Abstract
Introduction
We describe the use of contrast-enhanced ultrasound (CEUS) in the diagnosis of delayed splenic vascular injury (DSVI) and active extravasation (DAE) during spleen injury follow-up. CEUS might be used instead of contrast-enhanced computed tomography (CECT) during spleen injury follow-up in order to reduce radiation exposure.
Objective
Assess diagnostic comparability between CEUS and CECT in the evaluation of DSVI and DAE during spleen injury follow-up.
Subjects and methods
A total of 139 trauma patients (101 males, 38 females; mean age 48.6 years) with CECT diagnosed spleen injury were prospectively evaluated. They performed CEUS and CECT follow-up. All CEUS studies were performed using the same ultrasound scan, convex probe, mechanical index and ultrasound contrast agent dose. Twelve patients performed digital subtraction angiography (DSA) during follow-up, and the diagnostic performance comparability between CEUS and DSA was evaluated.
Results
CEUS showed 17 delayed spleen injury complications, and in 122 patients no complication was suspected. CECT diagnosed 16 delayed spleen injury complications in these 17 patients and showed a small DSVI in another patient. A total of 122 follow-up CT scans were negative. CEUS and CECT diagnostic comparability was 98.6%. Compared to DSA, CEUS showed a sensitivity of 100% and a positive predictive value of 91.7%.
Conclusions
CEUS can be used during spleen injury follow-up instead of CECT. Positive CEUS examinations could perform CECT and, when necessary, DSA in order to confirm and treat spleen injury complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The spleen is the second most frequent organ involved in blunt abdominal trauma (13%) after the liver (16%) [1]. Delayed splenic vascular injury (DSVI) and delayed active extravasation (DAE) are reported to occur, respectively, in 3–23% and 1.5% of blunt splenic injuries (BSI) [2,3,4,5]. Non-operative management (NOM) of blunt splenic trauma is the treatment of choice for hemodynamically stable patients in an optimal setting in which monitoring and frequent clinical evaluations are possible, and an operating room is available for urgent laparotomy. The advantages of NOM of spleen injuries are well recognized. NOM allows the preservation of spleen role in immune system, reducing the risk of future infections, the most serious of which are part of the overwhelming post-splenectomy infection (OPSI) syndrome. It avoids a hypercoagulable state and thromboembolic complications, and it allows earlier discharge and a costs reduction [6]. Moreover, a previous study demonstrated that preserving the spleen allows a reduction in cancer incidence [7]. Delayed splenic rupture is a life-threatening injury complication, and it is thought that it could be related to the rupture of a pseudoaneurysm (PSA), clot disruption or expansion of a subcapsular hematoma [4, 8, 9]. There are different classifications of spleen trauma injury grade; the American Association for the Surgery of Trauma (AAST)—spleen Injury Scale (SIS) is the most used [10] (Table 1). According to the Western Trauma Association (WTA) algorithm, in all patients with AAST-SIS grade II or higher-grade injuries a repeat imaging may be considered before hospital discharge to rule out PSA formation [11].
Conventional ultrasound (US), contrast-enhanced ultrasound (CEUS) and CT are used to assess patients with blunt abdominal trauma. Conventional US is generally used in the early assessment of polytrauma patients in order to assess intra-abdominal free fluid, a technique known as focused assessment with sonography for trauma (FAST). However, the literature provides evidence of the low US sensitivity in diagnosing spleen injury [12]. In adult patients, CT is the most used imaging modality in spleen injury follow-up, but CEUS is a promising alternative imaging modality in this field [13]. According to EFSUMB guidelines, CEUS can be used in the follow-up of conservatively managed abdominal trauma to reduce the number of CT examinations, particularly in children [14]. According to the World Society of Emergency Surgery (WSES) guidelines, CT scan repetition during the admission should be considered in adult patients with an initial diagnosis of moderate lesions (hemodynamically stable AAST-SIS grade III-V lesions) as well as when there is lowering hematocrit levels, vascular anomalies, underlying splenic pathology or coagulopathy, and in neurologically impaired patients. In the last three situations, additional CT follow-up is suggested after discharge. According to the same guidelines, CEUS follow-up seems reasonable to minimize the risk of life-threatening hemorrhage and associated complications in children [15]. During spleen injury follow-up, two main complications could develop: DAE and DSVI [16,17,18]. DSVI are splenic-contained vascular injuries, and consist of pseudoaneurysm (PSA) and post-traumatic arteriovenous fistula (AVF): These two entities are usually indistinguishable by means of CEUS or CT [19,20,21]. Previous studies showed that CEUS detection rate for active extravasation was not different from that of contrast-enhanced CT [16, 22]. Another study demonstrated a high sensitivity (83%) and specificity (92%) of CEUS at detection of post-traumatic liver and splenic PSA in the pediatric population [23].
To our knowledge, no previous study evaluated CEUS diagnostic performance in diagnosing DSVI and DAE in adult patients with serial CEUS examinations during follow-up.
The study aim was to assess diagnostic comparability between CEUS and CECT in the evaluation of DSVI and DAE during spleen injury follow-up.
Subjects and methods
Patient population
During the 2 years period 2016–2017, 824 hemodynamically stable trauma patients without diffuse peritonitis underwent contrast-enhanced CT (CECT) in our emergency department. A prospective study was performed in 144 consecutive patients who had a CECT diagnosed spleen injury at the emergency department. Three minor patients were excluded, as well as two patients who could not undergo CECT during follow-up due to prior allergic reaction to iodinated contrast agents. The study population consisted, therefore, of 139 adult patients (101 males; 38 females; M:F 2.7:1; mean age 48.6 years, range 18–86) who underwent CEUS and CECT follow-up between January 2016 and December 2017.
The study was approved by the institutional review board and ethics committee of our institution. Informed consent was obtained from all individual participants included in the study.
CEUS technique
CEUS follow-up consisted of one-to-eight (mean 4.7) serial examinations at 1–3–7–15–30–60–90–180 days (± 1 day) after trauma until spleen injury became no more visible. CEUS examinations were performed using iU22 Philips, 1–5 MHz convex probe, with Mechanical Index = 0.08, and 2.4-ml sulfur hexafluoride injection (SonoVue, Bracco, Milan, Italy), followed by a 10 ml saline flush. Left intercostal scanning was performed with the focus set to the deepest level of the spleen. CEUS were performed with continuous image acquisition, starting immediately after contrast injection and lasting 5 min.
CT technique
All the 139 patients underwent a CECT examination between 3 and 7 days after trauma. CECT examination was performed using a 16-slice CT (Philips Brilliance), with arterious, venous and delayed post-contrast images after intravenous injection of 90–120 ml iopamidol 370 mg I/ml (Iopamiro 370, Bracco, Milan, Italy) with an electronic power injector (Stellant; Medrad) at a flow rate of 3 ml/s.
Image assessment
Two radiologists, with more than 10 years experience in CEUS and CECT abdominal imaging, evaluated in consensus CEUS and CECT images in order to detect a DSVI or a DAE. Active bleeding was suspected when CEUS showed a hyperechoic irregular or round spot or fountain-like jet in the arterial and late parenchymal phases. Active bleeding was diagnosed by CT when a hyperdense spot of contrast enhancement tended to increase in size in portal venous phase. DSVI was suspected by CEUS when a hyperechoic round or oval area showed distinct margins in arterial phase. DSVI was diagnosed by CT when a hyperdense round or oval area of contrast enhancement with distinct margins in arterial phase did not increase in size in portal venous phase. In the thirteen patients eligible for interventional procedures, DSA images, considered as the standard of reference, were reviewed by an experienced interventional radiologist (with 10 years of experience in interventional radiology), who was unaware of the CEUS and CECT findings. DSA diagnosis was compared with that made using CEUS to assess the two modalities comparability.
Statistical analysis
In the 139 patients included in the study, CEUS diagnosis was compared with CECT one, and diagnostic performance comparability was assessed. In the thirteen patients who underwent DSA, CEUS diagnosis was compared with DSA one, and sensitivity and positive predictive value were evaluated.
Results
Patients characteristics
According to the AAST-SIS classification of splenic trauma, in the first CT performed in the emergency department were found 51 (36.7%) grade I, 45 (32.4%) grade II, 37 (26.6%) grade III and 6 grade IV (4.3%).
No patient died from splenic injury related complications.
Diagnostic performance comparability of CEUS to CECT
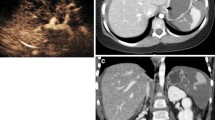
CEUS showed 17 delayed splenic injury complications, 12 DSVI and 5 DAE. In 122 patients, CEUS did not show complication. CECT diagnosed 16 delayed spleen injury complications in these 17 patients (12 DSVI and 4 DAE); CECT diagnosed a small DSVI (2 mm of maximum diameter) in another patient. A total of 122 follow-up CT scans were negative. CEUS and CECT diagnostic comparability was 98.6% (Figs. 1, 2, 3).
Diagnostic performance comparability of CEUS to DSA
Thirteen patients with CEUS diagnosed delayed splenic injury complication performed DSA, 12 with DSVI and 1 with DAE. DSA confirmed 12 delayed splenic injury complications, 11 DSVI and 1 DAE. Considering DSA as the gold standard, CEUS showed a sensitivity of 100% and a positive predictive value of 92.3% (Fig. 4).
Discussion
CEUS spleen injury follow-up in adult patients is considered a promising imaging modality [10]. Previous studies showed that CEUS can detect active bleeding [16, 22] or demonstrated the usefulness of performing one or two CEUS during follow-up [24, 25]. Some other studies reported the usefulness of performing a follow-up CT scan 48 or 72 h after admission in patients with grade ≥ II in order to diagnose a possible PSA development [4, 25, 26].
In the present study, all delayed splenic injury complications were diagnosed in the first 7 days after trauma, and none occurred in AAST-SIS grade I spleen injuries. This study demonstrate that CEUS is a valuable imaging modality that could be performed during splenic injury follow-up; in fact, splenic injury complications could be promptly diagnosed and embolized before a splenectomy would be necessary. This is particularly useful during the first 7 days after trauma in patients with AAST-SIS grade ≥ II, when complications are more probably to occur [9]. According to a recent literature review, routine imaging follow-up CT scans may not be indicated in asymptomatic patients with lower grade blunt splenic injuries in order to avoid a lot of unuseful CT scans [13]. It is widely recognized that CT is the best imaging modality in adult patients with blunt abdominal trauma to be performed in the emergency department. However, CEUS could replace CT as a follow-up imaging modality in patients who need to reevaluate splenic injuries. CEUS is a radiation-free imaging modality, and it is noteworthy taking into account that spleen injury often occurs in young adults and middle-aged adults. CEUS allows to perform serial spleen injury evaluation at short time intervals, and our study results strongly support the use of CEUS as a follow-up imaging modality of splenic injury. In fact CEUS is safe, relatively cheap, and can be performed at the patient’s bedside in critical-ill patients, such as in intensive care unit (ICU) ones. Spleen injury complications could occur at any time—particularly in the first seven days after trauma—but they are not so frequent to justify several CT scans. Therefore, we could affirm that CEUS could fill a gap in diagnostic imaging, and that it could represent the reference imaging modality in splenic injury follow-up. We do not have the haughtiness to think that the study cohort could be the representative of all the patient cohorts in other hospitals, but we think that the use of an imaging modality like CEUS could be used at least in the first seven days after trauma in patients with AAST-SIS grade ≥ II at pre-established intervals (e.g., 1–3–7 days after trauma) in order to diagnose DSVI and DAE, and to reduce CT scans.
This study has some limitations: It is a single-institute analysis, and the study population is small. However, to our knowledge, this is the first study which evaluated CEUS efficacy in diagnosing DSVI and DAE with respect to CT and DSA performing many serial CEUS examinations.
References
Raza M, Abbas Y, Devi V, Prasad KV, Rizk KN, Nair PP (2013) Non operative management of abdominal trauma—a 10 years review. World J Emerg Surg 8:14
Weinberg JA, Magnotti LJ, Croce MA, Edwards NM, Fabian TC (2007) The utility of serial computed tomography imaging of blunt splenic injury: still worth a secondlook? J Trauma 5:1143–1147; discussion 1147–8
Weinberg JA, Lockhart ME, Parmar AD et al (2010) Computed tomography identification of latent pseudoaneurysm after blunt splenic injury: pathology or technology? J Trauma 68:1112–1116
Furlan A, Tublin ME, Rees MA, Nicholas DH, Sperry JL, Alarcon LH (2017) Delayed splenic vascular injury after nonoperative management of blunt splenic trauma. J Surg Res 211:87–94
Leeper WR, Leeper TJ, Ouellette D et al (2014) Delayed hemorrhagic complications in the nonoperative management of blunt splenic trauma: early screening leads to a decrease in failure rate. J Trauma Acute Care Surg 76:1349–1353
Stassen NA, Bhullar I, Cheng JD, Eastern Association for the Surgery of Trauma et al (2012) Selective nonoperative management of blunt splenic injury: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg 73:S294–S300
Sun LM, Chen HJ, Jeng LB, Li TC, Wu SC, Kao CH (2015) Splenectomy and increased subsequent cancer risk: a nationwide population-based cohort study. Am J Surg 210:243–251
Anyanwu CT, Reynal SD (2018) Delayed splenic rupture resulting in massive intraperitoneal hemorrhage post ambulatory-related injury. Cureus 10:e2160
Freiwald S (2010) Late-presenting complications after splenic trauma. Perm J 14:41–44
Moore EE, Cogbill TH, Jurkovich GJ, Shackford SR, Malangoni MA, Champion HR (1995) Organ injury scaling: spleen and liver (1994 revision). J Trauma 38:323–324
Rowell SE, Biffl WL, Brasel K et al (2017) Western trauma association critical decisions in trauma: management of adult blunt splenic trauma-2016 updates. J Trauma Acute Care Surg 82:787–793
Valentino M, Serra C, Zironi G, De Luca C, Pavlica P, Barozzi L (2006) Blunt abdominal trauma: emergency contrast-enhanced sonography for detection of solid organ injuries. AJR Am J Roentgenol 186:1361–1367
Mebert RV, Schnüriger B, Candinas D, Haltmeier T (2018) Follow-up imaging in patients with blunt splenic or hepatic injury managed nonoperatively. Am Surg 84:208–214
Sidhu PS, Cantisani V, Dietrich CF et al (2018) The EFSUMB guidelines and recommendations for the clinical practice of contrast-enhanced ultrasound (CEUS) in non-hepatic applications: update 2017 (long version). Ultraschall Med 39:e2–e44. https://doi.org/10.1055/a-0586-1107
Coccolini F, Montori G, Catena F et al (2017) Splenic trauma: WSES classification and guidelines for adult and pediatric patients. World J Emerg Surg 12:40
Lv F, Tang J, Luo Y et al (2011) Contrast-enhanced ultrasound imaging of active bleeding associated with hepatic and splenic trauma. Radiol Med 116:1076–1082
Marmery H, Shanmuganathan K, Mirvis SE et al (2008) Correlation of multidetector CT findings with splenic arteriography and surgery: prospective study in 392 patients. J Am Coll Surg 206:685–693
Hamilton JD, Kumaravel M, Censullo ML, Cohen AM, Kievlan DS, West OC (2008) Multidetector CT evaluation of active extravasation in blunt abdominal and pelvic trauma patients. Radiographics. 28:1603–1616
Boscak AR, Shanmuganathan K, Mirvis SE et al (2013) Optimizing trauma multidetector CT protocol for blunt splenic injury: need for arterial and portal venous phase scans. Radiology 268:79–88
Graves JA, Hanna TN, Herr KD (2017) Pearls and pitfalls of hepatobiliary and splenic trauma: what every trauma radiologist needs to know. Emerg Radiol 24:557–568
Miele V, Piccolo CL, Galluzzo M, Ianniello S, Sessa B, Trinci M (2016) Contrast-enhanced ultrasound (CEUS) in blunt abdominal trauma. Br J Radiol 89:20150823
Catalano O, Sandomenico F, Raso MM, Siani A (2005) Real-time, contrast-enhanced sonography: a new tool for detecting active bleeding. J Trauma 59:933–939
Durkin N, Deganello A, Sellars ME, Sidhu PS, Davenport M, Makin E (2016) Post-traumatic liver and splenic pseudoaneurysms in children: diagnosis, management, and follow-up screening using contrast enhanced ultrasound (CEUS). J Pediatr Surg 51:289–292
Brillantino A, Iacobellis F, Robustelli U et al (2016) Non operative management of blunt splenic trauma: a prospective evaluation of a standardized treatment protocol. Eur J Trauma Emerg Surg 42:593–598
Tugnoli G, Bianchi E, Biscardi A et al (2015) Nonoperative management of blunt splenic injury in adults: there is (still) a long way to go. The results of the Bologna–Maggiore Hospital trauma center experience and development of a clinical algorithm. Surg Today 45:1210–1217
Morrison CA, Gross BW, Kauffman M, Rittenhouse KJ, Rogers FB (2017) Overview of nonoperative blunt splenic injury management with associated splenic artery pseudoaneurysm. Am Surg 83:554–558
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no potential conflicts of interests associated with this study.
Ethical standard
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Tagliati, C., Argalia, G., Polonara, G. et al. Contrast-enhanced ultrasound in delayed splenic vascular injury and active extravasation diagnosis. Radiol med 124, 170–175 (2019). https://doi.org/10.1007/s11547-018-0961-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-018-0961-9