Abstract
At present, concern regarding radiation exposure is increasing with the prevalence of radiologic examination. As radiation damages the human body, we have evaluated medical radiation dose values and studied the importance of optimizing radiation exposure. We measured entrance surface dose (ESD) values using a RANDO® phantom (neck) in 94 randomly selected locations in the central region of Korea. Thyroid and organ doses were calculated using Monte Carlo simulations (PCXMC 2.0.1) based on measured values. In addition, the lifetime attributable risk (LAR) of cancer was calculated for the thyroid, using the method proposed in the biological effects of ionizing radiation VII report. The average measured ESD values obtained using the RANDO® phantom (neck) were antero-posterior 1.33 mGy and lateral 1.23 mGy, for a total of 2.56 mGy. Based on the ESD values measured using the phantom, the organ doses were obtained using a Monte Carlo simulation (PCXMC 2.0.1). The thyroid dose was 1.48 mSv on average. In evaluating the LAR of thyroid cancer incidence, a frequency of 0.02 per 100,000 from 2.94 per 100,000 males and a frequency of 0.10 per 100,000 from 16.23 per 100,000 females were found. The risk of cancer was found to be higher when the patient’s age was lower, and was also higher in females than in males. It was concluded that beneficial exams in the medical field should not be prohibited because of a statistically small risk, although acknowledgement of the dangers of ionizing radiation is necessary.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diagnostic radiology is the largest source of radiation exposure among the various fields in which man-made artificial radiation is used. However, diagnostic radiology is a fundamental stage in the diagnosis and evaluation of modern diseases and is the basic engine, along with antibiotics, that is leading modern medical science. According to the Korean Ministry of Food and Drug Safety, the annual amount of diagnostic radiation exposure per person increased from 0.93 mSv in 2007 to 1.4 mSv in 2011, a rate of 51 % for 5 years. The numbers of radiation exams were also shown to have increased from 3.3 per person in 2007 to 4.6 in 2011 [1]. However, it is extremely rare for medical radiation exposure to be a cause for cancer, because the medical tests involve low-dose radiations that have a radiation dosage of less than 100 mSv, which is nearly equal to that of natural background radiation [2, 3].
The neck (cervical spine) simple X-ray is the most commonly used trauma and disease diagnostic method. For this method, CT and MRI are used optionally in order to check the neck for abnormality (e.g., soft tissue inflammation, infection, or tumors of the laryngopharynx), although they are basic test methods. The incidence in the risk of thyroid cancer in children and the youth exposed to radiation because of radiography tends to be 88 percent higher per 1 Gy [4]. According to Seaberg, thyroid cancer caused by radiation exposure is likely to be more malignant compared to that of patients who have not been exposed to radiation, and the radiation exposure itself is the cause of the tumor, whether benign or malignant [5]. In addition, Memon stated that dentistry radiation exposure levels are deeply related to incidents of thyroid cancer and that the effects of radiologic examinations should therefore be considered in the young (children and adolescents) and in women [6].
The National Academies’ Biological Effects of Ionizing Radiation 7th Report (BEIR VII Phase 2) developed risk estimates for cancer due to exposure to low-level ionizing radiation using the most current data and epidemiologic models available, incorporating data from atomic bomb survivor studies as well as medical and occupational radiation studies. Its review of available data supports the so-called linear no-threshold risk (LNT) model for low-dose exposure to low-linear energy transfer radiation such as X-rays, in which the risk of cancer proceeds in a linear fashion with no lower threshold [3].
Radiation exposure contains sufficient energy to change the structure of human cells, including that of deoxyribonucleic acid (DNA). Some elements of such atomic changes are so intricate that the repair mechanisms in the human body may not be able to fully recover. Even for small changes to minor components, cancer genes may be produced or damage to cancer suppressor genes may be caused, which will negatively influence health. According to such mechanisms, radiation is a Grade I carcinogen, and it is classified as a carcinogen by the International Cancer Society [7].
Taking these recent research results into account, it is apparent that damage can occur as a result of medical radiation exposure. Furthermore, no attention is currently being paid to the level of patient cumulative radiation, and no actual method exists for measuring or assuming cumulative radiation amounts. Chronic side effects of radiation, however, continue to occur even at low doses, and it is clear that radiation negatively influences the human body, which includes increased incidences of cancer.
Therefore, this study has three aims: evaluation of radiation exposure doses using a phantom (neck; cervical spine), measurement of entrance surface doses (ESD), and calculating the thyroid and neighboring organs doses using Monte Carlo simulations. We also calculate the lifetime attributable risk (LAR) of cancer of the thyroid due to radiation exposure, using methods proposed by BEIR VII, and study the importance of optimizing radiation exposure.
Materials and methods
Research sample and entrance surface dose (ESD)
The authors randomly selected 94 sites in which radiography is used (film screen type, storage phosphor, flat panel type) in general hospitals (over 100 inpatients), hospitals (between 30 and 100 inpatients), and medical centers (primarily outpatient) [8], based on Act 3 of the Korean medical law, in the Korean central district (Gangwon-do, Chungcheongnam-do, Chungcheongbuk-do, and Daejeon metropolitan city).
A 12-mm glass dosemeter with a tin filter (Dose Ace M-GD352M; dose range: 0.01 mGy–10 Gy), a dose reader system (FGD-1000), a pre-heating system (MDKN 302), and an annealing oven system (M-NEW1CT) (all: Asahi Techno Glass, Ltd., Japan) were used to measure the dose ranges for different procedures [9–11]. We calibrated the dose reader system according to manufacturers’ protocols, and the doses were reproducible within a range of 2 % using a standard dose of 6 mGy.
We secured a RANDO® phantom (height, 175 cm; weight, 73.5 kg; adult male phantom; Alderson Laboratory, USA) to the X-ray table, positioning the dosemeter at the approximate beam center for each of the cervical antero-posterior (AP) and lateral (Lat.) examinations (Fig. 1). An auto exposure control, set according to the guidelines established by the Korean Ministry of Food and Drug Administration (KFDA) [12] and the National Radiological Protection Board (NRPB) [13], was employed.
Calculation of organ doses
PCXMC is a PC-based Monte Carlo program used to calculate patient dose in medical X-ray examinations (radiography and fluoroscopy) and developed by STUK (the Finnish Radiation and Nuclear Safety Authority). Using PCXMC 2.0.1 (STUK CO., Helsinki, Finland), a Monte Carlo simulation program, organ doses, and effective doses were calculated. PCXMC calculates the organ and effective doses from interactions due to the Compton effect in the human body, based on mathematical probability. This software uses the phantom model developed by Cristy and Eckerman [14], and the phantom, projection angle (AP, both Lat., PA: postero-anterior), X-ray tube (tube voltage (kVp), added filter thickness, and anode angle), height, weight, the parameters used in the examination, and other details for use in the calculation can be edited and selected.
The effective doses show the risk for organs and tissue when the full body is under radiation exposure. Further, the effective doses are expressed by the total sum of the values calculated based on the tissue-weighting factor and equivalent dose in the tissue. The tissue-weighting factors are set by the International Commission on Radiological Protection (ICRP) 60 and 103, as given in [15, 16]. The Monte Carlo simulation in this study was based on the phantom, which has patient-representative height and weight, kVp, focus–image distance (FID), and projection angle. In terms of exposure area, the focus–skin distance (FSD) and beam field size were calculated using FID (AP: 110 cm, Lat.: 180 cm) values and image field size (25 × 30 cm), using the PCXMC software.
In this study, each of the investigated X-ray tube voltages, an anode, and a total inherent filtration (tube and collimation) system were used. By inserting the ESD value data, the organ doses of the esophagus, oral mucosa, salivary glands, upper spine, clavicles, and thyroid were obtained.
BEIR VII risk modeling
For each examined age, sex, and organ, the LAR of cancer incidence from a theoretical 100-mSv organ equivalent dose was determined using Table 1 2D-1 of the BEIR VII report [3]. This LAR was scaled linearly based on the actual organ dose determined by the Monte Carlo simulation. For example, a 40-year-old woman receives a dose of 0.001 Gy (1 mGy) to the breast from a mammogram. The table shows the estimated lifetime risk of being diagnosed with breast cancer for a female exposed to 0.1 Gy at the age 40 as 1.41 per 100,000 (approximately 1 in 70,000). The estimate for a male exposed to 0.001 Gy is obtained as (0.001/0.1) × 141 = 1.41 per 100,000. The risks for the thyroid and all solids, considering all cancers, all solid cancers, and leukemia incident risks, were evaluated in this LAR of cancer incidence calculation process.
Result
Dose-area product value and organ doses
Based on the test results using the RANDO® phantom at the 94 randomly selected locations, the average measured ESD values were AP 1.33 ± 0.91 mGy and Lat. 1.23 ± 0.82 mGy, with a total value of 2.56 ± 1.50 mGy (Table 1). Based on the ESD value measured from the phantom, the organ doses were obtained using Monte Carlo simulations (PCXMC 2.0.1). Each organ dose exhibited the following average values: oral mucosa, 0.72 mSv; salivary glands, 0.77 mSv; upper spine, 1.19 mSv; clavicles, 1.76 mSv; and thyroid, 1.48 mSv (Table 2).
Evaluation of LAR of cancer
According to the method proposed in the BEIR-VII report, the evaluation of the LAR of cancer is the result of the calculated risk for a population of 1,000,000 of developing all cancers, all solid cancers, leukemia, and thyroid cancer. The LAR of cancer incidence due to neck examination for 0–50 years is listed in Table 3. The results of this research indicate that, for a 0-year-old, the following LARs are likely: all cancer incidence, 65.61 per 100,000 males and 122.29 per 100,000 females; all solid cancer incidence, 59.54 per 100,000 males and 117.55 per 100,000 females; leukemia cancer incidence, 6.06 per 100,000 males and 4.73 per 100,000 females; and thyroid cancer incidence, 2.94 per 100,000 males and 16.23 per 100,000 females (Table 3).
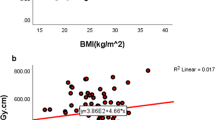
As regards radiation exposure, the LAR showed that, females have an approximately two times higher risk for all cancers compared to males, when the age of the exposed group is lower, along with an approximately 5.5 times higher risk of thyroid cancer. These trends can be seen in the graphs of cancer incidence for different age groups shown in Figs. 2 and 3.
Discussion
As the use of radiation medical equipment increases, interest in reducing the risk of cancer grows simultaneously. The American Cancer Society recently identified environmental carcinogens and radiation exposure as cancer risk factors as a result of the increased use of X-rays and computed tomography (CT) [17]. In addition, the medical use of SunLamp, which is used for cosmetic reasons and to cure acne or other skin diseases, was included as a dangerous factor [18]. In our research, the ESD value under cervical spine X-ray radiography was found to be 2.56 mGy. Using PCXMC 2.0.1 and the measured ESD value to conduct a Monte Carlo simulation, the thyroid radiation dose was found to be 1.48 mSv.
In a report on the influence of diagnostic X-rays, conducted in 15 countries including England, Berrington de Gonzalez and D›arby stated that approximately 0.6 % of diagnosed cancer, especially with regard to the evaluation of accumulated cancer risk of ages up to 75 in England, was related to radiation exposure. Of the other countries, 13 showed rates of 0.6–1.8 %, while Japan had the highest rate of 3 %. This is said to be related to the frequency of radiology exams in each country [19].
According to the Ministry of Food and Drug Safety in the Republic of Korea, the number of annual diagnostic radiography examinations was 160,000,000 in 2007, which increased to 220,000,000 in 2011, a rate of increase of approximately 35 % over 5 years [1]. Because radiation exposure doses accumulate, not only should the risk for the exposed patient should be considered, but also the genetic effects this exposure might have on his or her offspring should be taken into consideration. However, focus on health increases with increases in people’s average income and, accordingly, the number of regular health checkups grows. In addition, life expectancy is extended and, in recent medical trends, more scientific diagnostic methods such as radiography are applied, rather than diagnoses based on experience. Such phenomena lead to an increase in the amount of radiation exposure because of multiple health examinations, which puts individuals’ health in danger with threats such as cancer.
The reason for selecting BEIR VII lifetime model is that organ dose of thyroid is 1.48 mSv. This value is lower than the threshold dose 100 mSv giving deterministic effect in Thyroid LAR of cancer evaluation. This model applied the linear no-threshold (LNT) model, stating that even for very small doses, a minor increase in the risk of cancer can potentially cause a patient to develop cancer. The BEIR VII risk models were developed based on a comprehensive review of the world literature on radiation epidemiology. It is impossible to reconcile every study in this complex literature with every other study, and there are differing interpretations of these data; therefore, despite the extensive efforts made to compose a highly expert committee, avoid conflicts of interest, and obtain diverse perspectives, some of the premises underlying the BEIR VII risk models are not uniformly agreed upon, and its applicability to different populations has been challenged. Uncertainties in the BEIR VII models relate to the methods used to transport data from Japanese atomic bomb survivors to a US population with different baseline cancer rates, sampling variability in parameter estimates in the risk models, the choice of dose and dose-rate effectiveness factors (DDREF), and the manner in which differences in relative biological effectiveness between X-rays and other types of ionizing radiation are accounted for [3].
Other radiation protection organizations, such as the ICRP [15], have selected a higher DDREF than that used in BEIR VII, typically 2.0 rather than 1.5. Using a higher DDREF results in lower risks of cancer incidence than those reported in this study. On the other hand, current radiation protection guidelines assign a radiation weighting factor of 1 to X-rays, although some biological evidence suggests that the biological effectiveness per unit-absorbed dose of X-rays may be twice that of high-energy photons [3]. This may result in an underestimation of the cancer risk associated with radiation exposure from simple neck (cervical spine) X-rays using our methodology. Perhaps the most debated assumption of the BEIR VII models is the LNT relationship between dose and cancer risk. Besides the BEIR VII committee, the National Council on Radiation Protection and Measurements (NCRP) [20], ICRP [21], United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR) [22], and NRPB [23] have recently reviewed the LNT hypothesis. While there are subtleties in the positions of each of these organizations, the majority basically conclude that LNT best fits the data and should remain the standard for radiation protection.
However, in our research, the organ doses produced using the Monte Carlo simulation program to evaluate the risk of cancer and LAR of cancer incidence have sufficient credibility. According to the results of this research, regarding a 0-year-old, the LARs of thyroid cancer incidence are likely to be 2.94 per 100,000 males and 16.23 per 100,000 females (Table 3). The LARs of cancer incidence due to radiation exposure are likely to be approximately two times greater for all cancers and about 5.5 times greater for thyroid cancer, when the exposed patient’s age is lower than average, while female patients, compared to males, are more likely to develop cancer. This can be seen in the cancer incident graph of the various age groups (Figs. 2, 3).
Transitions in chromosomes is a type of genetic information damage that causes various types of cancer, because of the body’s inability to properly recover damaged DNA. If the frequency of chromosome damage is higher, the frequency of cancer incidence automatically increases according to the basic mechanism of cancer caused by radiation exposure. High doses are known to cause chromosomal defects, but the influence of low-dose exposure is not clearly known. Low-dose exposure, however, can still be assumed to cause cancer as the same mechanism is involved.
Based on in vitro research on the influence of low-dose exposure due to medical X-rays, Bhatti et al., Rothkamm et al., and Neumaier et al., reported that chromosome damage frequency increases in proportion to dose. They also stated that biological restoration response is not proportional to dose [24–26]. Such results show that it is difficult to say that the recovery rate of cells in low-dose cases is good and that, therefore, a health risk does not exist. However, there is no scientific proof that low-dose radiation under 100 mSv has any specific influence on humans. Low-dose radiation is proven to cause chromosome damage in experimental settings, but has not been shown to be an actual cause of disease in the human body to date. Therefore, it is not wise to ignore the fact that there is a possible lifetime risk of cancer due to low-dose medical radiation exposure, simply because it is low-dose. However, there are various other factors that react to DNA damage to form cancer cells, so the previous statement is difficult to prove through experiment. Further, it is impossible to physically apply an exposure of 1 mGy (mSv) to a human to prove this hypothesis. Ultimately, it is not correct to say that, since no side effects have been determined, low-dose exposure is safe; more research is required and, until then, the risk of radiation exposure should be minimized when using medical diagnostic radiography systems.
There were certain limitations to our research: (1) The research sample was small and, because the study was based on cervical spine X-ray radiography, the focus was limited to thyroid cancer. (2) The short period of observation is another limitation of this study. If possible, long-term tracking observation research is necessary in the future.
In our research, however, it is meaningful that we could evaluate organ doses and the LAR of incidence, considering biological probable influence, to determine the actual influence on patient thyroids of cervical (neck) spine radiology. Furthermore, this research is contributing to a new acknowledgement of the risks of ionizing radiation by confirming the influence of radiation on cancer incidence.
Conclusion
The amounts of radiation absorbed by the thyroid and surrounding organs during cervical spine X-ray radiological procedures and the resultant LAR of cancer incidence were found to have low values. Even though the increase in the cancer incidence rate due to medical radiation is quite small, if other radiography exams are repeatedly conducted, the accumulated exposure will increase the incident rate of diseases including cancer. In the medical field, even though there is no standard base for radiation exposure doses, necessary radiology exams must be taken and, therefore, efforts to reduce radiation exposure for those undergoing frequent exams should be considered. However, medical radiography is absolutely essential for patients and, statistically, it has such a low level of risk that patients should not be overly concerned. This research is meaningful in that it provides information to examiners and patients who make use of medial radiation, allowing them to acknowledge the risk of ionizing radiation and helping them to make related decisions wisely.
References
The Korean Ministry of Food and Drug Safety (2014) News release Nationwide effectuation of recording and control work about radiation exposure dose in patients with CT exposure
Effect of Ionizing Radiation: United Nations Scientific Committee on the Effects of Atomic Radiation (2008) UNSCEAR 2006 report to the general assembly with scientific annexes. Volume 1. New York: United Nations. http://www.unscear.org/docs/reports/2006/07-82087_Report_2006_Web.pdf. Accessed 9 March 2015
National Research Council (US); Committee to Assess Health Risks from Exposure to Low Levels of Ionizing Radiation (2006) Health risks from exposure to low levels of ionizing radiation: BEIR VII phase 2. National Academies Press, Washington DC
Ron E, Lubin JH, Shore RE et al (1995) Thyroid cancer after exposure to external radiation: a pooled analysis of seven studies. Radiat Res 178(2):259–277
Seaberg RM, Eski S, Freeman JL (2009) Influence of previous radiation exposure on pathologic features and clinical outcome in patients with thyroid cancer. Arch Otolaryngol Head Neck Surg 135(4):355–359
Memon A, Godward S, Williams D, Siddique I, Al-Saleh K (2010) Dental X-rays and the risk of thyroid cancer: a case-control study. Acta Oncol 49:447–453
International Agency for Research on Cancer (2000) IARC monographs on the evaluation of carcinogenic risks to humans. Ionizing radiation: part 1. X- and gamma-radiation and neutrons. International Agency for Research on Cancer, Lyon
Republic of Korea medical law article 3. http://www.law.go.kr/engLsSc.do?menuId=0&subMenu=5&query=%EC%9D%98%EB%A3%8C%EB%B2%95%20%EC%98%81%EB%AC%B8%ED%8C%90#liBgcolor7. Accessed 9 Nov 2014
Knezevic Z, Beck N, Milkovic D, Miljanic S, Ranogajec-Komor M (2011) Characterisation of RPL and TL dosimetry systems and comparison in medical dosimetry applications. Radiat Meas 46:1582–1585
Hsu SM, Yang HW, Yeh TC et al (2007) Synthesis and physical characteristics of radiophoto luminescent glass dosimeters. Radiat Meas 42:621–624
Gali-Muhtasib H (2011) Advances in cancer therapy. In-Tech press, pp 553–567. ISBN 978-953-307-703-1
Korea Food and Drug Administration (2007) Patient dose measurement guideline, Radiation safety management series no. 14. Korean Ministry of Food and Drug Administration, pp 13–34
National Radiological Protection Board (NRPB) IPSM COR (1992) National Protocol for Patient Dose Measurements in Diagnostic Radiology NRPB. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/337175/National_Protocol_for_Patient_Dose_Measurements_in_Diagnostic_Radiology_for_website.pdf. Accessed 9 Mar 2015
Cristy, M and Eckerman, KF (1987) Specific absorbed fractions of energy at various ages from internal photon sources. I. Methods. Oak Ridge National Laboratory Report. ORNL/TM-8381/V1
International Commission on Radiological Protection (1991) 1990 Recommendations of the International Commission on Radiological Protection. ICRP Publication 60. ICRP
International Commission on Radiological Protection (2007) 2007 Recommendations of the International Commission on Radiological Protection. ICRP Publication 103. ICRP
American Cancer Society (2013) X-rays, gamma rays, and cancer risk. http://www.cancer.org/acs/groups/cid/documents/webcontent/acspc-038756-pdf.pdf. Accessed 9 March 2015
American Cancer Society (2013) Ultraviolet (UV) radiation . http://www.cancer.org/acs/groups/cid/documents/webcontent/acspc-039643-pdf.pdf. Accessed 9 March 2015
Berrington de Gonzalez A, Darby S (2004) Risk of cancer from diagnostic X-rays: estimates for the UK and 14 other countries. Lancet 363(9406):345–351
Upton AC, Adelstein SJ, Brenner DJ et al (2001) Report no. 136—evaluation of the linear-non threshold dose response model for ionizing radiation. National Council on Radiation Protection and Measurements (NCRP), Bethesda
Valentin J (2005) Low-dose extrapolation of radiation related cancer risk. Ann ICRP 35(4):1–140
United Nations Scientific Committee on the Effects of Atomic Radiation (2000) Sources and effects of ionizing radiation, UNSCEAR 2000 Report to the general assembly, with scientific annexes. United Nations, New York. http://www.unscear.org/docs/reports/gareport.pdf. Accessed 9 March 2015
Cox R, Muirhead CR, Stather JW, Edwards AA, Little MP (1995) Risk of radiation induced cancer at low doses and low dose rates for radiation protection purposes. Doc NRPB 6:1–77
Bhatti P, Yong LC, Doody MM et al (2010) Diagnostic X-ray examinations and increased chromosome translocations: evidence from three studies. Radiat Environ Biophys 49:685–692
Rothkamm K, Lobrich M (2003) Evidence for a lack of DNA double-strand break repair in human exposed to very low X-ray doses. Proc Natl Acad Sci USA 100:5057–5062
Neumaier T, Swenson J, Pham C et al (2012) Evidence for formation of DNA repair centers and dose-response nonlinearity in human cells. Proceedings National Academy of Sciences USA 109:443–448
Acknowledgments
The authors wish to thank the 94 medical institutions within the Korean central district used in this study for their cooperation.
Conflict of interest
This study was not funded by anyone. There is no financial relationship with a commercial entity producing healthcare-related products and/or services relevant to this article. Therefore, the authors declare that they have no conflict of interest.
Ethical standards
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
We measured the entrance surface dose using a Rando® phantom and calculated the patient doses using a Monte Carlo program. Thus, we believe that informed consent is not required.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Seo, D., Han, S., Kim, K.H. et al. Evaluation based on Monte Carlo simulation of lifetime attributable risk of cancer after neck X-ray radiography. Radiol med 120, 1043–1049 (2015). https://doi.org/10.1007/s11547-015-0543-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-015-0543-z