Abstract
Purpose
To compare point shear wave elastography (pSWE, ElastPQ®) and transient elastography (TE) with Liver Biopsy in order to evaluate fibrosis stage in non-alcoholic fatty liver disease (NAFLD).
Methods
Our prospective study from September 2017 to October 2020 included 50 consecutively enrolled patients with NAFLD (52.2 ± 13.0 years, 32 male). All patients underwent clinical evaluation, B-mode ultrasound, pSWE, TE and liver biopsy in a single evaluation. The clinical, laboratory and liver biopsy data were compared with liver stiffness (LS) measurement obtained with pSWE and TE. TE and pSWE diagnostic accuracy for the diagnosis of the different fibrosis stages were evaluated using the area under receiver operating characteristic curve (AUROC).
Results
Only fibrosis stage was independently associated with TE and pSWE. The median liver stiffness measurement for fibrosis stages F0, F1, F2, F3, and F4 using TE was 4.8 (4.7–6.1) kPa, 5.5 (4.4–7.3) kPa, 7.7 (6.1–9.1) kPa, 9.9 (8.8–13.8) kPa, and 20.2 kPa, respectively. The corresponding median liver stiffness measurement using pSWE was 4.2 (4.0–4.8) kPa, 4.7 (4.2–5.8) kPa, 5.1 (4.1–6.9) kPa, 8.5 (5.2–13.3), and 15.1 kPa, respectively. The AUROC of TE for diagnosis of fibrosis stage F1, ≥ F2, ≥ F3, and F4 were 0.795, 0.867, 0.927, and 0.990, respectively. The corresponding AUROC of pSWE was 0.717, 0.733, 0.908, and 1.000, respectively. No association was observed with other histological parameters.
Conclusion
TE was significantly better than pSWE for the diagnosis of fibrosis stage ≥ F2. No statistically significant differences were found between TE and pSWE AUROC of fibrosis stage ≥ F1, ≥ F3, and F4.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Non-alcoholic fatty liver disease (NAFLD) is increasingly recognized as the most common form of chronic liver disease worldwide and is defined as the presence of 5% of hepatic steatosis (HS), in the absence of competing liver disease aetiologies, such as chronic viral hepatitis [1]. NAFLD is divided into two major subtypes: non-alcoholic fatty liver (NAFL, also termed simple steatosis), and NASH (non-alcoholic steatohepatitis), the progressive form of NAFLD that can lead to cirrhosis, hepatocellular carcinoma (HCC) and liver-related mortality that is characterized by the presence of steatosis, ballooning degeneration and lobular inflammation [2]. The most accurate estimation of the global prevalence of NAFLD is 24–25% of the general population, a figure reported for the first time in Italy by the Dionysos study [3] and recently confirmed by Younossi [1, 4]. Liver biopsy was typically performed in chronic liver disease with the aim to assess liver fibrosis, and it is required for the diagnosis of NASH. However, the invasiveness of the procedure entail risk for the patient [5, 6]. In patients with NAFLD is important to know the degree of liver disease, and surrogate markers of fibrosis (NFS, FIB-4, ELF or FibroTest) should be used for every patient, in order to rule out significant fibrosis (F ≥ 2).
If significant fibrosis cannot be ruled out with other methods, patients should be referred to a liver evaluation with transient elastography (TE) [7]. Several studies about TE were reported in NAFLD and NASH. Wong et al. compared TE with liver biopsy in 246 consecutive patients with NAFLD and revealed 91% sensitivity and 75% specificity for predicting severe fibrosis (F ≥ 3), using a cut-off value of 7.9 kPa [8]. A recently developed method for liver stiffness assessment is point Share Wave Elastography (pSWE). It is already standardized to use in other chronic liver disease [9, 10], although to date only few pSWE studied were performed in NAFLD and NASH [11, 12].
TE is used for liver stiffness measurement. An automated movement of a piston, which is also a disc-shaped ultrasound transducer, applies a single push to the body surface with controlled applied force. The transient shear deformation created in this way propagates into the tissue. Its near constant speed for about 4 cm in the liver is measured by a straight line automatically fitted to the displacement M-mode, obtained by processing the ultrasound radio frequency echo signal versus time, and then generating values in kPa. In pSWE method the shear-wave is generated using a probe and its arrival time at nearby A-lines is measured to provide the average shear-wave speed between two points bounded by a measurement region of interest (ROI). The speed can be measured to depths of about 8 cm and is reported in units of ms−1 or converted to Young’s modulus in kPa. Although ultrasound imaging is used to guide placement of the ROI, no elasticity images are produced [9].
Materials and methods
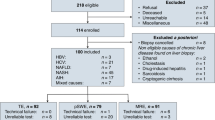
Between September 2017 and October 2020 50 adult patients with NAFLD diagnosis were prospectively enrolled in our hospital. Diagnosis of NAFLD was achieved on the basis of ultrasound fatty liver characteristics, and excluding all the other evaluable etiologies of chronic liver disease. HCV and HBV patient were excluded; patient’s informed consent was obtained. Each patient was evaluated with demographic, anthropometric, clinical and laboratory data, b-mode ultrasound, point Shear Wave Elastography, Transient Elastography, and then on the same day underwent liver biopsy. All patients were studied after fasting for at least 6 h.
Conventional ultrasonography (US) of the liver was performed to evaluate echogenicity of liver parenchyma. TE (Fibroscan Echosense® 402) was performed in fasting patient with M probe by a single operator (G S B) with over 10 years experience. A TE examination was recognized as adequate if there were ≥ 10 acceptable assessment and reliable if the interquartile range (IQR)/median for liver stiffness measurement was ≤ 30% or if the liver stiffness measurement was < 7.1 kPa when the IQR/median was > 30%. When less than ten acceptable evaluations were attained after 30 attempts an examination was regarded as unsuccessful. XL probe was used after failed evaluation with the M probe, and successful XL probe examinations were included in the analysis [13]. pSWE (ElastPQ® Philips healthcare Affinity® 70) measurements were performed by a single radiologist (G A) with over 10 years experience. In all patients, measurements were taken on the same day of TE and before liver biopsy. Patients were evaluated in the supine position, at least 1.5–2 cm beneath the right liver capsule in order to avoid reverberation artefact and away from the intrahepatic vessels and the gallbladder [14]. When the elasticity imaging mode was selected, the patient held the breath for 3–5 s. When the target area was located, the operator initiated the SWE sequence measurements. A rectangular quantitative sampling frame with a diameter of 10 mm was used to evaluate the region of interest. Mean speed values were calculated on the basis of 10 measurement and the software automatically calculated the median elastic modulus (Young’s modulus) in kPa within the region of interest [9]. For both methods the operators had an adequate training period respecting the learning curve. Ultrasound guided liver biopsy was performed using 18G BioPince™ (Argon Medical Devices, Athens, Texas, USA) and was analyzed by pathologists of our institute that were blinded to US. Liver biopsy was performed in the same segments of liver elastography assessment. The adequate liver specimen criteria were defined as follows: ≥ 20 mm in length and ≥ eight portal tracts [15]. Histopathological findings were reported according to the Non-Alcoholic Steatohepatitis Clinical Research Network Scoring System [16]. Steatosis, lobular inflammation, and ballooning with or without fibrosis defined NASH. Fibrosis stages were: F0 = no fibrosis, F1 = perisinusoidal fibrosis, F2 = perisinusoidal with portal/periportal fibrosis, F3 = bridging fibrosis, and F4 = cirrhosis.
Statistical analysis
Continuous and categorical variables were presented as mean ± standard deviation and as absolute figures, respectively. Univariate and multivariate linear regression analyses were performed in order to assess the existence of independent factors associated with TE and pSWE. The area under receiver operating characteristic curve (AUROC) using four sets of examinations was performed in order to assess diagnostic accuracy for TE and pSWE for the diagnosis of fibrosis stages. AUROC 0.90–1.00 was assesses as excellent, 0.80–0.90 good, 0.70–0.80 fair, and lower than 0.70 as poor. The liver stiffness value that yield the highest sum of sensitivity and specificity for the diagnosis of each specific fibrosis stage was assumed as the optimal cut-off. On the basis of this optimal cut-off for each specific fibrosis stage were evaluated sensitivity, specificity, positive predictive value, and negative predictive value of liver stiffness measurement for the diagnosis of that particular fibrosis stage. A p value < 0.05 was considered statically significant. All statistical analyses were performed using MedCalc Software v. 15.8 (Ostend, BEL).
Results
Patient characteristics and clinical and histological data are shown in Table 1.
Liver biopsy length and numbers of portal tracts were adequate in all patients.
Liver stiffness measurement according to fibrosis stages were the follows: the median liver stiffness measurement for fibrosis stages F0, F1, F2, F3, and F4 using TE was 4.8 (4.7–6.1) kPa, 5.5 (4.4–7.3) kPa, 7.7 (6.1–9.1) kPa, 9.9 (8.8–13.8) kPa, and 20.2 kPa, respectively. The corresponding median liver stiffness measurement using pSWE was 4.2 (4.0–4.8) kPa, 4.7 (4.2–5.8) kPa, 5.1 (4.1–6.9) kPa, 8.5 (5.2–13.3), and 15.1 kPa, respectively.
Accuracy of transient elastography and point shear wave elastography for the diagnosis of the different fibrosis stages were evaluated. The AUROC, optimal cut-off, sensitivity, specificity of TE and pSWE for the diagnosis of fibrosis stages ≥ F1 (p = 0.252), ≥ F2 (p = 0.035), ≥ F3 (p = 0.734), and F4 (p = 0.479) are shown in Table 2. All patients had pSWE measurements that were obtained with an IQR/M ≤ 30%. As regards transient elastography the XL probe was used in 17 (34%) patients.
A statistically significant difference between the two methods showed that TE was better than pSWE for the diagnosis of fibrosis stage ≥ F2. No statistically significant differences were found between TE and pSWE AUROC of fibrosis stage ≥ F1, ≥ F3, and F4.
The AUROC of TE and pSWE for the diagnosis of fibrosis stage ≥ F1 (Fig. 1), ≥ F2 (Fig. 2), ≥ F3 (Fig. 3), and F4 (Fig. 4) are shown.
Biochemical data about all patients were acquired, and no patient had ALT or AST > 5 times the upper limit of normal, but no associations were observed with other histological parameters.
Discussion
Liver biopsy is the gold standard for the diagnosis of NASH and is the only procedure that reliably differentiates NAFLD from NASH. The aims of non-invasive markers are: predict treatment response, identify severe NASH and monitor disease progression without complications of liver biopsy.
EASL–EASD–EASO Clinical Practice Guidelines recommends using TE as non-invasive method for identification of cases at low risk of advanced fibrosis/cirrhosis. There is no consensus about the use of TE in combination with biomarkers in order to evaluate patients who have high risk of advanced fibrosis/cirrhosis. Consequently, it is necessary to assess new methods, and pSWE is a promising tool [7].
In the management of patients with NAFLD is possible to avoid liver biopsy when surrogate markers (NFS, FIB-4, ELF or FibroTest) could rule out significant fibrosis (F ≥ 2). If significant fibrosis cannot be ruled out, patients should be referred to a liver clinic for TE study [7].
Furthermore, some studies suggest that non-invasive methods in patients suspected of having NAFLD can be used in order to select patients who may benefit from liver biopsy. In fact, patients with a liver stiffness value lower than 6 kPa have none or minimal fibrosis and can be monitored non-invasively [5].
We found that pSWE was poor for the diagnosis of fibrosis stage ≥ F1, fair for the diagnosis of fibrosis stages ≥ F2 and excellent for fibrosis stage ≥ F3 and F4, whereas TE was fair for the diagnosis of fibrosis stages ≥ F1, good for the diagnosis of fibrosis ≥ F2, and excellent for ≥ F3 and F4. Our study showed that TE was significantly better than pSWE for the diagnosis of fibrosis stage ≥ F2. However, statistically significant differences were not found between TE and pSWE AUROC of fibrosis stage ≥ F1, ≥ F3, and F4.
To the best of our knowledge, only few published studies evaluated TE, pSWE and liver biopsy in patients with NAFLD [11, 17,18,19,20,21]. However, some of these studies assessed patients with various etiologies of chronic liver disease including NAFLD [17, 22]. Moreover, some previous studies used different techniques such as Supersonic Imaging and Virtual Touch Quantification. In our study, acoustic radiation force impulse (ARFI) was used in order to stimulate the liver tissue and to generate shear waves that propagate into the liver.
Only a previous study clearly showed that TE was significantly better than pSWE for the diagnosis of fibrosis stage ≥ F2 and ≥ F3, similarly to our data [11]. However, one of the strengths of our study is that all the biopsied liver specimens conformed to international standards for adequacy, which was not the case for the study by Leong et al. despite their samples being deemed subjectively adequate by the pathologist. Furthermore, the patient population in Leong et al. study showed a higher mean fast blood glucose, hypertension and fibrosis prevalence. Therefore, the two study populations are not similar, and the results could not be comparable. Our optimal cut off values were 4.23 and 4.63 kPa, respectively, for the diagnosis of fibrosis stages ≥ F1 and ≥ F2 with pSWE method, and 5.20 and 5.30 kPa, respectively, for the diagnosis of fibrosis stages ≥ F1 and ≥ F2 with TE. This values are lower than the ones obtained by Leong et al. probably due to the fact that in our population many patients (42%) had a F0 fibrosis stage and only few patients (4%) had F4 fibrosis.
Observing AUROC curves in Lee et al. study it seems that ARFI showed lower performance for the diagnosis of fibrosis stage ≥ F2. However, patients mean body mass index in Lee et al. study is lower than in our study (27.1 vs. 29.1); therefore, the study populations are different [18].
For the diagnosis of significant fibrosis (≥ F2) Cassinotto et al. reported that TE had a better diagnostic performance than ARFI; however, this difference was not statistically significant [19]. Similarly, for the diagnosis of severe fibrosis and cirrhosis Friedrich-Rust et al. showed a lower but not statistically significant ARFI AUROC than TE AUROC [20].
On the contrary, for the diagnosis of significant fibrosis (≥ F2) in obese patients Attia et al. reported a better ARFI performance compared to TE one. However, no significant difference was detected between liver stiffness measurement using ARFI and TE for the diagnosis of fibrosis stage ≥ F3 and ≥ F4 in overweight and obese patients. In this study, a Virtual Touch Tissue Quantification technique was used; therefore, the authors argue that the different results between their study and this one could be justified by the use of different techniques [21].
In a recent meta-analysis Selvaraj et al. showed acceptable diagnostic accuracy for advanced fibrosis and cirrhosis for both pSWE and TE in adult patients with NAFLD [23].
Finally, Lafebvre et al. reported no significant differences in AUROCs between TE and pSWE for the diagnosis of fibrosis stages ≥ F1, ≥ F2, ≥ F3 and F4 [22].
The current study has some limitations. It is a single-institution analysis, with a limited number of patients, particularly with fibrosis stages ≥ F3 and F4. Moreover, pSWE inter-observer variability was not evaluated. However, very few studies were published in this field. What is more, a strength of this study was that all the biopsied liver specimens conformed to international standards for adequacy.
In conclusion, our study indicates that TE is significantly better than pSWE in the diagnosis of advanced fibrosis in patients with NAFLD; therefore, TE could be used in association with other non-invasive methods in these patients.
References
Younossi ZM, Koenig AB (2016) Global epidemiology of nonalcoholic fatty liver disease—meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 64:73–84. https://doi.org/10.1002/hep.28431
Loomba R, Sanyal AJ (2013) The global NAFLD epidemic. Nat Rev Gastroenterol Hepatol (N Y) 350:1–5. https://doi.org/10.1038/nrgastro.2013.171
Bedogni G, Miglioli L (2005) Prevalence of and risk factors for nonalcoholic fatty liver disease: the dionysos nutrition and liver study. Hepatology 42:44–52. https://doi.org/10.1002/hep.20734
Araújo AR, Rosso N, Bedogni G et al (2018) Global epidemiology of non-alcoholic fatty liver disease/non-alcoholic steatohepatitis: what we need in the future. Liver Int 38:47–51. https://doi.org/10.1111/liv.13643
Gunn NT, Shiffman ML (2018) The use of liver biopsy in nonalcoholic fatty liver disease: when to biopsy and in whom. Clin Liver Dis 22:109–119. https://doi.org/10.1016/j.cld.2017.08.006
Piccinino F, Sangelli F (1986) Complications following percutaneous liver biopsy. A multicentre retrospective study on 68,276 biopsies. J Hepatol 2(2):165–173. https://doi.org/10.1016/s0168-8278(86)80075-7
European Association for the Study of the Liver (EASL), The SEA for, Diabetes (EASD) of, Obesity (EASO) European Association for the Study of EASL–EASD–EASO (2016) Clinical practice guidelines for the management of non-alcoholic fatty liver disease. J Hepatol 64:1388–1402. https://doi.org/10.1016/j.jhep.2015.11.004
Cosgrove D, Piscaglia F, Bamber J et al (2013) EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 2: clinical applications. Ultraschall Med 34:238–253
Dietrich CF, Bamber J et al (2017) EFSUMB guidelines and recommendations on the clinical use of liver ultrasound elastography, update 2017 (Long Version). Ultraschall Med 2017:16–47
Argalia G, Tarantino G, Ventura C et al (2021) Shear wave elastography and transient elastography in HCV patients after direct—acting antivirals. Radiol Med 126(6):894–899. https://doi.org/10.1007/s11547-020-01326-4
Leong WL, Lai LL, Raihan N et al (2019) Comparing point shear wave elastography (ElastPQ) and transient elastography for diagnosis of fi brosis stage in non- alcoholic fatty liver disease. J Gastroenterol Hepatol. https://doi.org/10.1111/jgh.14782
Shen FF, Lu LG (2016) Advances in noninvasive methods for diagnosing nonalcoholic fatty liver disease. J Dig Dis. https://doi.org/10.1111/1751-2980.12384
Boursier J, Zarski JP, de Ledinghen V et al (2013) Multicentric group from ANRS/HC/EP23 FIBROSTAR studies. Determination of reliability criteria for liver stiffness evaluation by transient elastography. Hepatology 57(3):1182–1191. https://doi.org/10.1002/hep.25993
Ferraioli G, Parekh P, Levitov AB, Filice C (2014) Shear wave elastography for evaluation of liver fibrosis. J Ultrasound Med 33:197–203. https://doi.org/10.7863/ultra.33.2.197
Schiano TD, Azeem S, Bodian CA et al (2005) Importance of specimen size in accurate needle liver biopsy evaluation of patients with chronic hepatitis C. Clin Gastroenterol Hepatol 3:930–935. https://doi.org/10.1016/S1542-3565(05)00541-0
Kleiner DE, Brunt EM, Van NM et al (2005) Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 41:1313–1321. https://doi.org/10.1002/hep.20701
Ferraioli G, De Silvestri A, Reiberger T et al (2018) Adherence to quality criteria improves concordance between transient elastography and ElastPQ for liver stiffness assessment—A multicenter retrospective study. Dig Liver Dis 50:1056–1061. https://doi.org/10.1016/j.dld.2018.03.033
Lee MS, Bae JM, Joo SK et al (2018) Correction: prospective comparison among transient elastography, supersonic shear imaging, and ARFI imaging for predicting fibrosis in nonalcoholic fatty liver disease. PLoS ONE 13:1–17. https://doi.org/10.1371/journal.pone.0200055
Cassinotto C, Boursier J, de Lédinghen V et al (2016) Liver stiffness in nonalcoholic fatty liver disease: a comparison of supersonic shear imaging, FibroScan, and ARFI with liver biopsy. Hepatology 63:1817–1827. https://doi.org/10.1002/hep.28394
Friedrich-Rust M, Romen D, Vermehren J et al (2012) Acoustic radiation force impulse-imaging and transient elastography for non-invasive assessment of liver fibrosis and steatosis in NAFLD. Eur J Radiol 81:325–331. https://doi.org/10.1016/j.ejrad.2011.10.029
Attia D, Bantel H, Lenzen H et al (2016) Liver stiffness measurement using acoustic radiation force impulse elastography in overweight and obese patients. Aliment Pharmacol Ther 44:366–379. https://doi.org/10.1111/apt.13710
Lefebvre T, Wartelle-Bladou C, Wong P et al (2019) Prospective comparison of transient, point shear wave, and magnetic resonance elastography for staging liver fibrosis. Eur Radiol 29:6477–6488. https://doi.org/10.1007/s00330-019-06331-4
Selvaraj EA, Mózes FE, Jayaswal ANA et al (2021) Diagnostic accuracy of elastography and magnetic resonance imaging in patients with NAFLD: a systematic review and meta-analysis. J Hepatol 75:770–785. https://doi.org/10.1016/j.jhep.2021.04.044
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Contributions
GA, GSB, and AG conceived the study. CV, NT, DC, MT, and MC were involved in data collection. CT analysed data. GA, GSB, CV and NT interpreted data. CV, NT were the major contributors in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no potential conflicts of interests associated with this study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Argalia, G., Ventura, C., Tosi, N. et al. Comparison of point shear wave elastography and transient elastography in the evaluation of patients with NAFLD. Radiol med 127, 571–576 (2022). https://doi.org/10.1007/s11547-022-01475-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-022-01475-8