidence, and policy implications. Journal of Health and Social Behavior 51:28–40.
Pickett, Kate E., and Richard G. Wilkinson. 2015. Income inequality and health: A causal review. Social Science and Medicine 128:316–326.
Rathmann, Katharina, Irene Moor, Anton E. Kunst, Nico Dragano, Timo-Kolja Pförtner, Frank J. Elgar, Klaus Hurrelmann, Lasse Kannas, Tibor Baška and Matthias Richter. 2016. Is educational differentiation associated with smoking and smoking inequalities in adolescence? A multilevel analysis across 27 European and North American countries. Sociology of Health and Illness 38:1005–1025.
Rathmann, Katharina, Veronika Ottova, Klaus Hurrelmann, Margarethe de Looze, Kate Levin, Michal Molcho, Frank Elgar, Saoirse N. Gabhainn, van Dijk, Jitse P and Matthias Richter. 2015. Macro-level determinants of young people’s subjective health and health inequalities: A multilevel analysis in 27 welfare states. Maturitas 80:414–420.
Reeves, Aaron, Martin McKee, Johan Mackenbach, Margaret Whitehead and David Stuckler. 2017. Public pensions and unmet medical need among older people. Cross-national analysis of 16 European countries, 2004–2010. Journal of Epidemiology and Community Health 71:174–180.
Regidor, Enrique, Cruz Pascual, David Martínez, María E. Calle, Paloma Ortega and Paloma Astasio. 2011. The role of political and welfare state characteristics in infant mortality. A comparative study in wealthy countries since the late 19th century. International Journal of Epidemiology 40:1187–1195.
Richter, Matthias, Katharina Rathman, Saoirse Nic Gabhainn, Alessio Zambon, William Boyce and Klaus Hurrelmann. 2012. Welfare state regimes, health and health inequalities in adolescence: A multilevel study in 32 countries. Sociology of Health and Illness 34:858–879.
Rodgers, Gerry B. 1979. Income and inequality as determinants of mortality: An international cross-section analysis. Population Studies 33:343–351.
Rogers, Everett M. 2005. Diffusion of innovations. 5th ed. New York: Free Press.
Romaniuk, Joanna. 2014. Subjective and objective health of the population aged 50+ and the welfare state regimes in 16 European countries. International Journal of Management and Economics 39:82–107.
Saint-Arnaud, Sébastien, and Paul Bernard. 2003. Convergence or resilience? A hierarchical cluster analysis of the welfare regimes in advanced countries. Current Sociology 51:499–527.
Schmidt-Catran, Alexander W., Malcolm Fairbrother and Hans-Jürgen Andreß. 2019. Multilevel models for the analysis of comparative survey data: Common problems and some solutions. In Cross-national comparative research – analytical strategies, results and explanations. Sonderheft Kölner Zeitschrift für Soziologie und Sozialpsychologie. Eds. Hans-Jürgen Andreß, Detlef Fetchenhauer and Heiner Meulemann. Wiesbaden: Springer VS. https://doi.org/10.1007/s11577-019-00607-9.
Schneider, Silke L. 2010. Nominal comparability is not enough. (In-)equivalence of construct validity of cross-national measures of educational attainment in the European Social Survey. Research in Social Stratification and Mobility 28:343–357.
Schröder, Martin. 2019. Varieties of capitalism and welfare regime theories: Assumptions, accomplishments, and the need for different Methods. In Cross-national comparative research – analytical strategies, results and explanations. Sonderheft Kölner Zeitschrift für Soziologie und Sozialpsychologie. Eds. Hans-Jürgen Andreß, Detlef Fetchenhauer and Heiner Meulemann. Wiesbaden: Springer VS. https://doi.org/10.1007/s11577-019-00609-7.
Strully, Kate W., David H. Rehkopf and Ziming Xuan. 2010. Effects of prenatal poverty on infant health. State earned income tax credits and birth weight. American Sociological Review 75:534–562.
Subramanian, S. V., and Ichiro Kawachi. 2004. Income inequality and health: What have we learned so far? Epidemiologic Reviews 26:78–91.
Thomson, Katie, Clare Bambra, Courtney McNamara, Tim Huijts and Adam Todd. 2016. The effects of public health policies on population health and health inequalities in European welfare states: Protocol for an umbrella review. Systematic Reviews 5:57.
Vahid Shahidi, Faraz, Arjumand Siddiqi and Carles Muntaner. 2016. Does social policy moderate the impact of unemployment on health? A multilevel analysis of 23 welfare states. European Journal of Public Health 26:1017–1022.
van de Velde, Sarah, Clare Bambra, Koen van der Bracht, Terje A. Eikemo and Piet Bracke. 2014. Keeping it in the family. The self-rated health of lone mothers in different European welfare regimes. Sociology of Health and Illness 36:1220–1242.
Victora, Cesar G., J. Patrick Vaughan, Fernando C. Barros, Anamaria C. Silva and Elaine Tomasi. 2000. Explaining trends in inequities. Evidence from Brazilian child health studies. The Lancet 356:1093–1098.
Wakefield, Jonathan. 2008. Ecologic studies revisited. Annual Review of Public Health 29:75–90.
van der Wel, Kjetil A., Espen Dahl and Karsten Thielen. 2012. Social inequalities in “sickness”. Does welfare state regime type make a difference? A multilevel analysis of men and women in 26 European countries. International Journal of Health Services 42:235–255.
Wicks-Lim, Jeannette, and Peter S. Arno. 2017. Improving population health by reducing poverty. New York’s earned income tax credit. SSM—Population Health 3:373–381.
Wilkinson, Richard G. 1990. Income distribution and mortality. A ‘natural’ experiment. Sociology of Health and Illness 12:391–412.
Wilkinson, Richard G., and Pickett, Kate. 2011. Spirit level. Why equality is better for everyone. London: Penguin Books Ltd.
Wilkinson, Richard G., and Kate E. Pickett. 2007. The problems of relative deprivation: Why some societies do better than others. Social Science and Medicine 65:1965–1978.
Witvliet, Margot I., Anton E. Kunst, Karien Stronks and Onyebuchi A. Arah. 2012. Assessing where vulnerable groups fare worst. A global multilevel analysis on the impact of welfare regimes on disability across different socioeconomic groups. Journal of Epidemiology and Community Health 66:775–781.
Woolf, Steven H., and Paula Braveman. 2011. Where health disparities begin: The role of social and economic determinants—and why current policies may make matters worse. Health Affairs 30:1852–1859.
Zambon, Alessio, Will Boyce, Ester Cois, Candace Currie, Patrizia Lemma, Paola Dalmasso, Alberto Borraccino and Franco Cavallo. 2006. Do welfare regimes mediate the effect of socioeconomic position on health in adolescence? A cross-national comparison in Europe, North America, and Israel. International Journal of Health Services 36:309–329.
Author information
Authors and Affiliations
Corresponding author
Additional information
Online Appendix: www.kzfss.uni-koeln.de/sites/kzfss/pdf/pfoertner_et_al.pdf.
Rights and permissions
About this article
Cite this article
Pförtner, TK., Pfaff, H. & Elgar, F.J. The Role of Welfare State Characteristics for Health and Inequalities in Health from a Cross-National Perspective: A Critical Research Synthesis. Köln Z Soziol 71 (Suppl 1), 465–489 (2019). https://doi.org/10.1007/s11577-019-00606-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11577-019-00606-w
Keywords
- Social determinants of health
- Cross-national differences
- Welfare regime
- Social policy
- Public health
- Healthcare