Abstract
Objective
Intravenous (iv) glucocorticoids (GC) (ivGC) and orbital radiotherapy (ORT) are commonly used in active Graves’ orbitopathy (GO), with favorable outcomes in up to 80 % of patients. However, little is known on the factors that may affect GO outcome in the long term, an issue that we investigated here.
Methods
We studied retrospectively 96 untreated patients with GO, identified out of 787 consecutive patients who came to our GO Clinic for a follow-up visit between September 2010 and June 2013. After the first observation, patients were treated with ivGC and ORT and were then re-examined after a median period of 55.5 months. The primary end-point was the possible relation between GO outcome and several individual variables.
Results
Exophthalmometry, eyelid aperture, CAS, diplopia and visual acuity (the latter only in patients with an initial reduction) improved significantly after treatment. Overall, 67.7 % of patients had improved and were considered as responders, whereas the remaining (29.1 % stable and 4.5 % worsened) were considered as non-responders. Age, smoking, thyroid volume, thyroid treatment, serum anti-TSH receptor autoantibodies and individual GO features at first observation did not affect the outcome of GO, which, in contrast, was affected by gender and by the time elapsed between first and last observation. Thus, the prevalence of responders was higher in females (76.4 vs 48 % in males, P = 0.02) and the time elapsed between first and last observation was greater in responders (58 vs 39 months in non-responders, P = 0.02). Whereas the prevalence of responders and non-responders was similar up to 36 months, there was an increase in responders beginning between 37 and 48 months and reaching a peak of ~80 % between 61 and 72 months, to plateau thereafter.
Conclusions
Given the limitations of retrospective investigations, our study confirms that the combination of GC and ORT is effective in GO and shows that females have greater chances to respond to treatment. The notorious tendency of GO to improve spontaneously with time most likely contributes the long-term outcome of the eye syndrome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The combination of high-dose intravenous (iv) glucocorticoids (GC) (ivGC) and orbital radiotherapy (ORT) is a well-established treatment for active Graves’ orbitopathy (GO) [1–7], the most common extrathyroidal manifestation of Graves’ disease [8, 9]. The use of systemic glucocorticoids takes advantage from their immune suppressive and antiinflammatory actions, which results in an overall beneficial effect on GO, ranging from ~60 to ~85 % of patients in various studies [6]. Several investigations have shown that the intravenous route of administration is superior to the oral route, both in terms of GO outcome and GC side effects [6], the latter in spite of the observation of a few cases of severe liver damage in patients given ivGC [10, 11]. ORT is used in GO because of its general antiinflammatory properties and, more specifically, because of its possible ability of damaging lymphocytes infiltrating orbital tissues, thereby exerting a local immune suppressive action [7]. There have been debates on whether ORT is actually effective for GO and on whether it should be employed, although the majority of studies have shown a good response to treatment, especially if associated with GC [7].
Based on findings of previous studies [1–7], in our Center we use routinely the combination of ivGC and ORT in patients with moderate–severe, active GO, regardless of thyroid treatment [12]. In the present study, we took advantage of the fact that the majority of our GO patients undergo routine visits in our GO Clinic, thereby allowing us to investigate retrospectively the outcome of GO treated with ivGC and ORT after a relatively long period of time, with the aim of indentifying factors that may affect the response of GO to treatment, an information that could be useful when designing a therapeutic strategy for GO. Thus, although several prospective and retrospective studies have addressed the issue of GO response to ivGC and ORT [1–7], little is known on the factors that may help predict GO outcome.
Patients and methods
Patients
A retrospective cohort study was conducted. Patients who met the following criteria were included: (1) no treatments for GO before first observation with the exception of eye lubricants; (2) GO treatment with ivGC and ORT between first and last observation; and (3) no treatments for Graves’ hyperthyroidism before first observation, with the exception of anti-thyroid drugs [methimazole (MMI) in all cases]; (4) no additional treatments for GO after the initial treatments.
A total of 96 patients meeting the above-mentioned criteria were identified out of 787 consecutive patients who came to our GO Clinic for a follow-up visit between September 2010 and June 2013. Demographical data on these patients are reported in Table 1. Signed informed consent was obtained from all patients prior to using their data.
Clinical and serological evaluation
All patients underwent an ophthalmological assessment at first and last observation, which included: (1) exophthalmometry; (2) measurement of eyelid aperture; (3) evaluation of the Clinical Activity Score (CAS) according to Mourits [13, 14]; (4) assessment of diplopia; (5) measurement of visual acuity. The GO features of patients are summarized in Table 2.
Serum anti-TSH receptor antibodies (TRAb, Brahms, Berlin, Germany) at first and last observation were available in 93 patients. Thyroid ultrasound was performed in all patients at first observation. Thyroid volume was calculated using the ellipsoid formula, as reported previously [15]. Smoking habits were recorded in all patients. The thyroid features of patients are summarized in Table 1.
Treatments
As reported in Table 1, after the first observation 69 patients underwent treatment with 131I (a single dose of 15 mCi), 11 underwent near-total thyroidectomy, and 16 were treated with a procedure named total thyroid ablation [16–18], namely near-total thyroidectomy followed by 131I (a single dose of 30 mCi). As reported previously [16, 17], in the latter group 131I was given ~45 days after thyroidectomy, and between thyroidectomy and 131I patients were given T3 (40 μg/day) to maintain euthyroidism, which was withdrawn 2 weeks before 131I. All patients were given LT4 at replacement doses after thyroid treatment.
Approximately, 2 weeks after thyroid treatment all patients started ivGC and ORT for GO. Patients were given one iv infusion/week of methylprednisolone acetate for a total of 12 infusions. The dose was 15 mg/kg for the first four infusions (maximum dose allowed 1 g), and 7.5 mg/kg for the last eight infusions. The cumulative dose of GC ranged between ~6 and ~8 g. The reason why we used a relatively low dose of methylprednisolone, compared with that usually used by others [18], was to avoid adverse events associated with ivGC, especially hepatitis [10, 11]. On the other hand, this protocol was largely employed in previous studies [16, 17]. No major side effects of GC were observed. ORT was performed with a high-voltage linear accelerator. A cumulative radiation dose of 10 Gy was delivered to each eye in 10 fractionated doses over a period of 2 weeks. All patients were treated bilaterally.
End-points
The primary end-point of the study was the possible relation between the overall outcome of GO and the following individual variables: age; gender, smoking habits, thyroid volume, thyroid treatment, TRAb at first and last observation, individual GO features at first observation (exophthalmometry, eyelid aperture, CAS, visual acuity, diplopia) and time elapsed between first and last observation. The secondary end-point was to investigate the relation between the variables, if any, affecting the outcome of GO and the individual GO features.
The overall GO outcome was evaluated as follows. GO was considered improved when at least one of the following criteria was fulfilled, without worsening of the other criteria: (1) reduction in proptosis ≥2 mm in at least one eye, with no increase ≥2 mm in the other eye; (2) reduction of CAS ≥1/7 points; (3) reduction in eyelid aperture ≥2 mm in at least one eye, with no increase ≥2 mm in the other eye; (4) disappearance or improvement (change of degree from constant to inconstant or intermittent, or from inconstant to intermittent) of diplopia; (5) increase in visual acuity ≥2/10. GO was considered worsened when at least one of the following criteria was fulfilled: (1) increase of CAS ≥1/7 points; (2) increase in proptosis ≥2 mm; (3) increase in eyelid aperture ≥2 mm; (4) appearance or worsening (change of degree) of diplopia; (5) decrease in visual acuity ≥2/10.
Data presentation and statistical analyses
Descriptive data are presented as median and interquartile range. When appropriate and as indicated, the following tests were performed: (1) Wilcoxon; (2) Mann–Whitney; (3) Fisher exact test.
Results
Outcome of GO following ivGC and ORT
The general and thyroid features of patients are reported in Table 1. The features of GO at first and last observation are reported in Table 2. As mentioned above, all patients were treated with ivGC and ORT and underwent an ophthalmological evaluation after a median follow-up period of 55.5 months. As reported in Table 2, exophthalmometry, eyelid aperture, CAS and diplopia improved significantly after treatment, whereas visual acuity did not. Concerning the latter, the finding is not surprising, considering that the vast majority of patients had a normal visual acuity (10/10) at first observation. Thus, only eight patients had a reduced visual acuity due to optic neuropathy (median: 2/10; IQR 1–4.5, range 0–8), which improved significantly after treatment (median: 8.5/10; IQR 5–8.5, range 5–10; P = 0.007 by Wilcoxon). These eight patients, who clearly had a severe GO, were not excluded as the degree of GO was not among the inclusion and exclusion criteria. In agreement with the clear amelioration of virtually all GO features, we estimated that the majority (67.7 %) of patients had an overall GO improvement, 29.1 had remained stable, whereas only 4.5 % had worsened.
Effect of individual variables on GO outcome
As reported above, the primary end-point of the study was the relation between the outcome of GO and several individual variables. Because of the low number of patients who had worsened, namely three, we grouped them together with patients who had remained stable and considered them as non-responders, whereas patients who had improved were defined as responders. Age, smoking habits, thyroid volume, thyroid treatment, TRAb at first and last observation and individual GO features at first observation (exophthalmometry, eyelid aperture, CAS, visual acuity, diplopia) did not affect significantly the outcome of GO. In contrast and as detailed below, the overall GO outcome was affected significantly by gender and by the time elapsed between first and last observation.
Relation between gender and GO outcome
As shown in Fig. 1, the prevalence of responders was significantly higher in females (76.4 %) than in males (48 %, P = 0.02 by Fisher exact test). We analyzed the individual GO features according to gender. As shown in Table 3, eyelid aperture, CAS, visual acuity and diplopia before treatment did not differ between males and females. In contrast, males had a significantly higher degree of proptosis at first observation. Presumably, the latter reflected the known difference between genders concerning exophthalmometry [19], rather than a more severe GO in males, as suggested by the fact that all other GO parameters before treatment were similar regardless of gender. In confirmation of the better GO outcome in females, after GC and ORT several GO features became significantly different between genders. Thus, in addition to exophthalmometry, which after treatment was still higher in males but to a greater statistical extent, eyelid aperture after treatment was significantly greater in males, as was the extent of eye muscle involvement (degrees of diplopia).
Prevalence of responders (patients who had improved) and non-responders (patients who had remained stable or had worsened) according to gender, in 96 patients with Graves’ ophthalmopathy treated with intravenous high-dose glucocorticoid pulse therapy and orbital radiotherapy, after a median time of 55.5 months. P = 0.02 by Fisher exact test
Relation between time and GO outcome
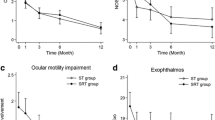
As shown in Fig. 2a, the time elapsed between first and last observation was significantly greater in responders (P = 0.02 by Mann–Whitney). We grouped patients into seven categories according to the time between first and last observation. As shown in Fig. 2b, whereas the prevalence of responders and non-responders was similar up to 36 months, there was an increase in responders beginning between 37 and 48 months and reaching a peak of ~80 % between 61 and 72 months, to plateau thereafter. We analyzed the individual GO features in these seven time groups. As shown in Table 4, exophthalmometry and eyelid aperture were quite variable over time, and visual acuity remained overall stable, the latter presumably due to the low number of patients with optic neuropathy. In contrast, CAS and diplopia were affected by time, thereby reflecting the observations reported in Fig. 2b. Thus, CAS decreased between 13 and 24 months and further between 25 and 36 months, to plateau thereafter. Diplopia improved progressively, beginning at 13–24 months, to reach a peak of amelioration between 37 and 48 months, although its behavior was quite variable compared with that of CAS.
a Median (±IQR) follow-up time (time elapsed between first and last observation) in responders (patients who had improved) and non-responders (patients who had remained stable or had worsened), in 96 patients with Graves’ ophthalmopathy treated with intravenous high-dose glucocorticoid pulse therapy and orbital radiotherapy. P = 0.02 by Mann–Whitney. b Prevalence of responders and non-responders after patient grouping according to the duration of follow-up
Discussion
Although ivGC and ORT are well-established treatments for active GO, little is known on which factors may affect the long-term GO outcome, an information that could be quite useful when designing a therapeutic strategy for GO. Here, we investigated this issue in a retrospective study, performed in a relatively large series of patients with GO. After a median follow-up period of 55.5 months, GO was found to be improved in ~70 % of patients. This finding is in line with the observations of previous retrospective studies on the long-term GO outcome after ORT [20, 21], although comparisons are quite difficult, because of the different patient selection, because in those studies not all patients were given GC, and finally because of the different outcome criteria used. Comparisons with the previous randomized, prospective studies assessing the effectiveness of GC and ORT are also difficult, because of their shorter follow-up periods and because of the fact that in some of those studies patients were treated with oral GC, rather than with ivGC as the patients studied here [22–24].
In any case, the main end-point of the present study was not to investigate the response of GO to treatment, but rather to identify individual variables that may have an influence on the GO outcome in the long term. In this regard, we did not compare the outcome of GO with that of patients treated with ivGC, but not with ORT, which, in any case, would not have been possible because of a selection bias. Thus, in our Center ORT is usually given only to patients with inconstant or constant diplopia, in the absence of which patients are usually treated only with ivGC.
We found that gender and the time elapsed after treatment play a major role. Thus, the prevalence of responders (patients whose GO had improved at the end of follow-up) was greater in females: GO ameliorated in ~75 % of female patients and only in ~50 % of males. The duration of follow-up, which, as reported above, also affected GO outcome, was not different between males and females (not shown), as were all the other parameters examined, with the exception of exophthalmometry at first observation, which was greater in males, presumably reflecting the difference in exophthalmometry between genders already under physiological conditions [19], as also suggested by the fact that all the other GO parameters before treatment did not different between males and females. In agreement with the more favorable GO outcome after treatment in females, at the end of individual follow-up women had a lower degree of proptosis, eyelid aperture and diplopia than men. The obvious consequence of these observations is that, when planning a GO treatment in a given patient, he/she should be made aware of the fact that his/her chances of having a good response in the long term are about 50 and 75 %, respectively. Given the limitations of a retrospective study, an issue discussed also later, in our opinion, together with the severity of GO before treatment and the estimate of risk for ivGC side effects [25], this information should be taken into account when planning the treatment, not the least in view of the patient’s preference once properly informed.
As mentioned above, the duration of follow-up, namely the time elapsed after treatment in individual patients, also affected the outcome of GO, as it was significantly longer in responders (~60 months) than in non-responders (~40 months). In agreement with this observation, the prevalence of responders increased with time, reaching a peak of ~80 % between 61 and 72 months, which is a relatively long period. In this regard, it is possible that this late improvement of GO reflects the natural history of the syndrome rather than treatment. Thus, it is well known that GO improves spontaneously with time [1, 26–29], as we also observed recently in mild GO [29]. CAS and diplopia were the GO features affected by time to a greater extent.
To our surprise, CAS at first observation did not affect the GO outcome in the long term. Thus, GO activity, of which CAS is a well-established measure [14], is known to affect the response to immune suppressive/antiinflammatory treatments [1–6]. How could this observation be explained? Most likely, the lack of relation between CAS and GO outcome is due to the fact that the majority of patients had a quite long follow-up, therefore, as mentioned above, a GO behavior reflecting not only the response to treatment, but also the natural history of the syndrome, which should not be affected by the initial degree of CAS. The same explanation probably applies also to the lack of correlation between the long-term GO outcome and TRAb, and between GO outcome and smoking habits, two factors that also are known to affect the response of GO to treatment [1–7, 30]. On the other hand, before treatment patients had a median CAS value of 3/7 points, indicating an active, but not a very active GO. Thus, CAS, as well as TRAb and smoking that are related to CAS, might not have affected the GO outcome in this series of patients simply because GO was not too much active to begin with, an issue that requires further investigations.
One possible limitation of the present study is that patients were relatively heterogeneous in terms of GO features before treatment, even though the majority of them had a mild-to-moderate GO. Ideally, this issue should be investigated in prospective studies that are certainly needed. Another, maybe even more important, limitation, is the fact that treatment for GO was started 2 weeks after treated of hypothyroidism, meaning that some of the patients given radioiodine might have been hypothyroid, a condition that is known to affect GO in a negative manner [1–7]. On the other hand, thyroid treatment did not seem to affect the outcome of GO, although this conclusion awaits confirmation in view of the relatively low number of patients treated with thyroidectomy or with total thyroid ablation (thyroidectomy followed by radioiodine), considering that the latter procedure has been reported to affect the outcome of GO by several studies [16–18].
Obviously, this study carries the limitations of retrospective investigations. On the other hand, it would be quite difficult to perform a prospective study on the follow-up of GO in the long term. Taking this aspect into account, our observations confirm that the combination of GC and ORT is effective in GO and show that female have greater chances than males to respond to treatment. The notorious tendency of GO to improve spontaneously with time most likely contribute the late amelioration of the eye syndrome. Clearly, further prospective, possibly randomized studies are needed to investigate this issue further.
References
Bartalena L, Tanda ML (2009) Clinical practice. Graves’ orbitopathy. N Engl J Med 360:994–1001
Bartalena L, Pinchera A, Marcocci C (2000) Management of Graves’ ophthalmopathy: reality and perspectives. Endocr Rev 212:168–199
Bartalena L, Wiersinga WM, Pinchera A (2004) Graves’ orbitopathy: state of the art and perspectives. J Endocrinol Invest 27:295–301
Marcocci C, Marinò M (2012) Treatment of mild, moderate-to-severe and very severe Graves’ orbitopathy. Best Pract Res Clin Endocrinol Metab 26:325–337
Marcocci C, Pinchera A, Marinò M (2007) A treatment strategy for Graves’ orbitopathy. Nat Clin Pract Endocrinol Metab 3:430–436
Zang S, Ponto KA, Kahaly GJ (2011) Clinical review: intravenous glucocorticoids for Graves’ orbitopathy: efficacy and morbidity. J Clin Endocrinol Metab 96:320–332
Tanda ML, Bartalena L (2012) Efficacy and safety of orbital radiotherapy for graves’ orbitopathy. J Clin Endocrinol Metab 97:3857–3865
Bartalena L, Fatourechi V (2014) Extrathyroidal manifestations of Graves’ disease: a 2014 update. J Endocrinol Invest 37:691–700
Piantanida E, Tanda ML, Lai A, Sassi L, Bartalena L (2013) Prevalence and natural history of Graves’ orbitopathy in the XXI century. J Endocrinol Invest 36:444–449
Marinó M, Morabito E, Brunetto MR, Bartalena L, Pinchera A, Marocci C (2004) Acute and severe liver damage associated with intravenous glucocorticoid pulse therapy in patients with Graves’ ophthalmopathy. Thyroid 14:403–406
Sisti E, Coco B, Menconi F, Leo M, Rocchi R, Latrofa F, Profilo MA, Mazzi B, Albano E, Vitti P, Marcocci C, Brunetto M, Marinò M (2014) Intravenous glucocorticoid therapy for Graves’ ophthalmopathy and acute liver damage: an epidemiological study. Eur J Endocrinol (in press)
Marinò M, Latrofa F, Menconi F, Chiovato L, Vitti P (2014) An update on the medical treatment of Graves’ hyperthyroidism. J Endocrinol Invest (in press)
Mourits MP, Prummel MF, Wiersinga WM, Koornneef L (1997) Clinical activity score as a guide in the management of patients with Graves’ ophthalmopathy. Clin Endocrinol (Oxf) 47:9–14
Bartalena L, Baldeschi L, Dickinson AJ, Eckstein A, Kendall-Taylor P, Marcocci C, Mourits MP, Perros P, Boboridis K, Boschi A, Currò N, Daumerie C, Kahaly GJ, Krassas G, Lane CM, Lazarus JH, Marinò M, Nardi M, Neoh C, Orgiazzi J, Pearce S, Pinchera A, Pitz S, Salvi M, Sivelli P, Stahl M, von Arx G, Wiersinga WM (2008) Consensus statement of the European group on Graves’ orbitopathy (EUGOGO) on management of Graves’ orbitopathy. Thyroid 18:333–346
Profilo MA, Sisti E, Marcocci C, Vitti P, Pinchera A, Nardi M, Rocchi R, Latrofa F, Menconi F, Altea MA, Leo M, Rago T, Marinò M (2013) Thyroid volume and severity of Graves’ orbitopathy. Thyroid 23:97–102
Menconi F, Marinò M, Pinchera A, Rocchi R, Mazzi B, Nardi M, Bartalena L, Marcocci C (2007) Effects of total thyroid ablation versus near-total thyroidectomy alone on mild to moderate Graves’ orbitopathy treated with intravenous glucocorticoids. J Clin Endocrinol Metab 92:1653–1658
Leo M, Marcocci C, Pinchera A, Nardi M, Megna L, Rocchi R, Latrofa F, Altea MA, Mazzi B, Sisti E, Profilo MA, Marinò M (2012) Outcome of Graves’ orbitopathy after total thyroid ablation and glucocorticoid treatment: follow-up of a randomized clinical trial. J Clin Endocrinol Metab 97:E44–E48
Moleti M, Violi MA, Montanini D, Trombetta C, Di Bella B, Sturniolo G, Presti S, Alibrandi A, Campennì A, Baldari S, Trimarchi F, Vermiglio F (2014) Radioiodine ablation of postsurgical thyroid remnants after treatment with recombinant human TSH (rhTSH) in patients with moderate-to-severe Graves’ orbitopathy (GO): a prospective, randomized, single-blind clinical trial. J Clin Endocrinol Metab 99:1783–1789
Wiersinga WM, Perros P, Kahaly GJ, Mourits MP, Baldeschi L, Boboridis K, Boschi A, Dickinson AJ, Kendall-Taylor P, Krassas GE, Lane CM, Lazarus JH, Marcocci C, Marino M, Nardi M, Neoh C, Orgiazzi J, Pinchera A, Pitz S, Prummel MF, Sartini MS, Stahl M, von Arx G (2006) Clinical assessment of patients with Graves’ orbitopathy: the European Group on Graves’ Orbitopathy recommendations to generalists, specialists and clinical researchers. Eur J Endocrinol 155:387–389
Marquez SD, Lum BL, McDougall IR, Katkuri S, Levin PS, MacManus M, Donaldson SS (2001) Long-term results of irradiation for patients with progressive Graves’ ophthalmopathy. Int J Radiat Oncol Biol Phys 51:766–774
Schaefer U, Hesselmann S, Micke O, Schueller P, Bruns F, Palma C, Willich N (2002) A long-term follow-up study after retro-orbital irradiation for Graves’ ophthalmopathy. Int J Radiat Oncol Biol 52:192–197
Bartalena L, Marcocci C, Chiovato L, Laddaga M, Lepri G, Andreani D, Cavallacci G, Baschieri L, Pinchera A (1983) Orbital cobalt irradiation combined with systemic corticosteroids for Graves’ ophthalmopathy: comparison with systemic corticosteroids alone. J Clin Endocrinol Metab 56:1139–1144
Marcocci C, Bartalena L, Bogazzi F, Bruno-Bossio G, Lepri A, Pinchera A (1991) Orbital radiotherapy combined with high dose systemic glucocorticoids for Graves’ ophthalmopathy is more effective than radiotherapy alone: results of a prospective randomized study. J Endocrinol Invest 14:853–860
Prummel MF, Mourits MP, Blank L, Berghout A, Koornneef L, Wiersinga WM (1993) Randomized double-blind trial of prednisone versus radiotherapy in Graves’ ophthalmopathy. Lancet 342:949–954
Marcocci C, Watt T, Altea MA, Rasmussen AK, Feldt-Rasmussen U, Orgiazzi J, Bartalena L, European Group of Graves’ Orbitopathy (2012) Fatal and non-fatal adverse events of glucocorticoid therapy for Graves’ orbitopathy: a questionnaire survey among members of the European Thyroid Association. Eur J Endocrinol 166:247–253
Bartley GB (2011) Rundle and his curve. Arch Ophthalmol 129:356–358
Perros P, Kendall-Taylor P (1998) Natural history of thyroid eye disease. Thyroid 8:423–425
Tanda ML, Piantanida E, Liparulo L, Veronesi G, Lai A, Sassi L, Pariani N, Gallo D, Azzolini C, Ferrario M, Bartalena L (2013) Prevalence and natural history of Graves’ orbitopathy in a large series of patients with newly diagnosed Graves’ hyperthyroidism seen at a single center. J Clin Endocrinol Metab 98:1443–1449
Menconi F, Profilo MA, Leo M, Sisti E, Altea MA, Rocchi R, Latrofa F, Nardi M, Vitti P, Marcocci C, Marinò M (2014) Spontaneous improvement of untreated mild Graves’ ophthalmopathy: Rundle’s curve revisited. Thyroid 24:60–66
Eckstein A, Esser J, Mann K, Schott M (2010) Clinical value of TSH receptor antibodies measurement in patients with Graves’ orbitopathy. Pediatr Endocrinol Rev 7(Suppl 2):198–203
Acknowledgments
Supported by a Grant from MIUR (Ministero dell’Istruzione, dell’Università e della Ricerca Scientifica) (2004068078 to MM).
Conflict of interest
Eleonora Sisti, Francesca Menconi, Marenza Leo, Maria Antonietta Profilo, Teresa Mautone, Barbara Mazzi, Roberto Rocchi, Francesco Latrofa, Marco Nardi, Paolo Vitti, Claudio Marcocci and Michele Marinò declare that they do not have any commercial association or other associations that might create a conflict of interest in connection with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sisti, E., Menconi, F., Leo, M. et al. Long-term outcome of Graves’ orbitopathy following high-dose intravenous glucocorticoids and orbital radiotherapy. J Endocrinol Invest 38, 661–668 (2015). https://doi.org/10.1007/s40618-015-0241-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-015-0241-7