Abstract
Purpose
Glucocorticoids (GCs) and external radiotherapy (RT) are used for treating moderate-to-severe Graves’ orbitopathy (GO). We aimed to assess whether GCs and RT were more effective when administered concomitantly or sequentially.
Methods
We retrospectively analyzed clinical outcomes [assessed by Clinical Activity Score (CAS) and NOSPECS classification] in 73 patients treated with both i.v. GCs and RT. The patients were divided in two groups: In group A (53 patients), RT was delivered concomitantly with GCs, and in group B (20 patients) RT was administered subsequently to the end of methylprednisolone.
Results
At baseline, CAS (median 4.0) and the percentage of patients encompassing the various grades of the classes 2, 3 and 4 of the NOSPECS score were similar in both groups. Six months after RT, CAS decreased to 2 in both groups (p = 0.0003 vs baseline) as well as NOSPECS class 4 (p < 0.0001 vs baseline). NOSPECS class 2 improved more in group A than in group B (p = 0.016). The median cumulative dose of GCs was lower in group A than in group B (median 4.500 vs 6000 mg, p < 0.007); the overall length of therapy was shorter in group A than in group B (68 vs 106 days, p < 0,02). The most common acute adverse effect was transient conjunctivitis (five in group A and three in group B); seven patients (five in group A and two in group B, age between 60 and 66 years) developed cataract, requiring surgery in five cases.
Conclusions
Concomitant administration of GC and RT showed a favorable effect in moderate-to-severe GO, thus suggesting that RT should be carried out early during steroid therapy, when clinical symptoms do not improve or deteriorate after the first i.v. administrations of GCs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Grave’s orbitopathy (GO) is an autoimmune process leading to ocular symptoms complex, which can cause impairment of the patient’s quality of life and visual function. In most cases, GO is characterized by mild ocular inflammation, but more severe signs and symptoms of inflammation, exophthalmos, involvement of extraocular muscles with diplopia, sight loss due to dysthyroid optic neuropathy (DON), corneal ulcerations and, in more advanced cases, perforations with consequent blindness may occur [1].
Glucocorticoids (GCs) are currently the first-line therapy for moderate-to-severe ophthalmopathy, but they are only effective in 50–80% of cases [2], with a non-negligible risk of relapse after their withdrawal [3]. Also radiotherapy (RT) has been used alone [4,5,6,7,8] or in combination with oral or intravenous GCs [9,10,11,12,13,14], showing a good efficacy and safety [15], which were also confirmed by several metanalysis [16,17,18]. However, to our knowledge, the impact of timing of RT administration on outcome in patients treated with i.v. GCs has not been addressed by any trial.
The aim of the present study was to evaluate whether orbital RT administered concomitantly or subsequently to steroids might influence the outcome in a rather large series of patients referred to our Thyroid Clinic for moderate-to-severe GO.
Materials and methods
From March 2003 to September 2016, 73 patients with moderate-to-severe GO were referred to the Centre for Thyroid Diseases at our hospital. Due to retrospective design of this analysis, informed consent was not obtained from the patients.
All patients underwent laboratory evaluation of TSH, free T4, free T3, AbTPO, AbTg and thyrotropin receptors antibodies (TRAb) titers and thyroid US scan. Ophtalmological evaluation included exopthalmometry (by Hertel exophtlamometer), measurement of eyelid aperture, measurement of visual acuity, assessment of ocular motility both by means of the Gorman score of diplopia (defined as absent, intermittent, inconstant and constant) and the Hess-Lancaster test, assessment of GO activity by means of the seven points of the Clinical Activity Score (CAS) [19] and severity by NOSPECS score [2]. Ocular motility was assessed in each patient, while visual field, the color vision test and visual-evoked potentials were carried out when dysthyroid optic neuropathy (DON) was suspected.
Furthermore, 68 patients underwent imaging of the orbital region with magnetic resonance, while CT scan was performed in the remaining patients, due to allergy to nichel or claustrophobia.
Orbitopathy was defined as moderate to severe according to the consensus statement of both American Thyroid Association and European Group on Graves’ Orbitopathy (EUGOGO) [20] that recommended the following definition: patients without sight-threatening GO whose eye disease has sufficient impact of daily life to justify the risks of immunosuppression (if active), that is with a CAS score of at least 3/7 according to the more recent EUGOGO guidelines [2] or surgical intervention (if inactive). Such patients usually have two or more of the following: lid retraction ≥ 2 mm, moderate or severe soft-tissue involvement, or exophthalmos ≥ 3 mm above normal for race and gender, inconstant or constant diplopia [2].
All these clinical signs were assessed by a skilled ophthalmologist, with an experience in GO of more 10 years.
Clinical and laboratory evaluations were carried out again 6 months after the end of RT, and about every 6/12 months for the entire follow-up period.
At our institution, in moderate-to-severe GO i.v. steroids are the first-line treatment, whereas orbital RT is associated when the response to steroids is unsatisfactory. RT is administered concomitantly or sequentially, according to the initial clinical response to i.v. methylprednisolone (MPN). The decision to start RT during a GC course of treatment is taken when no response or a deterioration of the opthalmological symptoms (defined by at least one of the following criteria: increase of CAS ≥ 1/7 points, increase of eyelid aperture ≥ 2 mm, appearance or worsening of diplopia) are seen after the first 5–6 administrations of MPN.
All the enrolled patients received GCs as initial therapy, which were administered weekly as intravenous pulses of methylprednisolone acetate for 10–12 weeks. In 53 subjects, RT was delivered during glucocorticoid treatment, beginning in the middle of the first i.v. GCs course of treatment (Group A), while in 20 cases RT was started 16–90 days after the end of GCs (Group B); in the latter group, further doses of MPN were given at the time of RT.
Orbital radiation therapy
The patients were immobilized with a customized face mask, and orbital CT planning simulation was performed with 3-mm-thick contiguous sections. All patients were treated with a total dose of 19.8 Gy in 11 fractions, 5 days a week with two opposed conformal lateral fields to cover both retrobulbar tissues and extraocular muscles using 6-MV photon beams energy delivered by linear accelerator (Clinac DBX, Varian Medical System Inc., Palo Alto, CA, USA).
The radiation dose to the opposite lens was reduced by angling the lateral beams 3° posteriorly. Acute reactions and late toxicity were analyzed using the Common Terminology Criteria for Adverse Events (CTCAE) Version 4.0 at the end of the treatment and during the follow-up, respectively.
Orbital surgery
It was performed when the disease was made inactive by previous therapies, but proptosis, muscles dysfunction or aesthetic discomfort persisted at least 6 months after the end of RT. Surgical orbital decompression in an emergency setting was not performed in any case.
Statistical analysis
The results of the evaluation carried out 6 months after RT and at the end of the long-term follow-up were considered. The data were analyzed for the whole series of 73 patients and separately for groups A and B.
Variables were tested for normal distribution (Wilk–Shapiro’s test) and, when confirmed, the results were expressed as mean ± standard deviation (SD). Otherwise, they were given as median and interquartile range (IQR).
Statistical differences in continuous variables were assessed by the Wilcoxon test for paired samples. Categorical variables (scores) were compared by Pearson χ2 analysis.
P values are two-sided and considered significant when < 0.05. All analyses were performed using Analyse-it (version 4.60.1 for Microsoft Excel; trademark of Analyse-it software, Ltd).
Results
The demographic and clinical characteristics of the patients are reported in Table 1. In all hyperthyroid patients, thyroid function was normalized with antithyroid drugs (ATD) at the time of RT. 51.4% of hyperthyroid subjects required a definitive treatment by surgery or radioiodine, which was performed 6–12 months after the end of GCs and RT; in 48.6%, the complete remission of hyperthyroidism was obtained by ATD only.
The median length of the orbitopathy at the beginning of RT in the 73 patients as a whole was 9 months [IQR 6–18], slightly but not significantly longer in group B than in group A (median 8 months [IQR 6–13] vs. 13.5 months [IQR 6.75–18.75]). The median duration of thyroid dysfunction was 13.7 months [IQR 6.9–18.9] in group A, and 14.1 months [IQR 7.1–19.2] in group B.
The overall mean follow-up after RT was 50 ± 39 months in the whole group, slightly longer in group B (62 ± 45 months) than in group A (46 ± 35 months).
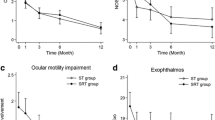
CAS
At the start of RT, median CAS was of 4 in both groups [IQR 2–5 in both] and significantly (p < 0.001) decreased to 2 6 months after the end of RT [IQR 1–2 in group A and 1–3 in group B]. At the end of the long-term follow-up, orbitopathy was inactive in almost all the patients, with a median CAS of 0 [IQR 0–1 in both groups] (p < 0.001 vs. baseline and < 0.01 vs. 6 month visit).
NOSPECS
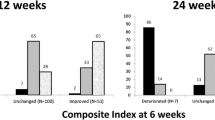
The percentage of patients included in each of the 2 and 4 NOSPECS classes, according to the grade of severity, before, 6 months after the end of RT and at the last follow-up visit, is reported in Figs. 1 and 2.
At the 6-month evaluation, a significant improvement (expressed as the increase in the percentage of patients who shifted from the highest to the lowest grades in each class) in the soft tissue involvement (NOSPECS Class 2) (p = 0.0003), as well as in the extraocular muscle dysfunction (Class 4) (p < 0.0001), occurred in the 73 patients as a whole, while proptosis (Class 3) did not change (exophtalmometry at baseline OD 21.1 ± 3.3 mm, OS 21.2 ± 3.4 mm, at the end of RT OD 21.5 ± 3.4 mm, OS 21.0 ± 3.5 mm). At the long-term follow-up, a further improvement in Class 2 was seen (p < 0.0001); no further change in proptosis (NOSPECS Class 3) and in ocular motility was seen, with the exception of the patients who underwent squint surgery.
When the data were analyzed for groups A and B separately (Figs. 1, 2), neither soft tissue involvement, nor proptosis, nor extraocular muscle dysfunction were significantly different at baseline: So, the two groups were quite homogeneous in eyes involvement. However, the improvement in soft tissue involvement at 6 months was significantly greater in group A than in group B, that is, the number of patients encompassing lower grades in Class 2 was larger in the former than in the latter (p = 0.016) (Fig. 1). No difference between groups was observed in Class 3 and Class 4 at the 6-month evaluation (Fig. 2).
At the last follow-up visit, no difference was seen between group A and B in any of the NOSPECS classes.
Dose of methylprednisolone
The median cumulative dose of MPN was 4500 mg [IQR 4250–6000] in group A, significantly (p < 0.007) lower than in group B [6000 mg; IQR 5104–6750].
Length of treatment
The overall length of treatment, that is, the time from the start of the GCs to the end of RT, was shorter (p < 0.0005) in group A (median 72 days [IQR 48–80]) than in group B (median 98 days [IQR 83–143]). The median interval between the end of the course of GCs and the start of RT in group B was 39 days [IQR 16–90].
Surgery
After glucocorticoids and RT, 22 patients required one or more orbital surgical procedures (orbital decompression, squint or eyelid surgery) (13 in group A and 9 in group B) (Table 1). The proportion of surgical interventions was higher, although not significantly (p = 0.06), in group B.
Hyperthyroidism therapy
The type of definitive treatment for hyperthyroidism was significantly different between the two groups (p = 0.0014): More patients in group A had their thyroid dysfunction cured by ATD alone, while in group B more patients required surgery or radioiodine. At the end of follow-up, all patients were euthyroid or hypothyroid on substitutive LT4 therapy with normal free-thyroxine and TSH serum levels. A comparison between the titers of TRAb was unavailable, due to the variation in the laboratory methods over time.
Acute and late toxicity
Eight patients (10.9%, five in Group A and two in Group 2) complained about G1 acute conjunctivitis, erythema and eye burning sensation, four patients suffered from photophobia (three patients at G1 and one patient at G2), two patients of eye pain (one patient at G1 and one patient at G2) and one patient of G1 flashing lights.
Seven patients, for a total of nine eyes (9.5%, five in group A and two in group B), developed a cataract; two of them were 55- and 60-year old, while the age of the other patients ranged between 70 and 75 years. Five cases required surgery at the age of 55, 60, 70, 71 and 72 years, respectively. In all patients who developed cataract, dose constraints to lens were respected, concluding that cataracts were related to physiological aging process instead of RT to retrobulbar areas. None retinal damage was observed.
Discussion
The treatment of GO is challenging for the clinicians, requiring a close collaboration among endocrinologists, ophthalmologists, radiotherapists and surgeons and is guided by the degree of activity and severity of the disease [19].
Immunomodulatory therapy is the first-line approach for moderate-to-severe and active GO [2], showing the maximum efficacy in the first “active” phases of the disease, when the release of cytokines and chemokines by fibroblasts leads to orbital inflammation, while it is less effective in the later phase, when inflammation subsides and fibrotic changes occur in orbital tissues [21]. Immunosuppressive drugs as rituximab are second-line tools [2]. Therefore, GCs still remain the mainstay of the medical therapy of GO, due to their anti-inflammatory and immunosuppressive effects; however, a complete response to GCs is seen in only 50-80% of patients, in particular with regard to extraocular muscle dysfunction [22].
Furthermore, a relapse of the disease activity is not infrequent after withdrawal of GCs [3], and, what is more, GCs may have worrisome side effects [23].
In some cases of moderate-to-severe GO, orbital RT may be an alternative option to GCs, or an additional tool for treating poorly responsive patients, in particular those with extraocular muscle dysfunction [24,25,26].
Previous studies, comparing the effects of RT versus sham-irradiation in patients with moderate-to-severe [5] or mild GO [26], demonstrated a greater efficacy of RT on ocular motility than on the involvement of soft tissues, while proptosis was not significantly affected, whereas other reports highlighted similar improvements in both soft tissue changes and proptosis [7, 9, 27].
On the contrary, Gorman et al. [28] were unable to show any benefit from RT, but their study included patients with longstanding disease, and this may have limited the efficacy of such treatment; also, Rajendram et al. [29] recently reported that in patients receiving oral prednisolone for 24 weeks, RT did not add any benefit.
A Cochrane-based review evidenced that orbital RT could be more effective than sham RT for the treatment of mild-to-moderate GO, without a difference between RT and steroid monotherapy [18].
The mechanisms by which RT exerts its beneficial effects in GO differ from those of steroids: Indeed, the effects of RT are mainly related to its ability to destroy the lymphocytes infiltrating the orbit and to affect the capacity of orbital fibroblast to synthesize glycosaminoglycans, whereas GCs reduce the release of pro-inflammatory molecules from lymphocytes and fibroblasts [17].
The two different mechanisms of action of GCs and RT may be a rational basis for combining GCs and RT in the treatment of GO, in particular, in more severe cases, allowing to obtain a beneficial additional effect [12, 13, 30]. Nicosia et al. [14] showed that RT plus concomitant i.v. GCs was effective in moderate-to-severe orbitopathy, thus helping to prevent surgery in some cases, but in their study a control group was not included, while Ohtsuka was unable to demonstrate a difference in the outcome when GCs were followed by RT [10].
The combination of systemic GCs and orbital RT was more effective than RT alone on both soft tissue changes and ocular motility in patients with GO of recent onset [30].
Nevertheless, some issues are still unresolved, for example what is the best timing for delivering RT in GC-treated patients (in conjunction with GCs or after the end of a first course of GCs).
At our institution, we treated 73 patients with moderate-to-severe GO with a combination of i.v. GCs and RT, administered simultaneously or subsequently. The decision of starting RT during the first course of GCs was taken when no improvement or a worsening of the opthalmological symptoms was recorded halfway through the course of MPN.
A recent literature report seems to support this decision-making in the management of moderate-to-severe GO.
Indeed, Bartalena et al. reported that in 159 patients, treated with three different doses of MPN, an early response to i.v. GCs may be predictive of a favorable outcome, thus encouraging the continuation of the therapy. In those patients showing no change or a deterioration of ophthalmic involvement after the first infusions, an improvement was unlikely to be recorded at the end of the course of GCs: Therefore, a second line of treatment should be performed, such as the combination of RT and GCs, or rituximab or cyclosporine [31].
In our series, RT and GCs were performed simultaneously in 53 patients (Group A, 72.6%) and subsequently in 20 (Group B, 27.4%). This difference in the numerousness of the two groups may be a limitation of the present study, as well as the fact that it is a retrospective analysis encompassing a long span of time. However, it is worth noting that, despite the number of patients being larger in group A than in group B, the two groups were quite homogeneous with regard to CAS and NOSPECS score both at diagnosis and at the start of RT, making them suitable for a comparative analysis. Moreover, when the therapy for orbitopathy was started, normal thyroid function was already restored with medical therapy in most patients in both groups.
The first interesting finding of our analysis is that at 6 months, the improvement in NOSPECS Class 2 in group A was significantly greater than in group B; this could seem to be in contrast with the absence of a significant difference observed in CAS at the same time in both groups, but we must take into account that CAS and NOSPECS Class 2 do not reflect exactly the same clinical parameters, as CAS encompasses symptoms, such as ocular pain, which are not included in Class 2.
As to the explanation of this finding, we can argue that it was mainly due to the combination of the effects of GCs on the release of pro-inflammatory factors and the ability of RT to destroy orbital lymphocytes; such additional effects may be less marked when GCs and RT are administered some weeks or months apart. We might also speculate that this difference is related to the transient soft tissue inflammation induced by RT, but this seems unlike since further MPN doses were given in conjunction with RT to hamper its inflammatory effects.
At long-term follow-up, this difference disappeared, though this is not surprising, since other factors, such as surgical procedures or other circumstances related to the natural history of the disease, may have occurred to influence the final outcome, characterized by an inactivation of the disease in almost all the patients.
Extraocular muscle dysfunction improved in both groups similarly; we could have expected an advantage related to concomitant therapy, but the absence of a significant difference could depend on the fact that in some patients, RT was started rather early after the completion of the course of GCs.
Another factor to be considered is that, when the patients underwent RT subsequently to the first course of GCs, they were further treated with steroids to hamper the possible orbital tissue edema related to RT: therefore, we cannot exclude that these supplementary doses of steroids could have contributed to the improvement in ocular motility in some patients in group B.
Indeed, the patients in group B received a significantly higher cumulative dose of MPN than those in group A; this aspect should be kept in mind when the management of GO is planned, considering the potential toxicity of high doses of steroids.
A further observation is that the improvement in ocular motility occurs in the first months after therapy (independently of the therapeutic protocol), while after this time further amelioration cannot be expected, possibly due to the occurrence of muscle fibrosis [21]. Therefore, rehabilitative surgery should be planned quickly, if diplopia persists 6 months after the completion of the treatment of the active phase.
Another finding was that in group A, the overall length of therapy was significantly shorter than in group B: Despite this is an obvious observation, taking into account the limitations and the impairment on the quality of life in patients with moderate-to-severe GO, the possibility to obtain a clinical improvement in a shorter time has a considerable advantage.
Unlike soft tissues and extraocular muscle involvement, proptosis did not significantly improve in either groups after 6 months: However, this finding is in agreement with literature data, showing an inconsistent benefit of both GCs and RT on this clinical manifestation [3,4,5]. However, a reduction in proptosis was seen after long-term follow-up; we cannot exclude that this improvement was due to the long-term effects of GCs or RT, but it is conceivable that it was related to the natural course of the disease or, in some cases, to surgical procedures.
At our institution, RT for GO is currently administered with a total dose of 19.8 Gy in 11 fractions, according to the current standard protocol [3, 32].
We have reported only 10.9% acute toxicity, mainly represented by a transient mild conjunctivitis.
Retinopathy (especially in patients affected by diabetes) and cataract will definitely be assessable though only after a longer follow-up. According to literature data [33], in our series we found 9.5% of cataract incidence, with five patients requiring surgery; however, it is difficult to ascertain if these cases are only RT-related or may have been linked to an age-related process, since five out of seven patients were older than 70 yrs when cataract developed.
In conclusion, despite some limitations, mainly related to its retrospective design and to the difference in the number of patients included in the two groups, this study provides some interesting observations that could support the simultaneous use of GCs and RT in the treatment of moderate-to-severe forms of GO poorly responsive to glucocorticoids.
Therefore, based on our findings, a decision-making process including a reassessment of the CAS and NOSPECS score after the first administrations of GCs could be appropriate: In the case of no response or worsening of ophtalmological symptoms, a course of external beam irradiation would be indicated immediately. Prospective randomized studies are required to confirm these findings.
References
Bartalena L, Tanda ML (2009) Cinical practice. Graves’ Orbitopathy. New Engl J Med 360:994–1001
Bartalena L, Baldeschi L, Boboridis K, Eckstein A, Kahaly GJ, Marcocci C, Perros P, Salvi M, Wiersinga WM (2016) The 2016 European Thyroid Association/European Group on Graves’ orbitopathy guidelines for the management of graves’ orbitopathy. Eur Thyroid J 5:9–26
Bartalena L, Pinchera A, Marcocci C (2000) Management of Graves’ ophthalmopathy: reality and perspectives. Endocr Rev 21:168–199
Prummel MF, Mourits MP, Blank L, Berghout A, Koornneef L, Wiersing WM (1993) Randomized double-blind trial of prednisone versus radiotherapy in Graves’ ophthalmopathy. Lancet 342:949–954
Mourits MP, Van Kempen-Hartevel ML, García MBG, Koppeschaar HP, Tick L, Terwee CB (2000) Radiotherapy for Graves’ orbitopathy: randomized placebo-controlled study. Lancet 355:1505–1509
Marquez SD, Lum BL, McDougall IR, Katkuri S, Levin PS, MacManus M, Donaldson SS (2001) Long-term results of irradiation for patients with progressive Graves’ ophthalmopathy. Int J Radiat Oncol Biol Phys 51:766–774
Matthiesen C, Thompsom JS, Thompson D, Farris B, Wilkes B, Ahmad S, Herman T, Bogardus C (2012) The efficacy of radiation therapy in the treatment of graves’ orbitopathy. Int J Radiat Oncol Biol Phys 82:117–123
Prabhu RS, Liebman L, Wojno T, Hall WA, Crocker I (2012) Clinical outcomes of radiotherapy as imitial local therapy for Graves’ ophtalmopathy and predictors of the need for post-radiotherapy decompressive surgery. Radiat Oncol 7:95–102
Tsujino K, Hirota S, Hagiwara M, Fukada S, Takada Y, Hishikawa Y, Kono M, Abe M (2000) Clinical outcomes of orbital irradiation combined with or without systemic high-dose or pulsed corticosteroids for Graves’. Ophtalmopathy 48:857–864
Ohtsuka K, Sato A, Kawaguchi S, Hashimoto M, Suzuki Y (2003) Effect of steroid pulse therapy with and without orbital radiotherapy on Graves’ ophthalmopathy. Am J Ophthalmol 135:285–290
Marcocci C, Bartalena L, Tanda ML, Manetti L, Dell’Unto E, Rocchi R, Barbesino G, Mazzi B, Bartolomei MP, Lepri P, Cartei F, Nardi M, Pinchera A (2001) Comparison of the effectiveness and tolerability of intravenous or oral glucocorticoids associated with orbital radiotherapy in the management of severe Graves’ ophthalmopathy: results of a prospective, single-blind, randomized study. J Clin Endocrinol Metab 86:3562–3567
Abboud M, Arabi A, Salti I, Geara F (2011) Outcome of thyroid associated ophtalmopathy treated by radiation therapy. Radiat Oncol 6:46–51
Sisti E, Menconi F, Leo M, Profilo MA, Mautone T, Mazzi B, Rocchi R, Latrofa F, Nardi M, Vitti P, Marcocci C, Marinò M (2015) Long-term outcome of Graves’ orbitopathy following high-dose intravenous glucocorticoids and orbital radiotherapy. J Endocrinol Invest 38:661–668
Nicosia L, Reverberi C, Agolli L, Marinelli L, De Sanctis V, Minniti G, Valeriani M, Osti MF (2019) Orbital radiotherapy plus concomitant steroids in moderate-to-severe Graves’ Ophtlamopathy: good results after long-term follow-up Int J. Endocrinol Metab 17:e84427
Wakelkamp IMM, Tan H, Saeed P, Schlingemann RO, Verbraak FD, Blank LEC, Prummel MF, Wiersinga WM (2004) Orbital irradiation for Graves’ ophthalmopathy. Ophthalmology 111:1557–1562
Viani GA, Boin AC, De Fendi LI, Fonseca EC, Stefano EJ, de Paula JS (2012) Radiation therapy for Graves’ ophthalmopathy: a systematic review and meta-analysis of randomized controlled trials. Arq Bras Oftalmol 75:324–332
Godfrey KJ, Kazim M (2018) Radiotherapy for active thyroid eye disease. Ophthalmic Plast Reconstr Surg 34:S98–S104
Rajendram R, Bunce C, Lee RW, Morley AM (2012) Orbital radiotherapy for adult thyroid eye disease. Cochrane Database Syst Rev 7:CD007114
Wiersinga WM, Perros P, Kahaly GJ, Mourits MP, Baldeschi L, Boboridis K, Boschi A, Dickinson AJ, Kendall-Taylor P, Krassas GE, Lane CM, Lazarus JH, Marcocci C, Marinò M, Nardi M, Neoh C, Orgiazzi J, Pinchera A, Pitz S, Prummel MF, Sartini MS, Stahl M, Arx V (2006) Clinical assessment of patients with Graves’ orbitopathy: the European Group on Graves’ Orbitopathy recommendations to generalists, specialists and clinical researchers. Eur J Endocrinol 155:387–389
Bartalena L, Baldeschi L, Dickinson A, Eckstein A, Kendall-Taylor P, Marcocci C, Mourits M, Perros P, Boboridis K, Boschi A, Currò N, Daumerie C, Kahaly GJ, Krassas GE, Lane CM, Lazarus JH, Marinò M, Nardi M, Neoh C, Orgiazzi J, Pearce S, Pinchera A, Pitz S, Salvi M, Sivelli P, Stahl M, von Arx G, Wiersinga WM (2008) Consensus statement of the European Group on Graves’ orbitopathy (EUGOGO) on management of GO. Eur J Endocrinol 158:273–285
Hiromatsu Y, Eguchi H, Tani J, Kasaoka M, Teshima Y (2014) Graves’ Ophthalmopathy: epidemiology and Natural History. Int Med 53:353–360
Marcocci C, Marinò M (2012) Treatment of mild, moderate-to-severe and very severe Graves’ orbitopathy. Best Pract Res Clin Endocrinol Metab 26:325–337
Zang S, Ponto KA, Kahaly GJ (2011) Intravenous glucocorticoids for Graves’ orbitopathy: efficacy and morbidity. J Clin Endocrinol Metab 96:320–332
Bartalena L (2013) Graves’ orbitopathy: imperfect treatments for a rare disease. Eur Thyroid J 2:259–269
Tanda ML, Bartalena L (2012) Efficacy and safety of orbital radiotherapy for Graves’ orbitopathy. J Clin Endocrinol Metab 97:3857–3865
Prummel MF, Terwee CB, Gerding MN, Baldeschi L, Mourits MP, Blank L, Dekker FW, Wiersinga WM (2004) A randomized controlled trial of orbital radiotherapy versus sham irradiation in patients with mild graves’ ophthalmopathy. J Clin Endocrinol Metab 89:15–20
Zygulska A (2009) Radiotherapy in the treatment of Graves ophthalmopathy—to do it or not? J Ocul Biol Dis Inform 3:1–11
Gorman CA, Garrity JA, Fatourechi V, Bahn RS, Petersen IA, Stafford SL, Earle JD, Forbes GS, Kline RW, Bergstralh EJ, Offord KP, Rademacher DM, Stanley NM, Bartley GB (2001) A prospective, randomized, double-blind, placebo-controlled study of orbital radiotherapy for Graves’ ophthalmopathy. Ophthalmology 108:1523–1534
Rajendram R, Taylor PN, Wilson VJ, Harris N, Morris OC, Tomlinson M, Yarrow S, Garrott H, Herbert HM, Dick AD, Cook A, Gattamaneni R, Jain R, Olver J, Hurel SJ, Bremner F, Drummond SR, Kemp E, Ritchie DM, Rumsey N, Morris D, Lane C, Palaniappan N, Li C, Pell J, Hills R, Ezra DG, Potts MJ, Jackson S, Rose GE, Plowman N, Bunce C, Uddin JM, Lee RWJ, Dayan CM (2018) Combined immunosuppression and radiotherapy in thyroid eye disease (CIRTED): a multicentre, 2 × 2 factorial, double-blind, randomised controlled trial. Lancet Diabetes Endocrinol 6:299–309
Marcocci C, Bartalena L, Bogazzi F, Bruno-Bossio G, Lepri A, Pinchera A (1991) Orbital radiotherapy combined with high dose systemic glucocorticoids for Graves’ ophthalmopathy is more effective than radiotherapy alone: results of a prospective randomized study. J Endocrinol Invest 14:853–860
Bartalena L, Veronesi G, Krassas GE, Wiersinga WM, Marcocci C, Marinò M, Salvi M, Daumerie C, Bournaud C, Stahl M, Sassi L, Azzolini C, Boboridis KG, Mourits MP, Soeters MR, Baldeschi L, Nardi M, Currò N, Boschi A, Bernard M, von Arx G, Perros P, Kahaly GJ (2012) European Group on Graves’ Orbitopathy (EUGOGO) (2017): Does early response to intravenous glucocorticoids predict the final outcome in patients with moderate-to-severe and active Graves’ orbitopathy? J Endocrinol Invest 40:547–553
Kahaly GJ, Rösler H-P, Pitz S, Hommel G (2000) Low- versus high-dose radiotherapy for graves’ ophthalmopathy: a randomized. Single Blind Trial J Clin Endocrinol Metab 85:102–108
Marcocci C, Bartalena L, Rocchi R, Marinò M, Menconi F, Morabito E, Mazzi B, Mazzeo S, Sartini MS, Nardi M, Cartei F, Cionini L, Pinchera A (2003) Long-term safety of orbital radiotherapy for graves’ ophthalmopathy. J Clin Endocrinol Metab 88:3561–3566
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Limone, P.P., Bianco, L., Mellano, M. et al. Is concomitant treatment with steroids and radiotherapy more favorable than sequential treatment in moderate-to-severe graves orbitopathy?. Radiol med 126, 334–342 (2021). https://doi.org/10.1007/s11547-020-01244-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-020-01244-5