Abstract
Background
Evaluation of liver fibrosis is important to assess prognosis and guide the treatment for chronic hepatitis B.
Objective
To analyze and compare transient, point, and two-dimensional (2D) shear wave elastography techniques in grading the liver fibrosis.
Methods
Based on the severity of liver inflammation and fibrosis (Scheuer criteria), 158 patients with chronic hepatitis B were assigned into group 1 (either G or S classification < 2) or group 2 (either G or S classification ≥ 2). Group 2 patients commonly require anti-viral treatment. All patients received transient (FibroScan), point (STQ), and 2D (STE) elastography examinations. Receiver operating characteristic curves were calculated from three elastography techniques in individual or in combination.
Results
A total of 158 patients were enrolled into the study, with 39.2% (62) female and mean age of 42.8 (standard deviation 19.1) years old. Transient elastography could not differentiate between group 1 and group 2 patients (P = 0.12), whereas point and 2D elastography examinations could distinguish patients in group 1 from group 2 (P < 0.01 for both STQ and STE). Administration of combined three elastography techniques showed the best diagnostic accuracy (90.1%) for liver fibrosis, which was confirmed with hepatic biopsy examination.
Conclusion
Point and 2D elastography were superior to transient elastography to detect liver fibrosis and guide clinical anti-viral treatment. Analysis of combined transient, point, and 2D elastography techniques showed the better diagnostic accuracy for liver fibrosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chronic hepatitis B is a global health problem with the prevalence close to 4% worldwide [1]. Without appropriate treatments, chronic hepatitis B can develop into hepatic fibrosis and then progress into cirrhosis and even hepatocellular carcinoma [2]. During this development, accurate grading of hepatic fibrosis is important, since early fibrosis may be reversible, whereas cirrhosis is irreversible [3,4,5]. Thus, accurate assessment of hepatic fibrosis grades is very helpful in evaluating the treatment and prognosis [6].
Hepatic biopsy has been the gold standard to assess the severity of liver fibrosis [7]. However, liver biopsy is an invasive procedure with potential complications, including pain, bleeding, infection, organ perforation, and arteriovenous fistula formation. Recently, ultrasound elastography, which measures the propagation velocity of shear waves to estimate the liver stiffness, has been applied to quantitatively assess the severity of liver fibrosis [8]. Ultrasound elastography could be performed with different techniques, including transient, point, and two-dimensional (2D) shear wave elastography [9].
Transient elastography is the first shear wave vibroacoustic technique used in the clinic, but has limitations when applied to patients with obesity or ascites. Point and 2D shear wave elastography could allow the examiner to select a sampling area and obtain real-time images, but are relatively new techniques and require more studies before they could be widely applied in the clinical [9, 10]. Previous studies comparing these different elastography techniques also reported controversial results, some showing better diagnostic values for point and 2D elastography, and others demonstrating no difference between transient and point/2D techniques [11,12,13,14]. In addition, most previous studies focused on patients with advanced liver fibrosis [15, 16]. In fact, detection of mild and moderate fibrosis is more important, since early diagnosis and treatments to patients with early stages of fibrosis might reverse the progression of the disease [3,4,5].
In the current study, we performed transient, point, and 2D elastography examinations in patients with chronic hepatitis B and in different stages of hepatic fibrosis, and compared diagnostic values of three elastography techniques for hepatic fibrosis.
Materials and methods
Study design and participants
Patients with viral B hepatitis, who visited the Ultrasonic Department, Ruijin Hospital (Shanghai, China) between January and July 2017, were prospectively and continuously screened for the study. The study protocol was approved by the hospital ethics committee, and all the study participants signed the informed consent.
The exclusion criteria were: (1) concurrent other liver disorders, such as drug-induced liver injury, autoimmune hepatitis, schistosomiasis, alcohol abuse, or infections from other virus diseases, including cytomegalovirus and human herpes virus; (2) the levels of serum alanine aminotransferase and/or aspartate aminotransferase were 5 times higher than the normal ranges; (3) the heart, brain, and kidney disease or diabetes; (4) conventional ultrasound showed moderate-to-severe fatty liver, which could affect elastography examination.
Study protocol
Study instruments and examiners
Transient elastography was performed with FibroScan device and M or L probe (SuperSonic Imagine, France). Point (STQ) and 2D (STE) elastography were performed with the Mindray Resona 7 ultrasound system and L5-1 probe (Mindray, China).
FibroScan examination was conducted by one sonographer with > 5 years of experience. STQ and STE examinations were conducted by one sonographer with 13 years of experience in sonogram and 500 times of STE examinations. Both sonographers were blinded to the liver biopsy results.
Patient’s position and preparation for examination
Based on the recommendation from European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB) [8], all participants were required to have a 2 h of fasting time before the examination. Patients were placed supine on the examination bed, with right arm elevated above the head to fully expose the right-side intercostal spaces. The left arm was naturally hanged down. The direction of the ultrasound probe was parallel with the intercostal space to avoid the biliary tract and large blood vessels. Appropriate intercostal space was selected to show the best images of the segments 5 and 6 of the right hepatic lobe. Then, markers were placed on the body surface. These markers were used to guide the elastography examination and also for the puncture point during the liver biopsy. Patients were asked to breathe normally (FibroScan) or hold breath for 3–4 s (STQ and STE) to obtain stable images.
Ultrasound elastography examination
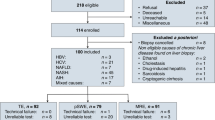
First, routine ultrasound was performed to measure the width of the main portal vein (MPV) and spleen vein (SPV), and the maximal diameter (SP1) and thickness (SP2) of the spleen. When the clear 2D images were obtained, patients were asked to hold the breath. The ultrasound was switched to SWE mode. Images were selected when the uniform color filled more than 90% of the sampling area at a detection depth of 3–7 cm. Then, the images were switched to quality control mode (RLB map added). Successful images were obtained with uniform green PR > 95%. Quantitative detection was performed in a circular area with a diameter of 20 mm in the color box. Satisfactory pictures were framed, measured, and saved (Fig. 1a, b).
STQ examination was performed under the similar condition with ultrasound switched to STQ mode. The size of the sampling frame region of interest (ROI) was 20 × 15 mm. Elastography measurements were performed 5 times with a final standard deviation < 2.0 as the quality control (Fig. 2). FibroScan was performed under the same condition. The average of 10 single-frame measurements was saved while keeping IQR/med < 30%.
Recording was carried out using FibroScan. STE included mean (E1), maximum (E2), and minimum (E3) values. STQ included mean (Q1), maximum (Q2), and minimum (Q3) values. Young’s modulus of elasticity in kilopascals (kPa) was calculated after each measurement.
Liver biopsy
After the ultrasound examination, liver biopsy was performed with a mn 1620 biopsy needle (Magnum biopsy gun, Bard, USA). Satisfactory biopsy was defined as a tissue length > 1.5 cm, containing > 10 integrated hepatic portal area structures. Liver samples were fixed by 10% neutral formalin, embedded in the paraffin for serial sections, and then underwent hematoxylin–eosin and Masson’s trichrome staining. Classifications of liver inflammation and fibrosis stages were determined based on Scheuer criteria [17]. The Scheuer criteria are: G0: no inflammation; G1: mild inflammation; G2: moderate inflammation; G3: moderate-to-severe inflammation; and G4: severe inflammation. Fibrosis grades are: S0: no fibrosis; S1: enlarged fibrotic portal tracts; S2: portal fibrosis with rare septa; S3: fibrosis with architectural distortion, but no obvious cirrhosis; and S4: numerous fibrous septal with pseudolobule formation. Based on the liver biopsy and pathological examination results, patients were assigned into group 1 (either G or S classification < 2) or group 2 (either G or S classification ≥ 2). This G/S classification was used since it was general agreement that patients with either G or S classification ≥ 2 require anti-viral treatment. Two senior pathologists who were blinded to the elastography results reviewed the biopsy specimens and provided the histopathological reports.
Statistical analysis
Data were presented as mean ± standard deviation or median with 95% confidence interval when appropriately. Comparisons of elastography results between group 1 and group 2 patients were performed by student’s t test or Mann–Whitney U test when appropriate. Receiver operating characteristic curve (ROC curve) was constructed, and the area under ROC curve (AUC) was calculated for each elastography examination. Yonden index was used to determine the diagnostic threshold and corresponding diagnostic sensitivity and specificity. The differences among three shear wave elastography techniques were investigated by Delong test with MedCalc software. SPSS (version 20.0, SPSS, USA) was used for statistical analysis. A P < 0.05 was considered statistically significantly different.
Results
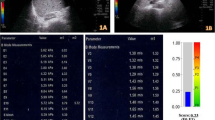
A total of 158 patients were enrolled into the study, with 39.2% (62) female and mean age of 42.8 (standard deviation 19.1) years old. The flowchart diagram of patient enrollment is summarized in Fig. 3. Their baseline characteristics are listed in Table 1.
When comparing the three ultrasound elastography techniques, FibroScan examination did not show any statistically significant difference between group 1 and group 2 (6.1 ± 2.4 vs. 15.0 ± 31.9, respectively, P = 0.12), which had different inflammation and fibrosis in the histopathologic examinations, whereas STQ and STE measurements demonstrated the statistically significant differences between the two groups (group 1 vs. group 2 were: STQ: Q1, 6.7 ± 0.8 vs. 10.1 ± 3.3; Q2, 16.9 ± 6.3 vs. 24.8 ± 10.4; Q3, 3.0 ± 0.9 vs. 4.0 ± 1.9. STE: E1, 6.2 ± 0.8 vs. 9.3 ± 3.0; E2, 12.0 ± 3.5 vs. 17.7 ± 6.8; E3, 3.0 ± 0.7 ± 4.4 ± 1.9. All P < 0.01) (Table 2).
ROC curve analyses with three shear wave elastography techniques are shown in Table 3. Comparisons of the ROC curves by DeLong method showed that STQ and STE showed the significant differences from FibroScan (P < 0.01 and 0.02, respectively); however, there was no statistically significant difference between STQ and STE. Of all of the elastography measurements, the calculated sensitivities were higher than the calculated specificities. The calculated sensitivities for FibroScan, STQ, and STE were 96.6%, 96.6% (Q1), 82.8% (Q2), 69.0% (Q3), 96.6% (E1), 89.7% (E2), and 79.3% (E3), respectively. The calculated specificities for FibroScan, STQ, and STE were 45.1%, 76.8% (Q1), 71.2% (Q2), 64.6% (Q3), 59.8% (E1), 66.4% (E2), and 73.2% (E3), respectively.
Diagnostic performances of combined techniques are shown in Table 4. The sensitivities for each elastography measurement were also higher than the specificities. The combined analysis of three ultrasound elastography techniques demonstrated the best diagnostic accuracy (90.1%).
Discussion
Our results showed that point and 2D elastography could provide better diagnostic performances for liver fibrosis than transient elastography. Analysis of combined three techniques could achieve the highest diagnostic accuracy.
Previous studies demonstrated that ultrasound elastography could provide quantitative information on the severity of liver fibrosis, though the results were controversial [11,12,13,14]. In the current study, transient elastography examination did not show a statistical significant difference between the group 1 and group 2 patients who suffered from different severity in liver fibrosis. Patient’s body habitus, such as obesity, as well as diseases including ascites and emphysema, could affect the examination results from transient elastography [18]. On the contrary, point and 2D elastography examinations showed statistically significant differences between the two group patients. Comparisons of AUCs also revealed that point and 2D elastography examinations were superior to transient elastography in detecting liver fibrosis. This suggested that accurate diagnosis, which could identify the grades of hepatic fibrosis and decide treatment plan, was better with point and 2D elastography than with transient elastography.
The controversial results from previous studies to compare different elastography techniques might be due to the different sonogram equipment used in the studies. In the current study, our transient elastography was conducted with FibroScan which was widely used to diagnose liver fibrosis. The point and 2D elastography examinations were conducted with the Mindray Resona 7 ultrasound system (Mindray, China). This system was never compared with transient elastography before. The point elastography (STQ) examination took multiple measurements of shear wave elasticity imaging in real-time fashion under the guidance of grayscale sonography. The final result was calculated based on the average of multiple measurements, which greatly improves the reliability of the examination. The 2D elastography (STE) examination used a multi-wave imaging platform that applies ultra-high-speed ultrasound wave to track the displacement of shear wave propagation paths at various points in different depths in the tissue. This resulted in a “Mach Cone” phenomenon, which could greatly enhance the production of the shear waves and increase the shear wave propagation efficiency in the tissue, and reduced the focused ultrasound energy to avoid negative biological effects. All of these could result in images with improved resolutions and high accuracy [19]. During the measurements, sampling areas were increased to 2 cm and 2 × 1.5 cm for STE and STQ, respectively. This could reduce the sampling errors and improve the accuracy of quantitative detection of the tissue elasticity. STE and STQ are easy to operate, take less time (3–5 s for one image), and can be applied in patients with ascites and obesity. We tested segments 5 and 6 of the liver since the ultrasound beam was vertical to the intercostal space at this area and could also avoid the large blood vessels and bile duct, less affected by the breathing, and easy for biopsy. Our results showed that point and 2D elastography provide better diagnostic accuracy compared to transient elastography.
There was no previous study which investigated the combined analysis results from the transient, point, and 2D elastography. In the current study, we analyzed the combined test results from these three techniques. Our results showed that combined analysis of multiple techniques could increase the accuracy to evaluate liver fibrosis.
Previous studies to calculate the diagnostic performance of elastography examinations showed that both sensitivity and specificity varied approximately 60–90%, with some studies reporting higher sensitivity than specificity and others reporting opposite results [20,21,22]. In our analysis, the calculated sensitivities and specificities were close to the results from these previous studies. However, in almost all our calculations, all three elastography techniques showed relatively higher sensitivities than specificities, no matter that they were analyzed individually or in combination. Our results suggested that elastography technique might be used to screen patients with possible liver fibrosis, but its finding should be confirmed by other diagnostic test, such as newly developed magnetic resonance elastography [23].
Limitations of the current study included small sample size and single-center study. We used liver biopsy as the diagnostic reference in the current study. However, the area tested by the liver biopsy was smaller than that measured by elastography and may not better represent the whole disease status of the liver. In addition, active inflammation of liver parenchyma might influence ultrasound detection. The diagnostic performance of elastography techniques could be different in patients with different stages of liver fibrosis [11]. Future studies with a large sample size and focused on different stages of liver fibrosis should be performed.
In conclusion, our results showed that point and 2D shear wave elastography had better diagnostic performances than transient elastography in detecting liver fibrosis. Combined analysis of transient, point, and 2D techniques could achieve the improved diagnostic accuracy for liver fibrosis.
References
Schweitzer A, Horn J, Mikolajczyk RT, Krause G, Ott JJ (2015) Estimations of worldwide prevalence of chronic hepatitis B virus infection: a systematic review of data published between 1965 and 2013. Lancet 386:1546–1555
Wright TL (2006) Introduction to chronic hepatitis B infection. Am J Gastroenterol 101(Suppl 1):S1–S6
Calvaruso V, Craxi A (2014) Regression of fibrosis after HBV antiviral therapy. Is cirrhosis reversible? Liver Int 34(Suppl 1):85–90
Friedman SL, Bansal MB (2006) Reversal of hepatic fibrosis—fact or fantasy? Hepatology 43:S82–S88
Pinzani M, Vizzutti F (2008) Fibrosis and cirrhosis reversibility: clinical features and implications. Clin Liver Dis 2:901–913
Sarin SK, Kumar M, Lau GK et al (2016) Asian-Pacific clinical practice guidelines on the management of hepatitis B: a 2015 update. Hepatol Int 10:1–98
Kose S, Ersan G, Tatar B, Adar P, Sengel BE (2015) Evaluation of percutaneous liver biopsy complications in patients with chronic viral hepatitis. Eurasian J Med 47:161–164
Cosgrove D, Piscaglia F, Bamber J et al (2013) EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 2: clinical applications. Ultraschall Med 34:238–253
Sigrist RMS, Liau J, Kaffas AE, Chammas MC, Willmann JK (2017) Ultrasound elastography: review of techniques and clinical applications. Theranostics 7:1303–1329
Barr RG, Ferraioli G, Palmeri ML et al (2016) Elastography assessment of liver fibrosis: society of radiologists in ultrasound consensus conference statement. Ultrasound Q 32:94–107
Gerber L, Kasper D, Fitting D et al (2015) Assessment of liver fibrosis with 2-D shear wave elastography in comparison to transient elastography and acoustic radiation force impulse imaging in patients with chronic liver disease. Ultrasound Med Biol 41:2350–2359
Zeng J, Zheng J, Huang Z et al (2017) Comparison of 2-D shear wave elastography and transient elastography for assessing liver fibrosis in chronic hepatitis B. Ultrasound Med Biol 43:1563–1570
Poynard T, Pham T, Perazzo H et al (2016) Real-time shear wave versus transient elastography for predicting fibrosis: applicability, and impact of inflammation and steatosis. A non-invasive comparison. PLoS ONE 11:e0163276
Ferraioli G, Tinelli C, Lissandrin R et al (2014) Point shear wave elastography method for assessing liver stiffness. World J Gastroenterol 20:4787–4796
Paul SB, Das P, Mahanta M et al (2017) Assessment of liver fibrosis in chronic hepatitis: comparison of shear wave elastography and transient elastography. Abdom Radiol (NY) 42:2864–2873
Zhuang Y, Ding H, Zhang Y, Sun H, Xu C, Wang W (2017) Two-dimensional shear-wave elastography performance in the noninvasive evaluation of liver fibrosis in patients with chronic hepatitis B: comparison with serum fibrosis indexes. Radiology 283:873–882
Scheuer PJ (1991) Classification of chronic viral hepatitis: a need for reassessment. J Hepatol 13:372–374
Sandrin L, Fourquet B, Hasquenoph JM et al (2003) Transient elastography: a new noninvasive method for assessment of hepatic fibrosis. Ultrasound Med Biol 29:1705–1713
Bercoff J, Tanter M, Fink M (2004) Supersonic shear imaging: a new technique for soft tissue elasticity mapping. IEEE Trans Ultrason Ferroelectr Freq Control 51:396–409
Xiao G, Zhu S, Xiao X, Yan L, Yang J, Wu G (2017) Comparison of laboratory tests, ultrasound, or magnetic resonance elastography to detect fibrosis in patients with nonalcoholic fatty liver disease: a meta-analysis. Hepatology 66:1486–1501
Bhat M, Tazari M, Sebastiani G (2017) Performance of transient elastography and serum fibrosis biomarkers for non-invasive evaluation of recurrent fibrosis after liver transplantation: a meta-analysis. PLoS ONE 12:e0185192
Geng XX, Huang RG, Lin JM, Jiang N, Yang XX (2016) Transient elastography in clinical detection of liver cirrhosis: a systematic review and meta-analysis. Saudi J Gastroenterol 22:294–303
Venkatesh SK, Ehman RL (2014) Magnetic resonance elastography of liver. Magn Reson Imaging Clin N Am 22:433–446
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of Ruijin Hospital, Shanghai Jiaotong University School of Medicine.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Ren, X., Xia, S., Ni, Z. et al. Analysis of three ultrasound elastography techniques for grading liver fibrosis in patients with chronic hepatitis B. Radiol med 123, 735–741 (2018). https://doi.org/10.1007/s11547-018-0905-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-018-0905-4