Abstract
The aim of this study was to update the radiation exposure for adult patients undergoing multi-slice CT (MSCT) examinations using size-specific dose estimates (SSDE). Console, displayed CTDIvol and scan parameters were retrospectively recorded for 423 adult patients in seven Sudanese hospitals. Patient torso diameters were measured using digital calipers on the scanner console. SSDE was determined based on transverse images (SSDEtrans) and scout radiographs (SSDEsco). Size-specific conversion factors were used to translate the recorded CTDIvol into SSDE according to the procedure described in the American Association of Physicists in Medicine (AAPM) Report 204. In chest CT, mean CTDIvol, SSDEtrans and SSDEsco ranged: from 4.3 to 47.5 mGy (average: 12.8), 5.5 to 70.3 mGy (average: 18.6) and 5.8 to 63.5 mGy (average: 18.7), respectively. In abdominal CT, mean CTDIvol, SSDEtrans and SSDEsco ranged: from 4.0 to 74.5 mGy (average: 16), 5.5 to 152.8 mGy (average: 23.9) and 6.0 to 151.3 mGy (average: 25.21), respectively. Our study highlights the relationships between CT dose and patient dimensions measured from scout and transverse CT images. The correlations between the patient size and dose based on scout images were less significant than that based on transverse images. High dose levels and dose variations among hospitals reveal the need for standardization of scanning protocols and staff training on adoption of scanners’ dose reduction techniques.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
According to UNSCEAR Global Survey of Medical Radiation Usage and Exposures, CT scanning accounts for 43% of the total collective effective dose due to diagnostic medical radiology [1]. CT scanning accounts for 7.9% of the total number of diagnostic medical examinations in health-care level I countries, just over 2.0% in health-care level II countries and just under 14% in health-care level III/IV countries [1]. The development of multi-slice CT (MSCT) has led to a noticeable improvement in clinical CT performance, enabling faster and accurate diagnosis of diseases. Its contribution to radiation dose for the general population has become significantly higher. For this reason, low-dose CT has become the subject of numerous research publications. Epidemiological studies have failed to answer the various questions regarding cancer risk related to low radiation levels; nonetheless, the data were robust and the topic is challenging [2]. Nevertheless, the associated high radiation dose and the associated risk of carcinogenicity are of concern. Accurate dose estimates are, therefore, essential for better protection of the patient receiving CT examination as well as other medical procedures utilizing ionizing radiation.
In the European Guidelines for CT, two quantities are proposed for setting diagnostic reference levels: CT dose index (CTDIvol) per slice (serial scanning) or per rotation (helical scanning) and the dose length product (DLP) per complete examination [3]. The CTDIvol estimates the average dose within a scan volume from dose measurements made in a standard 16-cm (head) or 32-cm (body) CT phantom. DLP accounts for the total radiation dose delivered to the scanned region of the body, defined as the product of CTDIvol and the scan length [3, 4].
The recommendations by the International Electrotechnical Commission (IEC) in 2002 made it mandatory for all manufacturers to display both CTDIvol and DLP on the screens of their CT devices [4]. However, because patients vary in size and shape, CTDIvol is an insufficient patient dose metric [5, 6]. In fact, CTDIvol is size independent, and patients with different sizes have the same CTDIvol value if scanned using the same imaging parameters. Moreover, using CTDIvol, the dose to patients smaller than the acrylic CT body phantoms (32 cm) is underestimated by as much as a factor of three [7,8,9].
Concerns over using CTDIvol as a dose metric has led the American Association of Physicist in Medicine to develop and recommend size-dependent conversion factors, which can be used to determine size-specific dose estimate (SSDE) values from CTDIvol values [10]. The SSDE corrects for the difference between the patient size and the acrylic CT phantom and offers an improved metric for expressing the average absorbed dose.
At the national level, CT patient dose data are available in Sudan in terms of CTDIvol and DLP dose indices [11, 12]. Thus, it was the aim of this study to update the radiation exposure for adult patients undergoing multi-detector CT examinations at Sudanese hospitals using size-specific dose estimates (SSDE). It was also the aim of this study to investigate the effect of body dimensions on SSDE calculated from transverse and scout images.
Materials and method
Study design
A total of 423 adult patients who underwent chest and abdominal CT examinations in seven MSCT CT facilities. The hospitals were in Khartoum and Medani states, representing the largest states in terms of population density and provide diagnostic services for a wide area around them. These hospitals were selected because these are among the largest in terms of workload. Patients were selected consecutively, and the relevant dose information was retrieved from the archive of examinations performed between May 2015 and December 2016. In each hospital, data on a minimum number of ten patients per examination, considered as a statistically significant number in radiological dose surveys, were collected. Survey data were collected from the following hospitals: Advance Diagnostic Center (ADC); Al-Amal Hospital (AMH); Antalia private Clinic (APC); Medani Hospital (MH); Ribat University Hospital (RUH); National Armed Force Hospital (AFH); Royal Care Hospital (RCH). Our institution ethics approved the study. Due to the retrospective nature of the study, formal consents from the examined individuals were waived.
Dose determination
Dose information and scan parameters pertaining to the studied patients were retrospectively collected from the DICOM header, including patient information (age, gender), tube voltage, tube current, rotation time(s), pitch value and CTDIvol.
For SSDE calculations, we measured the diameter of the patient’s images using digital calipers on the scanner console. Measurements were done for anterior–posterior diameter (hereafter, DAP) and lateral diameter (hereafter, DLAT) from the mid-slice location on the transverse CT image and DLAT on scout images. Measured dimensions, \(D_{{{\text{AP}} + {\text{LAT}}}}\) and DLAT were used as patient’s size indicators [10]. Next, the SSDE was calculated by multiplying the console-displayed CTDIvol with the size-specific conversion factors (f) given in the AAPM report 204 [10]:
Descriptive statistics was used to analyze the study results. Pearson test was used to evaluate the correlations between CTDIvol, SSDE and patient diameter in chest and abdominal CT. The correlation was considered statistically significant at P value less than 0.05.
Quality control measurements
The parameters, which best characterize the image quality, were assessed by CATPHAN 504 CT quality assurance phantom (The Phantom Laboratory Ltd, NY, USA). Parameters tested included slice width, linearity, uniformity, high and low contrast resolution and noise. The results were compared with recommended tolerance levels given in International Electrotechnical Commission [4].
Results
From 423 adult patients who underwent MSCT CT examinations, there were 84 females (mean age = 51 ± 17, range 19–90, 3rd quartile 65) and 105 males (mean age = 54 ± 16, range 22–82, 3rd quartile 66) in chest examinations, and 98 females (mean age = 51 ± 16, range 17–85, 3rd quartile 65) and 93 males (mean age = 52 ± 17, range 18–85, 3rd quartile 70) in abdominal examinations.
Table 1 summarizes the characteristic performance parameters for the CT systems included in the study. Four scanners were from Toshiba (three 64-slice and one 16 scanners), two scanners from Neusoft (128-slice and 16-slice) and one scanner from General Electric (8-slice). Image quality tests of the CT systems are shown in Table 2.
Modern multi-slice CT scanners are equipped with tube current modulation features where the radiation dose is adjusted according to patient attenuation. The survey showed that some centers use the protocols provided by the vendors and others use manual settings for the examinations, which could explain the variation in mAs values recorded in the study (Table 3). Also, it appeared that radiographers lacked training on how to deal with dose reduction techniques of the scanners.
As detailed above, SSDE was estimated via two ways: (1) from transverse images (hereafter, SSDEtrans) using \(D_{{{\text{AP}} + {\text{LAT}}}}\) as patient size; (2) from scout images (hereafter, SSDEsco) using DLAT as patient size. The relations between CTDIvol, SSDEtrans, SSDEsco and body size were studied for multi-slice CT examinations of 423 adult patients.
Tables 3 and 4 present patient information (age and size), scan parameters (kV, mAs), CTDIvol, SSDEtrans and SSDEsco for chest and abdominal CT.
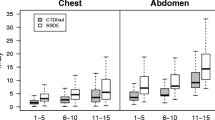
In chest CT scanning, mean CTDIvol, SSDEtrans and SSDEsco ranged: from 4.3 to 47.5 mGy (average: 12.8), 5.5 to 70.3 mGy (average: 18.6) and 5.8 to 63.5 mGy (average: 18.7), respectively. The relationships between patient size and CT doses, CTDIvol, SSDEtrans and SSDEsco, are shown in Fig. 1a, b.
Based on transverse images (Fig. 1a), weak correlations were shown between patient size and CTDIvol (r2 = 0.003) and between patient size and SSDEtrans (r2 = 0.023). Similarly, when patient dimensions were taken from scout radiographs (Fig. 1b), the correlations between patient size and CTDIvol (r2 = 0.14) and between patient size and SSDEscout (r2 = 0.009) were weak. These correlations were statistically significant at P = 0.05.
Concerning abdominal CT, mean CTDIvol, SSDEtrans and SSDEsco ranged from 4.0 to 74.5 mGy (average: 16), 5.5 to 152.8 mGy (average: 23.9) and 6.0 to 151.3 mGy (average: 25.21), respectively. The relationships between patient size and CT doses, CTDIvol, SSDEtrans and SSDEsco, are shown in Fig. 2a, b.
Based on transverse images (Fig. 2a), strong correlation was shown between patient size and CTDIvol (r2 = 0.39) and between patient size and SSDEtrans (r2 = 0.39). Both correlations were statistically significant at P = 0.05. On the contrary, when patient dimensions were taken from scout radiographs (Fig. 2b), weak correlation was shown between patient size and CTDIvol (r2 = 0.05) and between the patient size and SSDEscout (r2 = 0.01). The later correlation was statistically insignificant at P = 0.05.
In Table 5, a statistical summary is given for the studied CT doses [mean, σ, range (min–max), third quartile] and max/min ratios.
Significant dose variations were presented, reflected by the maximum to minimum ratio of 11.04 (chest CT) and 18.62 (abdominal CT), which is a clear indication that scan protocols were not standardized.
Discussion
CTDIvol provides a useful way to compare radiation output levels among different scanners. CTDIvol depends on scan parameters (kV and mAs), but does not consider the physical characteristics of the patient. This is of concern because the dose received depends on both the patient size and the scanner radiation output [5,6,7,8,9,10, 13]. SSDE is determined from CTDIvol using conversion coefficients that depend on patient effective diameter, which correlates linearly with patient weight. Both patient body characteristics and the radiation output are better described by the SSDE.
Performance of MSCT
Image quality assurance tests were performed, and the results were compared with the tolerance limits specified by the International Electrotechnical Commission [4]. With the exception of the low contrast resolution at 1%, the QA parameters tested fell within the recommended tolerance level indicating satisfactory performance. The equipment was not covered under regular QA program and thus baseline data for the tested QA parameters do not exist.
Concerning dose performance, CTDIvol can be used as a suitable dose descriptor for CT scanner output. For instance in abdominal CT, a 16-slice CT scanner at the ADC hospital provides the highest CTDIvol (23.3 mGy), followed by 64-slice CT at AMH (21.0 mGy) and AFH (22.2 mGy), followed by 128-slice CT at RUH (9.6 mGy). The low dose at 16-slice CT at APC is apparently due to the lower kV used. With the exception of 16-slice CT at RCH, one would conclude that multi-slice CT scanners tend to provide lower patient dose compared to the same type of CT with lower multi-detectors in a row. This is mainly due to the faster rotation which allow scanning larger volumes with less radiation dose. Definite conclusions on performance of different types of MSCT could not be feasible in this study due to the limited number of scanners per model studied.
CTDIvol vs SSDE
As seen (Figs. 1, 2), SSDE values from transverse CT images and scout radiographs were significantly different compared to CTDIvol. The correlation between the patient size and dose based on transverse images was stronger than that from scout radiographs. This agrees with the results of the study by Pourjabbar et al. [14], who reported that when patient dimensions were measured from scout radiographs, the obtained SSDE values overestimate the patient dose [14]. SSDE values (Figs. 1, 2) were always higher than CTDIvol, and larger size patients—more than 32 cm—received lower doses than smaller size patients, which was consistent with the nature of the conversion factors provided by the AAPM repot 204 [10].
In most clinics, scanners used a fixed exposure setting instead of tube current modulation. This has the implication that small patients would receive unnecessarily high absorbed doses and risks, while in large patients there would be poor image quality. Many studies have examined the relation between CTDIvol and patient diameter keeping radiographic techniques (mAs) constant. They agreed that for a given CT technique, patient dose decreases as patient size increases because there is more attenuation of the incident X-ray beam by surrounding soft tissues, necessitating adjustment according to patient size for appropriate CT dosimetry [15, 16]. AEC systems automatically adjust tube current to account for global variations in patient sizes and local thickness variations in individual patients [15]. In this regard, several authors studied the relationship between the radiation absorbed dose and patient size [17,18,19,20]. The result was an increase in patient organ dose as a function of patient size, which was ascribed to the AEC system that attempts to maintain constant image noise for all patient sizes [17, 19,20,21].
On the other hand, the relation between the patient size and dose in chest CT scanning showed a different trend. As seen (Fig. 1a), larger patients received higher (in case of SSDE) and lower (in case of CTDIvol) doses than smaller ones. The correlation between CTDIvol, SSDEsco and DLAT was insignificant at P = 0.05. In a study by Anam et al. [22], it was shown that among other factors, patient table can have significant effect on SSDE [22]. In chest CT scanning and generally when scanning tissues having different density from water or PMMA, SSDE considerably underestimates the absorbed dose due to the much lower density of lung tissues in chest [23].
To overcome this problem, the water equivalent diameter (DW) has been proposed that considers both the geometrical size of the patient and the inhomogeneity of the patient’s tissues [24]. Thus, further studies are needed to further improve current patient dose data using DW.
Comparison with the literature and dose optimizations
To optimize the radiation dose delivered to patients during radiological procedures, estimated radiation doses should be compared against established diagnostic reference levels (DRLs) [25, 26]. Examples of DRLs for abdominal CT are those recommended by the American College of Radiology in the USA (25.0 mGy), the Health Protection Agency in the UK (14.0 mGy) [25, 26] and the Italian nationwide survey (18 mGy) [27]. When our results (22.8 mGy) were compared with these DRLs, the current doses were comparable to the US DRLs.
As seen (Table 4), inter-hospital dose ratios—maximum to minimum—are as high as 11.04 (chest CT) and 18.62 (abdominal CT). All hospitals used almost 120 kV in exception to one APC hospital in chest CT, which reported using both 110 and 120 kV (median 115) during chest CT. There is wide variation in the mAs and therefore variations in the CTDIvol values, which are determined by the scan protocol of the specific CT scanner. Dose variations among hospitals are clear evidence that dose reduction is possible without losing the quality of diagnostic information. The most direct optimization measures are the standardization of CT protocols, either via using tube current modulation (TCM) or special dose-saving protocols provided by most of the modern MSCT CT scanners. TCM adjusts the mAs deployed according to the patient’s body size and hence the dose. When TCM is used, larger patients receive higher doses that maintain the same image quality. Furthermore, CTDIvol also depends on the helical pitch that considers the consecutive scanning in helical CT. CTDIvol is inversely correlated with the pitch. Therefore, it is always advised to use high pitch values for lower patient dose. CTDIvol values vary due to the variation of the normalized output (nCTDIw) among scanners. The latter depends on the inherent characteristics of the scanner such as bowtie filters used. Survey results revealed an important room for dose optimization; however, lack of proper training and inexperienced technologists are major obstacles to the full utilization of these features.
Conclusions
To provide more accurate estimations of patient doses, the SSDE metric was used in this study instead of CTDIvol. This study highlights the relationships among scanner radiation output and SSDE measurement of patient dimensions from both scout radiographs and transverse CT images. The correlation between the patient size and dose based on scout images was less significant than that based on transverse images. The results will assist the medical physics community and the radiologist to choose proper indicators for patient size when determining SSDE. The study also highlights the need for dose optimization through CT protocol standardizations and staff training on adoption of scanners’ dose reduction techniques. For more accurate patient dose estimates, further studies are certainly needed to improve the patient dose data in CT using water equivalent diameter.
References
United Nations Scientific Committee on the Effects of Atomic Radiation (2010) UNSCEAR 2008. Sources and effects of ionizing radiation
Colagrande S, Origgi D et al (2014) CT exposure in adult and paediatric patients: a review of the mechanisms of damage, relative dose and consequent possible risks. Radiol Med 119:803–810. https://doi.org/10.1007/s11547-014-0393-0
Menzel H, Schibilla H, Teunen D (2000) European guidelines on quality criteria for computed tomography. European Commission, Luxembourg, p 16262
International Electrotechnical Commission (2002) Medical electrical equipment—part 2-44: particular requirements for the basic safety and essential performance of X-ray equipment for computed tomography. IE-60601, Geneva, 2002
McCollough CH, Leng S, Yu L et al (2011) CT dose index and patient dose: they are not the same thing. Radiology 259:311–316
Dixon RL (2003) A new look at CT dose measurement: beyond CTDI. Med Phys 30:1272–1280
Boone J, Strauss K, Cody D et al (2011) AAPM report No. 204: size-specific dose estimates (SSDE) in pediatric and adult body CT examinations. American Association of Physicists in Medicine, College Park
Strauss K (2014) Dose indices: everybody wants a number. Pediatr Radiol 44:450–459
McCollough C, Cody D, Edyvean S et al (2008) AAPM report 96: the measurement, reporting, and management of radiation dose in CT Report of AAPM Task Group 23. American Association of Physicists in Medicine, College Park (ISSN: 0271-7344). ISBN 978-1-888340-73-0
American Association of Physicists in Medicine (2011) Size-specific dose estimates (SSDE) in pediatric and adult body CT examinations (Task Group 204). American Association of Physicists in Medicine, College Park, p 14
Suliman II, Abdalla SE, Ahmed NA, Galal MA, Salih I (2011) Survey of computed tomography technique and radiation dose in Sudanese hospitals. Eur J Radiol 80(3):e544–e551
Suliman II, Khamis HM, Ombada TH, Alzimami K, Alkhorayef M, Sulieman A (2014) Radiation exposure during paediatric CT in Sudan: CT dose, organ and effective doses. Radiat Prot Dosim 167(4):513–518
Mayo-Smith WW, Hara AK, Mahesh M, Sahani DV, Pavlicek W (2014) How I do it: managing radiation dose in CT. Radiology 273(3):657–672
Pourjabbar S et al (2014) Size-specific dose estimates: localizer or transverse abdominal computed tomography images? World J Radiol 6(5):210–217 (ISSN 1949-8470)
Huda W, Vance A (2007) Patient radiation doses from adult and pediatric CT. Am J Roentgenol 188(2):540–546
Favazza CP, Yu L, Leng S, Kofler JM, McCollough CH (2015) Automatic exposure control systems designed to maintain constant image noise: effects on computed tomography dose and noise relative to clinically accepted technique charts. J Comput Assist Tomogr 39(3):437
McCollough CH, Bruesewitz MR, Kofler JM Jr (2006) CT dose reduction and dose management tools: overview of available options. Radiographics 26(2):503–512
Schindera ST, Nelson RC, Toth TL, Nguyen GT, Toncheva GI, DeLong DM, Yoshizumi TT (2008) Effect of patient size on radiation dose for abdominal MDCT with automatic tube current modulation: phantom study. Am J Roentgenol 190(2):W100–W105
Christner JA, Braun NN, Jacobsen MC, Carter RE, Kofler JM, McCollough CH (2012) Size-specific dose estimates for adult patients at CT of the torso. Radiology 265(3):841–847
Kalra MK, Rizzo SM, Novelline RA (2005) Reducing radiation dose in emergency computed tomography with automatic exposure control techniques. Emerg Radiol 11(5):267–274
Rizzo S, Kalra M, Schmidt B, Dalal T, Suess C, Flohr T, Saini S (2006) Comparison of angular and combined automatic tube current modulation techniques with constant tube current CT of the abdomen and pelvis. Am J Roentgenol 186(3):673–679
Anam C, Haryanto F, Widita R, Arif I, Dougherty G, McLean D (2017) The impact of patient table on size-specific dose estimate (SSDE). Australas Phys Eng Sci Med 40(1):153–158
Li B, Behrman RH (2012) Comment on the “Report of AAPM TG 204: size-specific dose estimates (SSDE) in pediatric and adult body CT examinations” [Report of AAPM TG 204, 2011]. Med Phys 39(7):4613–4614
McCollough C, Bakalyar DM, Bostani M, Brady S, Boedeker K, Boone JM, McNitt-Gray MF (2014) Use of water equivalent diameter for calculating patient size and size-specific dose estimates (SSDE) in CT: the Report of AAPM Task Group 220. AAPM Rep 2014:6
American College of Radiology (2008) ACR practice guideline for diagnostic reference levels in medical X-ray imaging. In: American College of Radiology (ed) Practice guidelines and technical standards. American College of Radiology, Reston, pp 799–804
Shrimpton PC, Hillier MC, Meeson S, Golding SJ (2014) Doses from computed tomography (CT) examinations in the UK—2011 review. ISBN 978-0-85951-759-1
Palorini F, Salerno S et al (2013) Adult exposures from MDCT including multiphase studies: first Italian nationwide survey. Eur Radiol. https://doi.org/10.1007/s00330-013-3031-7 (ISSN 0938–7994)
Acknowledgements
The authors would like to thank the hospitals and their staff for their cooperation during data collections.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have no conflicts of interest to disclose.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Bashier, E.H., Suliman, I.I. Multi-slice CT examinations of adult patients at Sudanese hospitals: radiation exposure based on size-specific dose estimates (SSDE). Radiol med 123, 424–431 (2018). https://doi.org/10.1007/s11547-018-0859-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-018-0859-6