Abstract
Aim
To assess the correlation of quantitative data of pulmonary Perfused Blood Volume (PBV) on Dual-Energy CT (DECT) datasets in patients with moderate – severe Pulmonary Emphysema (PE) with Lung Perfusion Scintigraphy (LPS) as the reference standard. The secondary endpoints are the correlation between the CT densitometric analysis and the visual assessment of parenchymal destruction with PBV.
Materials and Methods
Patients with moderate – severe PE candidate to Lung Volumetric Reduction (LVR), with available a pre-procedural LS and a contrast-enhanced DECT were retrospectively included. DECT studies were performed with a 3rd generation Dual-Source CT and the PBV was obtained with a 3-material decomposition algorithm. The CT densitometric analysis was performed with a dedicated commercial software (Pulmo3D). The Goddard Score was used for visual assessment. The perfusion LS were performed after the administration of albumin macroaggregates labeled with 99mTechnetium. The image revision was performed by two radiologists or nuclear medicine physicians blinded, respectively, to LS and DECT data. The statistical analysis was performed with nonparametric tests.
Results
Thirty-one patients (18 males, median age 69 y.o., interquartile range 62–71 y.o.) with moderate – severe PE (Median Goddard Score 14/20 and 31% of emphysematous parenchyma at quantitative CT) candidate to LVR were retrospectively included. The median enhancement on PBV was 17 HU. Significant correlation coefficients were demonstrated between lung PBV and LS, poor in apical regions (Rho = 0.1–0.2) and fair (Rho = 0.3–0.5) in middle and lower regions. No significant correlations were recorded between the CT densitometric analysis, the visual score, and the PBV.
Conclusions
Lung perfusion with PBV on DECT is feasible in patients with moderate – severe PE candidate to LVR, and has a poor to fair agreement with LPS.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pulmonary emphysema (PE) is defined as the abnormal permanent enlargement of airways distal to the terminal bronchiole with alveolar destruction, without any fibrosis, and it is included in chronic obstructive pulmonary disease (COPD) [1, 2]. PE is characterized by obstructive ventilatory defects, reduced diffusion capacity, and parenchymal destruction is also often associated with altered alveolar ventilation/perfusion ratio (V/Q) [3, 4]. Ventilatory and Perfusion functional parameters assessed at scintigraphy are altered when at least one-third of the lung parenchyma is involved, making them poorly sensitive [4, 5]. Moreover, alveolar destruction and hypoxic vasoconstriction reduce regional perfusion in the emphysematous lung [4]. However, the distribution of perfusion damage does not necessarily correlate with the area of parenchymal destruction [4, 6,7,8,9].
Patients with advanced PE, poorly controlled with medical treatment, may take benefit from endoscopic or surgical Lung Volume Reduction (LVR) [10, 11]. These procedures aim to reduce the size disproportion between the hyperinflate pulmonary parenchyma and the volume of the chest cavity, thus restoring the forces acting on the elastic recoil of the bronchiolar walls [12]. As consequences, these procedures lead to an improved bronchiolar airflow with a global beneficial effect on the cardiothoracic function and on physical exercise [12,13,14]. The early diagnosis, classification, and assessment of disease extension strongly relies on High-Resolution Computed Tomography (HRCT) [15,16,17]. However, the management of candidates for LVR must include the assessment of lung perfusion, since perfused parenchyma should be preserved, while the pulmonary portions with impaired perfusion need to be treated [6, 7, 18, 19].
The assessment of PE on HRCT may be performed with visual, semiquantitative scores (Visual Score, VS), or with automatic or semiautomatic software that quantifies the percentage of pathological parenchyma in each volume using densitometric thresholds and morphological changes [18, 20,21,22,23,24,25]. On the one side, VS usually has an easy application but is time-consuming and has a low intra- and inter-rater agreement [18, 20,21,22,23]. Conversely, semi-automatic software has the potential for a more objective quantification with lower variability [18, 24].
Several methods are available for the assessment of lung perfusion; among them, the Lung Perfusion Scintigraphy (LPS) is one of the most widely used [25]. LPS provides a two-dimensional compression of a volumetric distribution of a radiotracer and does not provide morphological information [6, 26]. Dual-Energy CT (DECT) with material decomposition allows for effective iodine quantification [27]. The application of a specific three-material decomposition algorithm for the lung parenchyma provides the Perfused Blood Volume (PBV), namely the perfused blood volume into a unit mass of lung tissue, which is translated to a whole-lung map to assess the parenchymal perfusion [28, 29]. The agreement of PBV and nuclear medicine studies, mostly with qualitative methods, has been more extensively evaluated in pulmonary embolism [29,30,31,32], while little evidence is available for PE [33].
This study aims to correlate the quantitative PBV with LPS parameters in patients with moderate to severe PE candidate to endoscopic LVR. Secondary endpoints are the correlation between the lung PBV and the densitometric analysis with the semiautomatic software, and the correlation between perfusion abnormalities at PBV with parenchymal destruction at VS.
Materials and methods
Patient selection
This study was conducted in accordance with the Declaration of Helsinki. In agreement with our local IRB, due to the data being registered anonymously and the study’s retrospective design, formal ethical approval by the IRB was not required.
Patients with moderate-severe PE, in evaluation for endoscopic LVR, with pulmonary angio-DECT imaging between February 2018 and March 2022, who underwent planar LPS within 15 days of the DECT at our Institution (Azienda Ospedaliero Universitaria delle Marche) were included. Patients with imaging of inadequate quality (i.e., pulmonary artery enhancement < 200 HU, motion artifacts, underlying pulmonary diseases such as consolidations or pulmonary embolism), or with incomplete imaging data (DECT or LPS data not available) were not included.
DECT acquisition protocol
CT examinations were performed using 3rd generation Dual Source DECT (Somatom Force, Siemens Healthineers). The basal acquisition was performed in deep inspiration and reconstructed with a medium and sharp kernel (120 kV, modulated mA, model-based iterative reconstruction, ADMIRE, strength 3, kernels Br40 and Bl64) with a slice thickness and spacing of 1 mm/0.7 mm [34, 35]. The study was completed with a DECT acquisition (90/150Sn, modulated mA, ADMIRE 3, reconstruction kernels Br40, BL64, and Qr40, thickness/spacing: 1/0.7 mm) after the administration of intravenous contrast material (Iopamidol 370 mgI/mL, Iopamiro 370, Bracco; 1 mL/kg, 3,5 – 5 ml/s); the acquisition time was optimized with bolus tracking technique (Threshold: 100 HU in pulmonary trunk; acquisition delay: 6 s).
CT visual analysis
Visual quantification of emphysema was performed with Goddard VS on HRCT basal images by two readers in consensus and blinded to LS (AA, AB, with 15 and 10 years of experience in thoracic imaging), after the quality control of the DECT study (i.e., adequate enhancement of the pulmonary artery) and exclusion of concomitant pulmonary diseases [20]. Both lungs were evaluated at three levels: upper, middle, and lower. The apical zone was examined at an axial scan passing 1 cm above the upper margin of the aortic arch; the middle lung was examined at an axial scan passing 1 cm below the tracheal carina; the basal lung was examined 3 cm above the diaphragmatic dome. A percentage score of emphysematous parenchyma was assigned at these zones, bilaterally. In particular, no evidence of emphysema: score 0; emphysematous areas less than 25%: score 1; between 26 and 50%: score 2; between 51 and 75%: score 3; greater than 75%: score 4. These scores were summed, and the total value was the severity score of PE. Conventionally, the three regions of the lung considered for the visual analysis, and for the further segmentation (see below), were labeled as left (L1, L2, L3) and right (R1, R2, R3) in cranio-caudal direction.
Densitometric analysis with semi-automatic software
Basal images reconstructed with medium kernel (Br40) were processed with semiautomatic software for densitometric analysis (Pulmo3D on Syngo.via, Siemens Healthineers) by the same radiologists blinded to LS [34, 35]. The software quantifies the percentage of voxels with attenuation values lower than the threshold of -950 HU for the entire pulmonary parenchyma, the right and left lungs separately and the lower, middle and upper zones of equal volume (Volume Based, VB) of each lung separately (R1-3; L1-3). The Mean Lung Densities (MLD) were also recorded for each patient.
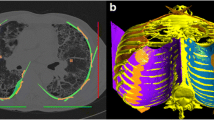
Calculation of PBV
The two radiologists in consensus and blinded to LS processed the post-contrast DECT datasets with dedicated three-material decomposition on DE Lung Analysis (Syngo.via, Siemens Healthineers) to calculate the lung PBV. Iodine distribution and PBV maps were rendered on axial, sagittal, and coronal planes and in 3D Volume Rendering (VR). The measurements were performed after normalization of iodine distribution on the Pulmonary artery enhancement: a standardized region of interest (ROI) sized 0.5 cm2 was placed in the pulmonary trunk on axial images. Lung partitioning was performed automatically using the Distance Based (DB) mode. The lungs were divided by two horizontal lines into three fields of equivalent cranio-caudal length: upper, middle, and lower (R1-3; L1-3). DB is a mode of lung segmentation more similar to that used in scintigraphy than the technique of VB segmentation used in densitometric analysis.
LPS acquisition, post-processing, and assessment
Perfusion Scintigraphy examinations were performed with γ-chamber Infinia (GE Healthcare). Eight standard planar projections (anterior, posterior, right lateral, left lateral, right posterior oblique, left posterior oblique, right anterior oblique, left anterior oblique) were acquired after intravenous administration of albumin macroaggregates labeled with 99mTechnetium (99mTc-MAA) [4]. The post-processing and image revision was performed with dedicated software by two nuclear medicine physicians in consensus and blinded to the DECT datasets (LB, AP, 30 and 10 years of experience respectively): each anterior and posterior digital planar scintigraphy projection of each lung was manually demarcated within a rectangular ROI which is semi-manually subdivided into three regions (upper, middle, lower) of approximately equivalent areas by two horizontal lines (R1-3; L1-3). The anteroposterior geometric mean of the detected counts was automatically calculated for all areas corresponding to anterior and posterior projections of each lung. The estimated lung perfusion was obtained in absolute k-count value for each lung field examined [26].
Statistical analysis
Statistical analysis of the data was performed on MedCalc Statistic Software (v20.211, MedCalc Software). All the quantitative variables were tested for normality (D’Agostino-Pearson test), and after the rejection of normal distribution, the variables were expressed as median values and interquartile ranges, and nonparametric tests were used. In particular, Wilcoxon or Friedman Tests were used when appropriate to assess differences among related samples, and correlation between DECT and LPS was evaluated with Rank Correlation (Spearman’s Rho), the values were interpreted, in absolute values, as perfect (1), very strong (0.8–0.9), moderate (0.6–0.7), fair (0.3–0.5), poor (0.1–0.2), and none (0) [36]. P values < 0.05 were considered significant.
Results
Fifty-five patients underwent to contrast-enhanced DECT study as treatment planning of LVR. Out of them, 5 had DECT studies of inadequate quality (3 patients with motion artifacts; 2 patients with inadequate enhancement of the pulmonary artery), and 19 had incomplete or inadequate imaging data (scintigraphy data not available). The final population included 31 patients with moderate-to-severe PE candidate to LVS. The median age was 69 years and 18 candidates were male, with a median Goddard VS of 14/24 (interquartile range 8–20).
Quantification of PE evaluated by Pulmo3D application of Syngo.via software had a median value of 31%, with a median value of mean lung density (MLD) of -903 HU. The median PBV value was obtained as an absolute value of 16.5 HU (Table 1).
Table 2 reports the semi—quantitative and quantitative findings for each lung region. Significant differences were recorded among median Goddard visual scores, CT densitometric parameters, and LS of the different regions (Friedman p < 0.05). No significant differences were recorded for PBV parameters across the different lung regions.
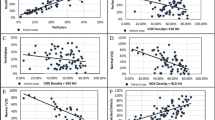
Regional PBV in absolute value (HU) in DB mode and perfusion values obtained by LPS in k-counts were correlated (Figs.1, 2). More in detail, a significant correlation was found between PBV values and k-count for each region of the right and left lungs (Spearman Rho ranging between 0.106 and 0.478).
Rank correlation (Spearman Rho) between PBV (HU) and lung Scintigraphy (kilo-count, kct). The figure reports the Spearman’s Rho coefficients, the relative 95% confidence intervals (95%CI) and the p-values. Significant correlations were found for the two methods for each region of the right (R1, R2, R3) and left lung (L1, L2, L3) regions. Significant p-values are underlined
Figure 3 reports the rank correlation (Spearman Rho) between the densitometric analysis with semi-automatic software (Pulmo 3D on Syngo.via) and lung PBV. In this case, a negative correlation trend was found between the extension of parenchymal destruction and perfusion; however, significant values were found only in the upper right region and lower left region.
Rank correlation (Spearman Rho) between PBV on DECT (HU) and densitometric analysis with semi-automatic software (pulmonary emphysema, PE, % value). The figure reports the Spearman’s Rho coefficients, the relative 95% confidence intervals (95%CI) and the p-values for each pulmonary region (L1, L2, L3, R1, R2, R3). A negative trend for correlation between the PBV and PE% was recorded, though significant only for right apical and left lower regions. Significant p-values are underlined
This statistical trend was confirmed by the correlation analysis between the Goddard VS and lung PBV (Fig. 4), where a significant, negative correlation was found only in the upper region of the right lung.
Rank correlation (Spearman Rho) between PBV on DECT (HU) and Goddard visual score (VS). The figure reports the Spearman’s Rho coefficients, the relative 95% confidence intervals (95%CI) and the p-values for each pulmonary region (L1, L2, L3, R1, R2, R3). Significant correlations were found only for the apical region of the right lung. Significant p-values are underlined
Discussion
This study aims to compare the quantitative assessment if lung perfusion on DECT (the lung PBV) with quantitative data of LPS: we found statistically significant, poor to fair correlation between the two techniques, with slightly higher correlation coefficients in middle and basal regions of right and left lungs (Fig. 2). Regarding the secondary endpoint, the correlation between pulmonary perfusion assessed with lung PBV and parenchymal destruction by PE, assessed with the Goddard semiquantitative score and with a dedicated, semi-automatic software, were not significant with few exceptions in upper or lower pulmonary regions (Figs. 3, 4).
These results deserve some considerations. In our study, both the software for the post-processing of DECT and scintigraphy data divided the lungs in three regions: fair, significant concordance was demonstrated for the middle and lower regions, while only a poor concordance was recorded in the apical regions. This finding can be explained by accounting several aspects. First, while the Lung PBV for DECT analysis uses an automatic method for the division in cranio-caudal equally distant regions (DB mode), the same method is semi-automatic for LPS, introducing a variability source. Second, the calculation of PBV use a three-material decomposition, where the spectral curves of air and lung are included for the calculation of the distribution of iodine. It has been demonstrated that the accuracy of iodine quantification can be influenced by variation of the effective atomic number and electron density given by pathological conditions (i.e., pulmonary consolidations) [28]. It could be hypothesized that different grades of parenchymal destruction in PE may slightly but significantly affect the estimation of PBV in PE. Moreover, the post processing of DECT datasets is prone to beam-hardening artifacts, which can be more significant in regions close to the superior vena cava and in paracardiac parenchyma [37].
While the radionuclide perfusion and ventilation examinations have an established role in the management of COPD and PE, the iodine spectral analysis on DECT is still under investigation [26, 33, 38]. On the one side, perfusion scintigraphy is based on the intravenous administration of 99mTechnetium—labeled albumin macroaggregates (99mTcMAA) which causes a microembolization of the pulmonary circulation resolving in 6–8 h, and the γ-rays emitted are detected by the γ-chamber [26]. On the other side, the assessment of pulmonary perfusion with DECT is derived from the iodine density map during the first pass of the contrast material in the pulmonary microcirculation [28]. The specific software for PBV is based on three-material decomposition to produce material-specific images from air, soft tissue, and iodine. After thresholding for the selection of the pulmonary parenchyma, the iodine density is superimposed to the virtual non-contrast images [39, 40]. Several studies assessed the diagnostic performance of Lung perfusion with DECT, particularly in patients with pulmonary thromboembolism (PTE). Sueyoshi et al. demonstrated significant different lung perfusion in patients with and without PTE [41]. These results were confirmed by Sakamoto et al. in patients with acute PTE of different grades of severity [39]. Dournes et al. compared the diagnostic performance of DECT with lung scintigraphy in patients with chronic thromboembolic pulmonary hypertension demonstrating a fair agreement (k = 0.44) between the two methods [30]. Renapurkar et al. performed the comparison between DECT and SPECT on a similar population of patients with chronic pulmonary hypertension, recording a lower inter-method agreement of k = 0.22–0.25 [42]. Regarding pulmonary emphysema, Gietema et al. compared the lung perfusion from DECT with scintigraphy, finding a good correlation between the two techniques [33]. These results were confirmed by Si-Mohamed et al. comparing the lung perfusion on DCT and SPECT/CT in PE [43]. However, the assessment of parenchymal involvement at HRCT nor the correlation with PBV were not performed in both studies [33, 43].
Even though the treatment planning of LVR mainly relies on the HRCT assessment of emphysema, the LPS still have a pivotal role by highlighting eventual mismatch of ventilation and perfusion in PE. It must be highlighted that lung PBV is a volumetric technique, while scintigraphy provides planar information [26]. This aspect is of clinical relevance, since the PBV on DECT provides more detailed spatial information than LPS. Moreover, the perfusion data of PBV can be superimposed, pixel by pixel, to the morphological information provided by the HRCT, thus giving the potential to DECT of being a one-stop-shop examination for the treatment planning of LVR in PE [26, 33].
Our data show a lack of concordance between the degree of parenchymal destruction and the hypoperfusion of the relative areas, confirming the previous studies [21]. However, it must be highlighted that also in this case the different segmentation techniques (volume-based for densitometric analysis and DB for the PBV) can be a source of variability of results. This trend was confirmed when the parenchyma destruction with VS was compared with the regional, PBV data, confirming the additional information provided by the perfusion assessment in addition to parenchymal destruction [6,7,8, 18, 19, 21].
The present study has several limitations. It is a retrospective, single-center study on a small cohort of patients with moderate-severe PE assessed with one DECT platform: the reproducibility of results should be assessed on different DECT platforms and in patients with different disease severity.
In conclusion, the calculation of PBV demonstrated a moderate correlation with scintigraphy data, with no significant correlation with the degree of parenchymal destruction assessed with semiautomatic software and VS in patients with moderate – severe PE candidate do LVR.
References
Christenson SA, Smith BM, Bafadhel M, Putcha N (2022) Chronic obstructive pulmonary disease. Lancet 399:2227–2242. https://doi.org/10.1016/s0140-6736(22)00470-6
Cottin V, Nunes H, Brillet P-Y et al (2005) Combined pulmonary fibrosis and emphysema: a distinct underrecognised entity. Eur Respir J 26:586–593. https://doi.org/10.1183/09031936.05.00021005
Janssen R, Piscaer I, Franssen FME, Wouters EFM (2019) Emphysema: looking beyond alpha-1 antitrypsin deficiency. Expert Rev Respir Med 13:381–397. https://doi.org/10.1080/17476348.2019.1580575
Sandek K, Bratel T, Lagerstrand L, ROSELL H, (2002) Relationship between lung function, ventilation–perfusion inequality and extent of emphysema as assessed by high-resolution computed tomography. Respir Med 96:934–943. https://doi.org/10.1053/rmed.2002.1371
Smith BM, Austin JHM, Newell JD et al (2014) Pulmonary emphysema subtypes on computed tomography: the MESA COPD study. Am J Med 127:94.e7-94.e23. https://doi.org/10.1016/j.amjmed.2013.09.020
Thuheer R, Engel H, Weder W et al (2012) Role of lung perfusion scintigraphy in relation to chest computed tomography and pulmonary function in the evaluation of candidates for lung volume reduction surgery. Am J Respir Crit Care Med 159:301–310. https://doi.org/10.1164/ajrccm.159.1.9711030
Chandra D, Lipson DA, Hoffman EA et al (2010) Perfusion scintigraphy and patient selection for lung volume reduction surgery. Am J Respir Crit Care Med 182:937–946. https://doi.org/10.1164/rccm.201001-0043oc
Suga K, Kawakami Y, Iwanaga H et al (2008) Assessment of anatomic relation between pulmonary perfusion and morphology in pulmonary emphysema with breath-hold SPECT-CT fusion images. Ann Nucl Med 22:339. https://doi.org/10.1007/s12149-007-0137-5
Suga K, Okada M, Kunihiro M et al (2011) Impaired Lung 123I-MIBG Uptake on SPECT in pulmonary emphysema. J Nucl Med 52:1378–1384. https://doi.org/10.2967/jnumed.111.090076
Pompeo E, Elkhouly A, Rogliani P et al (2021) Quasilobar minimalist lung volume reduction surgery. Eur J Cardio-Thorac Surg 60:598–606. https://doi.org/10.1093/ejcts/ezab174
Hartman JE, Welling JBA, Klooster K et al (2022) Survival in COPD patients treated with bronchoscopic lung volume reduction. Respir Med 196:106825. https://doi.org/10.1016/j.rmed.2022.106825
Lenga P, Ruwwe-Glösenkamp C, Grah C et al (2021) Endoscopic lung volume reduction with endobronchial valves in very low DLCO patients: results from the German Registry – Lungenemphysemregister e.V. ERJ Open Res 7:00449–02020. https://doi.org/10.1183/23120541.00449-2020
Martinez FJ, de Oca MM, Whyte RI et al (1997) Lung-volume reduction improves dyspnea, dynamic hyperinflation, and respiratory muscle function. Am J Respir Crit Care Med 155:1984–1990. https://doi.org/10.1164/ajrccm.155.6.9196106
Blondeel A, Demeyer H, Ceulemans LJ et al (2022) The impact of endoscopic lung volume reduction on physical activity coaching in patients with severe emphysema. ERJ Open Res 8:00150–02022. https://doi.org/10.1183/23120541.00150-2022
Lynch DA, Austin JHM, Hogg JC et al (2015) CT-definable subtypes of chronic obstructive pulmonary disease: a statement of the fleischner society. Radiology 277:192–205. https://doi.org/10.1148/radiol.2015141579
Lynch DA, Al-Qaisi MA (2013) Quantitative computed tomography in chronic obstructive pulmonary disease. J Thorac Imaging 28:284–290. https://doi.org/10.1097/rti.0b013e318298733c
Silva M, Picozzi G, Sverzellati N et al (2022) Low-dose CT for lung cancer screening: position paper from the Italian college of thoracic radiology. Radiol Med (Torino) 127:543–559. https://doi.org/10.1007/s11547-022-01471-y
Martini K, Frauenfelder T (2018) Emphysema and lung volume reduction: the role of radiology. J Thorac Dis 1:S2719–S2731
Criner GJ, Cordova F, Sternberg AL, Martinez FJ (2011) the national emphysema treatment trial (NETT). Am J Respir Crit Care Med 184:881–893. https://doi.org/10.1164/rccm.201103-0455ci
Goddard PR, Nicholson EM, Laszlo G, Watt I (1982) Computed tomography in pulmonary emphysema. Clin Radiol 33:379–387. https://doi.org/10.1016/s0009-9260(82)80301-2
Mascalchi M, Diciotti S, Sverzellati N et al (2011) Low agreement of visual rating for detailed quantification of pulmonary emphysema in whole-lung CT. Acta Radiol 53:53–60. https://doi.org/10.1258/ar.2011.110419
Sverzellati N, Devaraj A, Desai SR et al (2011) Method for minimizing observer variation for the quantitation of high-resolution computed tomographic signs of lung disease. J Comput Assist Tomogr 35:596–601. https://doi.org/10.1097/rct.0b013e3182277d05
Kim YS, Kim EY, Ahn HK et al (2016) Prognostic significance of CT-emphysema score in patients with advanced squamous cell lung cancer. J Thorac Dis 8:1966–1973
Newell JD, Sieren J, Hoffman EA (2013) Development of quantitative computed tomography lung protocols. J Thorac Imaging 28:266–271. https://doi.org/10.1097/rti.0b013e31829f6796
Martini K, Frauenfelder T (2020) Advances in imaging for lung emphysema. Ann Transl Medicine 8:1467–1467
Mortensen J, Berg RMG (2019) Lung Scintigraphy in COPD. Semin Nucl Med 49:16–21. https://doi.org/10.1053/j.semnuclmed.2018.10.010
Agostini A, Borgheresi A, Mari A et al (2019) Dual-energy CT: theoretical principles and clinical applications. Radiol Med 124:1281–1295. https://doi.org/10.1007/s11547-019-01107-8
Li K, Li Y, Qi Z et al (2021) Quantitative lung perfusion blood volume (PBV) using dual energy CT (DECT)-based effective atomic number (Zeff) imaging. Med Phys. https://doi.org/10.1002/mp.15227
Thieme SF, Becker CR, Hacker M et al (2008) Dual energy CT for the assessment of lung perfusion—correlation to scintigraphy. Eur J Radiol 68:369–374. https://doi.org/10.1016/j.ejrad.2008.07.031
Dournes G, Verdier D, Montaudon M et al (2014) Dual-energy CT perfusion and angiography in chronic thromboembolic pulmonary hypertension: diagnostic accuracy and concordance with radionuclide scintigraphy. Eur Radiol 24:42–51. https://doi.org/10.1007/s00330-013-2975-y
Thieme SF, Graute V, Nikolaou K et al (2012) Dual energy CT lung perfusion imaging—correlation with SPECT/CT. Eur J Radiol 81:360–365. https://doi.org/10.1016/j.ejrad.2010.11.037
Yang G-F, Yang X, Zhang L-J et al (2011) Pulmonary enhancement imaging with dual energy ct for the detection of pulmonary embolism in a rabbit model comparison to perfusion planar scintigraphy, SPECT and SPECT-CT modalities. Acad Radiol 18:605–614. https://doi.org/10.1016/j.acra.2010.12.012
Gietema HA, Walraven KHM, Posthuma R et al (2021) Dual-energy computed tomography compared to lung perfusion scintigraphy to assess pulmonary perfusion in patients screened for endoscopic lung volume reduction. Respiration 100:1–10. https://doi.org/10.1159/000517598
Gierada DS, Bierhals AJ, Choong CK et al (2010) Effects of CT section thickness and reconstruction kernel on emphysema quantification relationship to the magnitude of the CT emphysema index. Acad Radiol 17:146–156. https://doi.org/10.1016/j.acra.2009.08.007
Rodriguez A, Ranallo FN, Judy PF, Fain SB (2017) The effects of iterative reconstruction and kernel selection on quantitative computed tomography measures of lung density. Med Phys 44:2267–2280. https://doi.org/10.1002/mp.12255
Akoglu H (2018) User’s guide to correlation coefficients. Turkish J Emerg Medicine 18:91–93. https://doi.org/10.1016/j.tjem.2018.08.001
Parakh A, An C, Lennartz S et al (2021) Recognizing and minimizing artifacts at dual-energy CT. Radiographics. https://doi.org/10.1148/rg.2021200049
Herth FJF, Slebos D-J, Criner GJ et al (2019) Endoscopic lung volume reduction: an expert panel recommendation – update 2019. Respiration 97:548–557. https://doi.org/10.1159/000496122
Sakamoto A, Sakamoto I, Nagayama H et al (2014) Quantification of lung perfusion blood volume with dual-energy ct: assessment of the severity of acute pulmonary thromboembolism. Am J Roentgenol 203:287–291. https://doi.org/10.2214/ajr.13.11586
Thieme SF, Hoegl S, Nikolaou K et al (2010) Pulmonary ventilation and perfusion imaging with dual-energy CT. Eur Radiol 20:2882–2889. https://doi.org/10.1007/s00330-010-1866-8
Sueyoshi E, Tsutsui S, Hayashida T et al (2011) Quantification of lung perfusion blood volume (lung PBV) by dual-energy CT in patients with and without pulmonary embolism: preliminary results. Eur J Radiol 80:e505–e509. https://doi.org/10.1016/j.ejrad.2010.10.011
Renapurkar RD, Bolen MA, Shrikanthan S et al (2018) Comparative assessment of qualitative and quantitative perfusion with dual-energy CT and planar and SPECT-CT V/Q scanning in patients with chronic thromboembolic pulmonary hypertension. Cardiovasc Diagnosis Ther 8:414–422
Si-Mohamed S, Moreau-Triby C, Tylski P et al (2020) Head-to-head comparison of lung perfusion with dual-energy CT and SPECT-CT. Diagn Interv Imag 101:299–310. https://doi.org/10.1016/j.diii.2020.02.006
Funding
Open access funding provided by Università Politecnica delle Marche within the CRUI-CARE Agreement. The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation was performed by Myriam Badaloni, Andrea Palucci, and Luca Burroni. Data collection was performed by Alessandra Borgheresi, Sofia Balducci, Elisa Cesari, Elisabetta Tola, and Valeria Consoli. The statistical analysis was performed by Alessandra Borgheresi and Andrea Agostini. The first draft of the manuscript was written by Alessandra Borgheresi, Andrea Agostini, and Elisa Cesari. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical Approval
This is a retrospective, observational study. The Local Research Ethics Committee has confirmed that no formal ethical approval is required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Borgheresi, A., Cesari, E., Agostini, A. et al. Pulmonary emphysema: the assessment of lung perfusion with Dual-Energy CT and pulmonary scintigraphy. Radiol med (2024). https://doi.org/10.1007/s11547-024-01883-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11547-024-01883-y