Abstract
Purpose
The advantages of the conservative approach for major spleen injuries are still debated. This study was designed to evaluate the safety and effectiveness of NOM in the treatment of minor (grade I-II according with the American Association for the Surgery of Trauma; AAST) and severe (AAST grade III-V) blunt splenic trauma, following a standardized treatment protocol.
Methods
All the hemodynamically stable patients with computer tomography (CT) diagnosis of blunt splenic trauma underwent NOM, which included strict clinical and laboratory observation, 48–72 h contrast-enhanced ultrasonography (CEUS) follow-up and splenic angioembolization, performed both in patients with admission CT evidence of vascular injuries and in patients with falling hematocrit during observation.
Results
87 patients [32 (36.7 %) women and 55 (63.2 %) men, median age 34 (range 14–68)] were included. Of these, 28 patients (32.1 %) had grade I, 22 patients (25.2 %) grade II, 20 patients (22.9 %) grade III, 11 patients (12.6 %) grade IV and 6 patients (6.8 %) grade V injuries. The overall success rate of NOM was 95.4 % (82/87). There was no significant difference in the success rate between the patients with different splenic injuries grade. Of 24 patients that had undergone angioembolization, 22 (91.6 %) showed high splenic injury grade. The success rate of embolization was 91.6 % (22/24). No major complications were observed. The minor complications (2 pleural effusions, 1 pancreatic fistula and 2 splenic abscesses) were successfully treated by EAUS or CT guided drainage.
Conclusions
The non operative management of blunt splenic trauma, according to our protocol, represents a safe and effective treatment for both minor and severe injuries, achieving an overall success rate of 95 %. The angiographic study could be indicated both in patients with CT evidence of vascular injuries and in patients with high-grade splenic injuries, regardless of CT findings.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Trauma is the first cause of death in people younger than 40 years in western countries and constitutes a relevant clinical problem [1, 2].
Spleen represents the most commonly damaged organ during abdominal blunt trauma and is affected in about one-third of patients with traumatic abdominal injuries [3–8].
Until the middle of the past century, early splenectomy represented the gold standard treatment for blunt splenic injuries. This operative approach was based on the concept that spleen does not play essential functions for life and consists of a highly vascularized parenchyma that may cause uncontrollable bleeding, if not surgically removed, even in case of minor lesions [9–12].
Gradually, due to the increased knowledge of spleen immunological functions, the advanced accuracy of diagnostic imaging and the improvement of interventional radiology techniques, the conservative approach was encouraged and examined [13–22].
At present, the non operative management (NOM) is considered the standard treatment for minor splenic trauma (grades I-II according to the American Association for the Surgery of Trauma-AAST) [23], whereas the advantages of the conservative approach for major spleen injuries (AAST grades III-V) are still debated [4, 13].
This study was designed to evaluate the safety and effectiveness of NOM in the treatment of minor (AAST grade I-II) and severe (AAST grade III-V) blunt splenic trauma, following a standardized treatment protocol, including clinical observation and splenic angioembolization, according with the relevant literature and our own hospital resources.
Methods
From January 2009 to January 2014, all the patients with polytrauma referring to the Emergency Department and Trauma Center of the “A. Cardarelli” hospital were inserted in a prospective database, including the results of clinical and instrumental evaluation and any subsequent conservative or surgical treatment. For each patient, the demographic characteristics (age, gender, mechanism of injury), the Revised Trauma Score (RTS), the Glasgow Coma scale (GCS) and the Injures Severity Score (ISS) were recorded [24].
Among the referred patients were considered for the enrollment in this study all the subjects with blunt thoracoabdominal trauma.
These last, after clinical evaluation according to the Advanced Trauma Life Support (ATLS®) underwent initial instrumental study with FAST (focused assessment with sonography for trauma) and chest and pelvis x-ray [25].
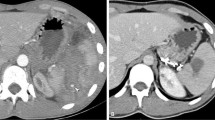
Then, the hemodynamically stable patients (systolic blood pressure ≥90 mmHg, heart rate <100 bpm) and the hemodynamically stabilized patients (returned to normal vital signs after 1000 ml crystalloid infusion) were investigated with a total body CT (Computer Tomography) scan examination.
Basing on the clinical and instrumental evaluation, from all the enrolled patients, were included in this study the adults subjects (14 years or more), with initial hemodynamic stability or good response to 1000 ml crystalloid prompt infusion and CT evidence of I–V grade spleen injury according with AAST. The patients with associated significant hemoperitoneum at CT (defined as intra abdominal blood extended to at least two abdominal quadrants) were also included.
All the patients receiving systemic anticoagulation, with diffuse peritonitis and with associated bowel injuries (pneumoperitoneum) or any other concomitant thoracoabdominal lesions requiring surgical procedure, were excluded.
All the included patients were admitted to the trauma center and underwent NOM.
Non operative management protocol
The non operatively managed patients underwent arterial blood gas measurements every 12 h and complete blood cell counts every 6 h, until two stable hemoglobin examinations were obtained [26]. Both activity and oral diet were liberalized after obtaining two consecutive hemoglobin stable measurement. A contrast-enhanced ultrasound (CEUS) follow-up was performed 48–72 h after injury.
All the patients with admission CT evidence of vascular injures (contrast extravasation, pseudo-aneurysm, arteriovenous fistula formation, vessel truncation), as well as the patients with progressive fall of the hemoglobin level despite the absence of vascular injures CT signs, underwent splenic angiography and, if indicated, angioembolization.
Postembolization clinical and instrumental follow-up was similar to the patients undergone conservative treatment; in case of falling serial hemoglobin level the angiography was repeated and re-embolization performed.
NOM was considered unsuccessful if, during observation, the following conditions occurred: hemodynamic instability, progressive fall in hemoglobin level despite two angioembolizations, diffuse peritonitis or detection of missed abdominal injuries requiring surgery.
NOM was considered successful when the patient was discharged with the spleen in situ.
Angioembolization technique
Splenic angiography was performed by an experienced interventional radiologist through the common femoral artery access.
The splenic artery and splenic artery branche catheterization were obtained using, respectively, a 4–5 Fr catheter and coaxial micro-catheters.
The presence of diffuse splenic bleeding and multiple focal bleeding vessels constituted the indication for proximal embolization by means of metallic coils.
Selective distal coil or particle embolization was performed in patients with one or few focal bleeding splenic vessels [8].
Statistical analysis
Statistical analysis was carried out using the program InStat Graph-Pad Prism® 5 (San Diego, California, USA).
Values are expressed as mean ± standard deviation (SD) or medians (range). Continuous data were compared between each group using the Mann–Whitney U test, according with distribution of data.
Prevalence data were compared between groups using the Fisher’s exact test.
A probability value of less than 0.05 was considered significant.
Results
Study population
Among all the patients with blunt trauma observed during the study period, 128 were admitted with diagnosis of splenic injury.
Of these, 41 patients (32 %) underwent operative management. The indications for surgery were the presence of persisting hemodynamic instability despite fluid therapy in 75.6 % (31/41), diffuse peritonitis in 19.5 % (8/41) and coexisting thoracoabdominal injuries requiring surgical procedure in 14.6 % (6/41) of cases. Two patients with diffuse peritonitis and hemoperitoneum (25 %) had splenomegaly due to hematologic disorders. These last underwent angioembolization prior to surgery, to stop bleeding and facilitate splenectomy. Among the hemodynamically unstable patients, 5 (16.1 %) were under systemic anticoagulation therapy.
Out of patients with blunt splenic trauma, 87 (68 %) [32 (36.7 %) women and 55 (63.2 %) men, median age 34 (range 14–68)] satisfied selection criteria, were included in the study and constituted the object of analysis.
The Table 1 shows the demographic characteristics and trauma severity of the included patients.
The main causes of injury were motor-vehicle collisions (56.3 %), physical aggressions (24.1 %), pedestrians struck (11.4 %) and falls from height (8.2 %).
According with AAST organ injury scale, 28 patients (32.1 %) had grade I, 22 patients (25.2 %) grade II, 20 patients (22.9 %) grade III, 11 patients (12.6 %) grade IV and 6 patients (6.8 %) grade V injuries.
Twenty-two patients (18/87 = 20.6 %) presented isolated splenic trauma whereas the remaining 69 patients (69/87 = 79.3 %) showed multiple injuries. Among these last patients, hepatic injury was observed in 5.8 % (4/69), adrenal injury in 2.8 % (2/69), renal injury in 4.3 % (3/69), mesothelium hematoma in 4.3 % (3/69), rib fractures in 52.1 % (36/69), hemothorax in 8.6 % (6/69), vertebral fractures in 8.6 % (6/69), pelvic fractures in 7.2 % (5/69) and traumatic brain injuries in 10.1 % (7/69) of cases.
Clinical outcome
Sixty-nine patients (69/87 = 79.3 %) [30 with grade I, 19 grade II, 11 grade III, 7 grade IV and 2 grade V injuries (mean injury grade = 2 ± 1.1)] did not show vascular injury signs on admission CT and underwent, according with study protocol, observation with serial clinical, radiological and laboratory examination. Out of these, 8 subjects (8/69 = 11.5 %) (1 with grade II, 2 grade III, 3 grade IV and 2 grade V injuries) showed, during hospitalization, progressive fall of hemoglobin level.
Among these last, 2 patients (2/8 = 25 %) with grade II and III injuries showed, on the third day, hemodynamic worsening and a ruptured sub capsular splenic hematoma associated with disseminated hemoperitoneum at follow-up CEUS; consequently they underwent emergency splenectomy.
The remaining six patients (6/8 = 75 %) with high grade injuries and falling serial hemoglobin during observation underwent splenic angiography with subsequent therapeutic embolization for the presence of angiographic extravasation; no NOM failure was observed in this patients group.
Eighteen patients (18/87 = 20.4 %) [2 with grade II, 9 grade III, 3 grade IV and 4 grade V injuries (mean injury grade = 3.31 ± 0.9)] showed admission CT findings of vascular injuries and underwent primary angioembolization.
The indications for embolization were pseudo-aneurysm, intraparenchymal contrast blush, intraperitoneal contrast blush, both intraparenchymal and intraperitoneal contrast blush in 22.2 % (4/18), 33.3 % (6/18), 27.7 % (5/18) and 16.6 % (3/18) of cases, respectively.
Out of these, 3 subjects (1 with grade IV and 2 with grade V injuries) (3/18 = 16.6 %), while maintaining hemodynamic stability during hospitalization, showed decrease of hemoglobin level and, consequently, underwent a second look angiography. Among these last, 1 (33.3 %) patient with rebleeding after distal particle embolization was successfully treated with subsequent proximal embolization. The two (66.6 %) remaining patients showed persistent multiple focal bleeding splenic vessels despite received proximal embolization. In these two cases, due to the inaccessibility of splenic artery, a more selective embolization was not possible, and emergency splenectomy was performed.
The overall success rate of NOM was 95.4 % (83/87). There was no significant difference in the success rate between the patients with different splenic injuries grade (Table 2).
The success rate in patients that underwent embolization was 91.6 % (22/24), without showing significant difference between patients with different injuries grade. Particularly, splenic angiography and subsequent embolization were performed in 24 patients (24/87 = 27.5 %) (2/20 with grade II, 10/20 grade III, 6/11 grade IV and 6/6 grade V injuries) and failed in 2 patients (9.4 %) with grade IV and V injuries.
There was no significant difference in the success rate between patients with CT finding of significant and not significant hemoperitoneum [90.3 % (28/31) vs 98.2 % (55/56): p = 0.127; Fisher’s exact test].
The median of blood transfusions was significantly different between patients with minor (AAST grade I–II) and severe (AAST grade III–V) trauma [0.5 (0–2) vs 2 (0–4): p = 0.0023; Mann–Whitney U test].
The overall median hospital stay was 4 days (4–10). No significant difference in the median hospitalization period was found between patients with minor and sever splenic trauma [4 (4–10) vs 5 (4–10): p = 0.057; Mann–Whitney U test]. No mortality was observed.
The median follow-up period in the included patients was 24 months (6–36). No major complications or delayed failures were observed. Minor complications included 2 cases of pleural effusions and 1 case of pancreatic fistula due to a missed pancreatic contusion in the observation group and 2 cases of splenic abscesses in the embolization group. These complications were successfully treated by EAUS or CT guided drainage and did not require surgery. No one case of symptomatic splenic infarct, late pseudo-aneurism, splenic pseud-ocyst or main coil migration was noted.
Discussion
The nonoperative management, first routinely used in children with success rate of 75–93 %, has become the standard initial treatment for blunt splenic trauma in hemodynamically stable patients [4, 27, 28].
The surgical treatment, considered mandatory for splenic trauma until the sixties, remains still indicated in unstable patients and in case of NOM failure [28].
Despite the wide diffusion of non operative management, and its value in high-grade injuries, the utility of adding angiography and the impact of angioembolization still represent matters of debate.
Although we employed for many years the non operative management for treatment of blunt splenic trauma, in this study we reported the results of a 5-year NOM experience using a standardized treatment protocol, developed on the base of existing literature, our experience and our own hospital resources.
According to other Authors [28], in our protocol the main indication to the NOM was the hemodynamic stability, regardless of the injuries’ grade and the amount of hemoperitoneum. Conversely, the patients with pneumoperitoneum, diffuse peritonitis and concomitant lesions requiring surgery were excluded.
Despite the definition of hemodynamic stability varies greatly in the literature [13], we chose 90 mmHg systolic blood pressure both as discriminating cut off and as endpoint for fluid resuscitation in blunt trauma, according to the principles of hypotensive resuscitation and the recent european guidelines [29, 30].
Basing on previous studies [31] and according to a recent consensus conference among 30 surgeons and interventional radiologists experts [32], angioembolization was reserved for hemodynamically stable patients with CT findings of vascular injuries and for patients with negative admission CT scan and diminished hematocrit during observation, to detect the delayed and missed vascular injuries [26, 33].
In order to avoid radiations repeated exposure, the instrumental follow-up was performed by means CEUS that seems to show a similar sensitivity and specificity in detecting post traumatic lesions, if compared with CT [34].
Finally, the emergence of hemodynamic instability and the progressive fall of hemoglobin despite two angioembolization attempts were considered the main criteria for NOM failure [26].
Our study shows, first of all, that the non operative management, performed according with our protocol, represents a safe and effective treatment option for blunt splenic trauma. Indeed, the overall success rate was about 95 %, no mortality or major complications were observed and the reported minor complications did not require surgery.
According to other Authors [26], although the success rate was lower in the subjects with high-grade injury, no significant difference in this parameter was found between patients with different injury grade.
In contrast to other Authors [27], and according to Haan et al. [26], the presence of significant hemoperitoneum did not represent a marker of treatment failure.
In our series, the impact of interventional radiology was considerable since more than a quarter of patients needed angioembolization. This procedure showed a high success rate (91 %) without complications related to the catheterization technique.
Interestingly, 91.7 % of patients underwent angioembolization and all the patients requiring angioembolization for decreased hemoglobin despite no CT evidence of vascular lesions showed high splenic injury grade.
These data seem to show, according to other Authors [26, 33], that in patients with high injury grade, the absence of contrast blush at CT scan should not preclude angioembolization and, especially in patients with IV and V injury grade, the use of angiography should be encouraged, regardless of CT findings.
According to our treatment protocol, in patients without CT evidence of vascular injuries, the choice of perform angiography was guided by strict clinical and laboratory observation and no morbidity or NOM failure was observed in this patients group.
However, other trials with larger series are needed to define if the choice of perform a “delayed” vs a “primary” angiography in patients with high splenic injury grade could result in an increased hospital stay and worse clinical outcome. In conclusion, our data show that the nonoperative management of blunt splenic trauma, according to our protocol, represents a safe and effective treatment for both minor (AAST grade I–II) and severe (AAST grade III–V) injuries, achieving an overall success rate of 95 %. The angiographic study could be indicated both in patients with CT evidence of vascular injuries and in patients with high-grade splenic injuries, regardless of CT findings.
Abbreviations
- NOM:
-
Non operative management
- AAST:
-
American association for the surgery of trauma
- CT:
-
Computer tomography
- CEUS:
-
Contrast enhanced ultrasonography
- FAST:
-
Focused assessment sonography for trauma
References
Gaines BA. Intra-abdominal solid organ injury in children: diagnosis and treatment. J Trauma. 2009;67:S135–9.
Sauaia A, Moore FA, Moore EE, Moser KS, Brennan R, Read RA. Pons PT epidemiology of trauma deaths: a reassessment. J Trauma. 1995;38(2):185–93.
Smith J, Caldwell E, D’Amours S, Jalaludin B, Sugrue M. Abdominal trauma: a disease in evolution. ANZ J Surg. 2005;75(9):790–4.
Hancock GE, Farquharson AL. Management of splenic injury. J R Army Med Corps. 2012;158(4):288–98.
Dupuy DE, Raptopoulos V, Fink MP. Current concepts in splenic trauma. J Intensive Care Med. 1995;10(2):76–90.
Akinkuole AA, Lawal OO, Arowolo OA, Agbakwuru EA, Adesunkanmi ARK. Determinants of splenectomy in splenic injuries following blunt abdominal trauma. S Afr J Surg. 2010;48(1):15–9.
Costa G, Tierno SM, Tomassini F, Venturini L, Frezza B, Cancrini G, Stella F. The epidemiology and clinical evaluation of abdominal trauma. An analysis of a multidisciplinary trauma registry. Ann Ital Chir. 2010;81:95–102.
van der Vlies CH, Hoekstra J, Ponsen KJ, Reekers JA, van Delden OM, Goslings JC. Impact of splenic artery embolization on the success rate of nonoperative management for blunt splenic injury. Cardiovasc Intervent Radiol. 2012;35:76–81.
Cirocchi R, Corsi A, Castellani E, Barberini F, Renzi C, Cagini L, Boselli C, Noya G. Case series of non-operative management vs. operative management of splenic injury after blunt trauma. Ulus Travma Acil Cerrahi Derg. 2014;20(2):91–6. doi:10.5505/tjtes.2014.99442.
Shakford SR, Molin MR. Management of splenic injuries. Surg Clin North Am. 1990;70:595–620.
Pachter HL, Guth AA, Hofstetter SR, Spencer FC. Changing patterns in the management of splenic trauma. Ann Surg. 1998;227:708–19.
Clancy AA, Tiruta C, Ashman D, Ball CG, Kirkpatrick AW. The song remains the same although the instruments are changing: complications following selective nonoperative management of blunt spleen trauma: a retrospective review of patients at a level I trauma centre from 1996 to 2007. J Trauma Manag Outcomes. 2012;6:4.
Cirocchi R, Boselli C, Corsi A, Farinella E, Listorti C, Trastulli S, Renzi C, Desiderio J, Santoro A, Cagini L, Parisi A, Redler A, Noya G, Fingerhut A. Is non-operative management safe and effective for all splenic blunt trauma? A systematic review. Crit Care. 2013;17(5):R185. doi:10.1186/cc12868.
Dent D, Alsabrook G, Erickson BA, Myers J, Wholey M, Stewart R, Root H, Ferral H, Postoak D, Napier D, Pruitt BA Jr. Blunt splenic injuries: high nonoperative management rate can be achieved with selective embolization. J Trauma. 2004;56:1063–7.
Gaarder C, Dormagen JB, Eken T, Skaga NO, Klow NE, Pillgram-Larsen J, Buanes T, Naess PA. Nonoperative management of splenic injuries: improved results with angioembolization. J Trauma. 2006;61:192–8.
Malhotra AK, Carter RF, Lebman DA, Carter DS, Riaz OJ, Aboutanos MB, Duane TM, Ivatury RR. Preservation of splenic immunocompetence after splenic artery angioembolization for blunt splenic injury. J Trauma. 2010;69:1126–30.
Franklin GA, Casós SR. Current advances in the surgical approach to abdominal trauma. Injury. 2006;37:1143–56.
Fu CY, Wu SC, Chen RJ, Chen YF, Wang YC, Huang HC, Huang JC, Lu CW, Lin WC. Evaluation of need for operative intervention in blunt splenic injury: intraperitoneal contrast extravasation has an increased probability of requiring operative intervention. World J Surg. 2010;34:2745–51.
Williams MD, Young DH, Svhiller WR. Trand toward nonoperative management of splenic injuries. Am J Surg. 1990;160:588–93.
Nakae H, Shimazu T, Miyauchi H, Morozumi J, Ohta S, Yamaguchi Y, Kishikawa M, Ueyama M, Kitano M, Ikeuchi H, Yukioka T, Sugimoto H. Does splenic preservation treatment (embolization, splenorrhaphy, and partial splenectomy) improve immunologic function and long-term prognosis after splenic injury? J Trauma. 2009;67:557–63.
Skattum J, Naess PA, Gaarder C. Non-operative management and immune function after splenic injury. Br J Surg. 2012;99(Suppl 1):59–65.
Scaglione M, de Lutio di Castelguidone E, Scialpi M, Merola S, Diettrich AI, Lombardo P, Romano L, Grassi R. Blunt trauma to the gastrointestinal tract and mesentery: is there a role for helical CT in the decision-making process? Eur J Radiol. 2004;50(1):67–73.
Moore EE, Cogbill TH, Jurkovich GJ, Shackford SR, Malangoni MA, Champion HR. Organ injury scaling: spleen and liver (1994 revision). J Trauma. 1995;38:323–4.
Greenspan L, McLellan BA, Greig H. Abbreviated injury scale and injury severity score: a scoring chart. J Trauma. 1985;25:60–4.
Advanced Trauma Life Support®—ATLS®—Student Manual. 9th ed. American College of Surgeon. ISBN: 978-1880696026.
Haan JM, Bochicchio GV, Kramer N, Scalea TM. Nonoperative management of blunt splenic injury: a 5-year experience. J Trauma. 2005;58(3):492–8.
Pietzman AB, Heil B, Rivera L, et al. Blunt splenic injury in adults: multi-institutional study of the eastern association for the surgery of Trauma. J Trauma. 2000;49(2):177–89.
Bhangu A, Nepogodiev D, Lal N, Bowley DM. Meta-analysis of predictive factors and outcomes for failure of non-operative management of blunt splenic trauma. Injury. 2012;43(9):1337–46. doi:10.1016/j.injury.2011.09.010.
Bouglé A, Harrois A, Duranteau J. Resuscitative strategies in traumatic hemorrhagic shock. Ann Intensive Care. 2013;3(1):1. doi:10.1186/2110-5820-3-1.
Spahn DR, Bouillon B, Cerny V, Coats TJ, Duranteau J, Fernández-Mondéjar E, Filipescu D, Hunt BJ, Komadina R, Nardi G, Neugebauer E, Ozier Y, Riddez L, Schultz A, Vincent JL, Rossaint R. Management of bleeding and coagulopathy following major trauma: an updated European guideline. Crit Care. 2013;17(2):R76. doi:10.1186/cc1268.
Gheju I, Venter MD, Beuran M, Gulie L, Racoveanu I, Carstea P, et al. Grade IV blunt splenic injury—the role of proximal angioembolization. A case report and review of literature. J Med Life. 2013;6(4):369–75.
Olthof DC, van der Vlies CH, Joosse P, van Delden OM, Jurkovich GJ, Goslings JC; PYTHIA Collaboration Group. Consensus strategies for the nonoperative management of patients with blunt splenic injury: a Delphi study. J Trauma Acute Care Surg. 2013;74(6):1567–74. doi:10.1097/TA.0b013e3182921627.
Bhullar IS, Frykberg ER, Tepas JJ 3rd, Siragusa D, Loper T, Kerwin AJ. At first blush: absence of computed tomography contrast extravasation in Grade IV or V adult blunt splenic trauma should not preclude angioembolization. J Trauma Acute Care Surg. 2013;74(1):105–11. doi:10.1097/TA.0b013e3182788cd2.
Dormagen J, Meyerdierks O, Gaarder C, Naess P, Sandvik L, Klow NE. Contrast-enhanced ultrasound of the injured spleen after embolization–comparison with computed tomography. Ultraschall Med. 2011;32(5):485–91. doi:10.1055/s-0029-1246003.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Antonio Brillantino, Francesca Iacobellis, Umberto Robustelli, Elisabetta Villamaina, Franco Maglione, Olga Colletti, Maurizio De Palma, Fiorella Paladino and Giuseppe Noschese declare that they have no conflict of interests regarding the publication of this article.
Research involving human participants and/or animals
The study involves Human Participants and the ethical committee of our Institution approved the study protocol.
Informed consent
All the patients gave informed written consent.
Rights and permissions
About this article
Cite this article
Brillantino, A., Iacobellis, F., Robustelli, U. et al. Non operative management of blunt splenic trauma: a prospective evaluation of a standardized treatment protocol. Eur J Trauma Emerg Surg 42, 593–598 (2016). https://doi.org/10.1007/s00068-015-0575-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-015-0575-z