Abstract
Controversy regarding potential health risks from increased use of medical diagnostic radiologic examinations has come to public attention. We evaluated whether chromosome damage, specifically translocations, which are a potentially intermediate biomarker for cancer risk, was increased after exposure to diagnostic X-rays, with particular interest in the ionizing radiation dose–response below the level of approximately 50 mGy. Chromosome translocation frequency data from three separately conducted occupational studies of ionizing radiation were pooled together. Studies 1 and 2 included 79 and 150 medical radiologic technologists, respectively, and study 3 included 83 airline pilots and 50 university faculty members (total = 155 women and 207 men; mean age = 62 years, range 34–90). Information on personal history of radiographic examinations was collected from a detailed questionnaire. We computed a cumulative red bone marrow (RBM) dose score based on the numbers and types of X-ray examinations reported with 1 unit approximating 1 mGy. Poisson regression analyses were adjusted for age and laboratory method. Mean RBM dose scores were 49, 42, and 11 for Studies 1–3, respectively (overall mean = 33.5, range 0–303). Translocation frequencies significantly increased with increasing dose score (P < 0.001). Restricting the analysis to the lowest dose scores of under 50 did not materially change these results. We conclude that chromosome damage is associated with low levels of radiation exposure from diagnostic X-ray examinations, including dose scores of approximately 50 and lower, suggesting the possibility of long-term adverse health effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There has been a rapid increase in the use of new radiologic procedures, such as computed tomography (CT), that deliver much higher doses than conventional exam types (Ron 2003; Brenner and Hall 2007; Einstein et al. 2007; Mettler et al. 2008). In fact, the per capita dose estimate to the US population from medical radiation exposure in 2006 was six times greater than in 1982 (Mettler et al. 2008) leading to concerns about the potential for increased radiation-related cancer risks (Ron 2003; Berrington de Gonzalez and Darby 2004; Brenner and Elliston 2004; Lee et al. 2004; Hampton 2006; Martin and Semelka 2006; Brenner and Hall 2007; Einstein et al. 2007; Mettler et al. 2008; Sodickson et al. 2009). Utilization data in five US health care markets indicated that approximately 21% of adults aged 18–64 years had effective doses of 3 mSv or higher annually from medical imaging procedures and 2% of those exceeded 20 mSv per year (Fazel et al. 2009). Certain conditions, such as Crohn’s disease, require several radiologic imaging follow-up procedures with the upper 25% of patients receiving effective doses between 48 and 279 mSv over an average of 9 years (Peloquin et al. 2008). In these dose ranges cancer risks are increased, but little is known about the health effects over a lifetime of medical imaging, such as for annual screening, and not necessarily to follow disease processes.
Because of the long time between exposure and disease, problems in recalling past X-ray procedures reliably and the relatively low radiation doses, epidemiologic studies of cancer risks associated with diagnostic medical radiation are difficult to conduct. Since chromosome aberrations are well-known markers of radiation exposure (Burak et al. 2001; Kodama et al. 2001; Tawn et al. 2004; Bhatti et al. 2007), may be markers of cancer risk (Boffetta et al. 2007; Bonassi et al. 2008) and are much more common than cancer outcomes, they offer a potentially informative alternative for study. Past studies have examined chromosome aberrations in association with short-term, high-dose diagnostic X-ray exposures (Weber et al. 1995; M’Kacher et al. 2003), but only recently has chromosome damage been associated with cumulative lifetime X-ray exposures from typical diagnostic procedures (Bhatti et al. 2008; Sigurdson et al. 2008a).
Two studies conducted within the US Radiologic Technologists (USRT) cohort nearly a decade apart have reported statistically significant increases in chromosome translocations, a persistent marker of long-term radiation exposure, with an increasing number of cumulative diagnostic X-ray exposures (Bhatti et al. 2008; Sigurdson et al. 2008a). To confirm these findings and to gain greater precision in determining the dose–response relationship, particularly at doses under 50 mSv, we pooled data from these studies with previously unpublished data on personal diagnostic X-ray examinations and chromosome translocations collected as part of a recent study of cosmic radiation exposure among airline pilots (Yong et al. 2009). Airline pilots were of particular interest because they are in good health and because their X-ray examinations were from annual screenings that are required to maintain flying status.
Materials and methods
Study population
Subject recruitment and design for all three studies have been described in detail (Bhatti et al. 2007, 2008; Sigurdson et al. 2008a; Yong et al. 2009). For each study, self-reported demographic, occupational and medical history data, including history of diagnostic and therapeutic radiologic procedures were obtained from participants. Whole blood samples were also collected from participants and shipped on ice overnight to a cytogenetics laboratory.
In study 1, 300 living radiologic technologists with a wide range of occupational badge doses were approached for enrollment until 90 subjects were successfully recruited (Bhatti et al. 2008). Subjects were excluded if they reported a previous cancer diagnosis other than non-melanoma skin cancer. For the final analysis, 11 participants were excluded because of incomplete data on history of diagnostic X-ray procedures from the cohort surveys. Of the remaining 79 study subjects, 65% were female.
In study 2, subjects were selected from a group of 3,441 radiologic technologists (not involved in study 1 and separated in time by nearly a decade) with a wide range of occupational badge doses who began working before 1950, were alive and had a known address in 2003 (Sigurdson et al. 2008a). Two hundred and seven eligible technologists who reported no previous cancer diagnosis other than non-melanoma skin cancer, no family history of chromosomal instability disorders and smoking less than 10 cigarettes per day were approached for participation in the study. One hundred and fifty-nine subjects agreed to participate. The final study size was 150 individuals (69% female) because two subjects died before interview, two blood samples were unusable due to delays in shipment, and five samples did not grow in cell culture.
In study 3, 83 full-time male pilots of a major US airline were recruited from a list obtained from the union representing the pilots (Yong et al. 2009). As a comparison group, 50 male university faculty members were also recruited from the city where the airline was based. Study eligibility was based on the following criteria: age 35–56 years; a never smoker or a very light smoker; no personal history of cancer except for non-melanoma skin cancer; no history of chemotherapy or radiotherapy; and no family history of chromosomal instability disorders.
All study participants provided informed consent. The three studies were approved by the Human Subjects Review Boards of the National Cancer Institute. Studies 1 and 2 also were approved by the University of Minnesota and study 3 by the National Institute for Occupational Safety and Health.
While analyses of chromosome aberrations in association with diagnostic radiation exposure from studies 1 and 2 have been previously published (Bhatti et al. 2008; Sigurdson et al. 2008a), such analyses from study 3 have not been previously reported. In addition, for the first time, pooled analyses across the three studies are presented.
Assay for chromosome translocations
In all three studies (Bhatti et al. 2008; Sigurdson et al. 2008a; Yong et al. 2009), laboratory personnel determined the frequency of translocations in peripheral blood lymphocytes using FISH (fluorescent in situ hybridization) whole chromosome painting without knowledge of the subjects’ radiation exposure history. Cell cultures were initiated on blood collected in heparinized vacutainer tubes within 24 h of phlebotomy and were processed according to routine cytogenetic methods (Ramsey et al. 1995). The slide preparation, staining and cell scoring were performed using standardized chromosome painting protocols (Ramsey et al. 1995; Matsumoto et al. 1998). Because whole chromosome paints are applied only to a portion of the genome, the counted metaphases are converted to whole genome cell equivalents (CEs) (Tucker et al. 1997). In study 1, single-color painting of chromosomes 1, 2 and 4 was conducted with an average of 432 CEs evaluated per person (FISH method 1). In studies 2 and 3, chromosomes 1, 2, and 4 were painted red and chromosomes 3, 5, and 6 were simultaneously painted green with an average of 1,000 CEs evaluated per person (FISH method 2).
Ionizing radiation exposure
The methods used for estimating diagnostic X-ray exposure have been described previously (Bhatti et al. 2008; Sigurdson et al. 2008a; Yong et al. 2009). Based on numbers of self-reported diagnostic X-ray procedures, a cumulative red bone marrow (RBM) dose was estimated for each subject using the mid-point RBM dose values (mGy) from a previous study in which published literature and expert judgment were used to assign red bone marrow doses to a comprehensive list of examination types (Preston-Martin and Pogoda 2003). From that assessment, there was no clear evidence of temporal changes in per-procedure doses, so we did not account for time period in our exposure estimates. Total doses were summed over all procedures to obtain an estimate of the cumulative personal diagnostic RBM X-ray dose. We refer to this estimate as a dose score, rather than a dose, because of uncertainties in the recall of various procedures and in the dose estimates assigned to each procedure. However, the intent of the score assignment was to approximate mGy.
The estimation of occupational radiation exposure among the study populations has also been described in detail previously (Simon et al. 2006; Bhatti et al. 2007; Yong et al. 2009). Subjects in the USRT cohort were primarily exposed to X-rays and were monitored for these exposures with badge dosimeters; yearly badge dose data, however, were not available for all individuals, particularly those that worked in earlier time periods. Yearly dose estimates for those individuals without badge dose readings were assigned using simulation techniques from probability distributions describing the plausible range of exposures. Yearly red bone marrow doses were derived from real or simulated badge doses by applying dose conversion factors and were summed to estimate cumulative occupational red bone marrow dose for each person.
Individual dosimetry data for exposure to cosmic radiation is not collected for pilots in the United States. A surrogate variable, duration of flight experience in years (i.e., flight years) was computed from commercial airline flight history reported by the pilots in the study questionnaire (Yong et al. 2009).
Statistical analyses
In addition to mean translocation frequencies by categories of covariates, we calculated translocation rate ratios (rate and frequency are used interchangeably) for these categories relative to a reference category, such that we could adjust for the strong effect of age at blood draw (Sigurdson et al. 2008b) to determine the age-independent association of these categories with translocation levels. We used the AMFIT module of EPICURE (HiroSoft, Seattle, WA) to conduct multivariable linear Poisson regression analysis for associations between cumulative medical diagnostic X-ray RBM dose score and translocation frequency. A Pearson scale factor was included in the analysis to account for over-dispersion of the data.
When assessed individually in Poisson regression models, study group, occupation and FISH method all resulted in the substantial alterations of the estimate for the association between diagnostic X-ray exposure and chromosome translocation frequency (i.e., changed the estimate of the dose score-translocation association by more than 10%). These variables, however, were highly correlated, and because FISH method had the largest impact on the dose–response estimate, only it was included along with categories of age at blood draw (as presented in Table 2) in the final analysis. Inclusion of occupational flight years, bone marrow dose from occupational X-ray exposure, gender, prior therapeutic radiation (yes/no) and military flying (yes/no) had little influence on the association between diagnostic X-ray exposure and chromosome translocation frequency.
We determined the lowest dose score range at which a consistent and significant exposure–response could be detected by restricting the pooled analysis to sequentially lower and lower dose scores. To assess the sensitivity of the pooled point estimate by individual study, the analysis was repeated excluding one study group at a time. To evaluate study heterogeneity, we added a dose score by study group (study 1, study 2, study 3-pilots, study 3-faculty) cross-products term to the regression model. By using a likelihood ratio test comparing the model including the cross-products term to a model without this term, we assessed if there was a statistically significant (P ≤ 0.05) improvement in the fit of the model to the data, which would indicate the presence of heterogeneity of the dose score-translocation association between the study groups. We checked for evidence of non-linearity in the dose–response by adding a quadratic dose score term and comparing the fit of the model to a model without the quadratic dose score term and for stability in the estimate by removing potential outliers which were identified by visual inspection of scatter plots.
Results
Table 1 provides descriptive statistics for age, translocation frequency and cumulative medical diagnostic radiation bone marrow dose score for each of the study groups separately and for the pooled analysis. In the pooled analysis, subjects ranged in age from 34 to 90 years (mean 62) and had translocation frequencies ranging from 0 to 4.5 translocations/100 CE (mean 1.0). Cumulative medical diagnostic radiation bone marrow dose scores for participants ranged from 0 to 303.3 (mean 33.5).
Descriptive features of the pooled study population (n = 362) are provided in Table 2, including mean translocation levels by covariate categories and age-adjusted translocation rate ratios comparing categories of these covariates. The age-adjusted rate ratios indicate lower translocation levels in studies 2 and 3 compared to study 1, which may be attributed to FISH method, and increasing translocation levels with increasing cumulative RBM X-ray dose scores.
After adjusting for age at blood draw and FISH method, a 10 unit increase in medical diagnostic radiation dose score was associated with a statistically significant increase of 0.04 excess translocations/100 CE (95% CI: 0.02, 0.06; P < 0.001). Translocation frequencies plotted as a function of diagnostic RBM dose score are shown in Fig. 1 with the superimposed multivariable dose–response trend line that is specified for FISH method 2 because it was the most commonly used method in the pooled study population and for the 60–<65 age category because the mean age of the study population was 62. The dose–response was consistent with linearity, and removal of potential outliers (i.e., those 12 individuals with greater than 4.0 translocations/100 CE or dose scores greater than 200) did not affect the estimate.
Translocation frequency as a function of the cumulative diagnostic red bone marrow radiation dose score (n = 362). The trend line with 95% upper and lower confidence bounds is from multivariable Poisson regression analysis, specified for ages 60–<65 and FISH method 2. [0.04 excess translocations/100 CE/10 bone marrow dose score units (95% CI: 0.02, 0.06; P < 0.001); R 2 = 0.7]. Dose score approximates mGy
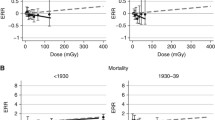
When restricting the analysis to the 287 participants with dose scores below 50, we detected a statistically significant dose–response relationship consistent with the association observed using the full dose range [0.05 excess translocations/100 CE/10 dose score units (95% CI: 0.001, 0.1; P = 0.04)] (Fig. 2a). At lower dose ranges, the dose–response relationship became increasingly large and inconsistent with the overall estimate. At dose scores of 20 and lower (n = 196), the magnitude of the association was 0.08 translocations/100 CE/10 dose score units (95% CI: −0.002, 0.02, P = 0.1; Fig. 2b). At dose scores of 10 and lower (n = 131), the estimate of the dose–response relationship was 0.3 excess translocations/100 CE/10 dose score units (95% CI: 0.06, 0.5, P = 0.02) (Fig. 2c). The low-dose range estimates remained essentially unchanged when we additionally excluded those individuals with translocation frequencies greater than 3.0 translocations/100 CE.
Translocation frequency with successive truncation of cumulative diagnostic red bone marrow radiation dose score ranges at 50 or less, 20 or less and 10 or less. Trend lines with 95% upper and lower confidence bounds are from multivariable Poisson regression analyses and are specified for ages 60–<65 and FISH method 2. a ≤50 dose score units [0.05 excess translocations/100 CE/10 bone marrow dose score units (95% CI: 0.001, 0.1; P = 0.04); R 2 = 0.7]. b ≤20 dose score units [0.08 excess translocations/100 CE/10 bone marrow dose score units (95% CI: −0.02, 0.2; P = 0.1); R 2 = 0.7]. c ≤10 dose score units [0.3 excess translocations/100 CE/10 bone marrow dose score units (95% CI: 0.05, 0.5; P = 0.02); R 2 = 0.7]. Dose score approximates mGy
The association also remained consistent after excluding one study group at a time. Our test for heterogeneity of the dose–response associations from the study populations was highly statistically significant (P < 0.001), which can be attributed to the lack of a dose–response from the university faculty [−0.03 excess translocations/100 CE/10 dose score units (95% CI: −0.07, 0.02)]. The estimates from study 1, study 2, and among the pilots in study 3, however, were consistent with each other (0.07, 0.04 and 0.07 excess translocations/100 CE/10 dose score units, respectively).
Discussion
In this pooled analysis, we found a statistically significant linear increase in translocation frequency (P = <0.001) with increasing cumulative medical diagnostic RBM radiation dose score after adjustment for age at blood drawing and FISH method. This association remained significant and consistent with the overall association even when limiting the analysis to the lowest dose scores (under 50) and excluding outliers with high translocation frequencies. In vitro experiments with lymphocytes have demonstrated significantly increased unstable chromosome aberrations at X-ray doses below 50 mGy, but not at doses below 20 mGy (Lloyd et al. 1992). While we observed a significant dose–response relationship when restricting dose scores to 10 and under, the estimate of the dose–response relationship increased by an order of magnitude and was inconsistent with the overall estimate of 0.04 excess translocations/100 CE/10 dose score units. It is estimated that a cumulative dose score of 50 would be received from just three to five CT procedures (Sigurdson et al. 2008a), and recent data indicate that certain segments of the US population are receiving cumulative doses of ionizing radiation at and above this level (Peloquin et al. 2008). The observed magnitude of 0.04 excess translocations is also consistent with the expected estimate of 0.05 excess translocations/100 CEs/10 mGy, which was previously derived by extrapolation from excess translocation frequencies observed in studies of high-energy gamma rays (Bhatti et al. 2007, 2008), suggesting that the increase in translocation frequency per unit dose score is reliably reflecting the extent of ionizing radiation exposure from diagnostic X-rays.
In our analysis for heterogeneity, we found that the association observed among university faculty members was inconsistent with the estimates from the three other study groups. While the estimated cumulative medical diagnostic RBM dose scores among faculty (mean = 11) were low compared to radiologic technologists (mean = 46) this is unlikely to be the sole reason for the heterogeneity because a similarly low mean dose score was observed among pilots (mean = 11). As seen in the previous study among airline pilots and university faculty, there are no differences in lifestyle factors that would seem to account for the heterogeneity (Yong et al. 2009). We speculate that university faculty members may not be as able to accurately recall past diagnostic X-ray procedures because they may not have undergone regular examination (pilots typically have annual physicals) or because they are not medical professionals (radiologic technologists probably are more aware of their radiographic examination history). This suggests that studies of diagnostic radiation exposure based on recall of past procedures may not be feasible in the general public.
Our ability to detect a low-dose relationship (even below a dose score of 50) was enhanced by the large number of study subjects obtained by pooling data from three separate studies and the scoring of extremely large numbers of cell equivalents (approximately 1,000) per person in studies 2 and 3. The pilots, particularly, provided a large group of individuals exposed to low levels of medical radiation that can be attributed to screening (such as chest X-rays as part of annual physicals) rather than following any active disease process, since the latter would restrict them from flying and would have made them ineligible for this study.
Recall error of past diagnostic X-ray procedures is a concern, but because study subjects had no knowledge of their translocation frequencies, the recall error would be non-differential and unlikely to result in finding a false association. While it might have been preferable to report dose in mGy, we ultimately decided on dose score as more appropriate because mGy would convey an unwarranted level of accuracy and precision for the dose estimates. In addition to the uncertainty in assigning representative dose scores for specific procedures, there is also the issue of reporting errors, since the numbers and types of diagnostic procedures were self-reported by study subjects. Thus, characterizing the nature and magnitude of errors or uncertainties associated with the radiation exposure estimates for this study is multiply complex.
FISH method was included as a covariate in our models; as seen in Table 2, differing laboratory methods may account for the large difference in translocation rate ratios when comparing study 1 to studies 2 and 3. A recent international pooling effort to assess chromosome translocations in “unexposed” human populations found evidence that inter-laboratory differences may have contributed to variability in translocation frequencies (Sigurdson et al. 2008b) and therefore should be taken into account analytically.
Because we derived genome-equivalent translocation frequencies from translocations measured in only a subset of chromosomes, the potential sensitivity of particular chromosomes to radiation-induced damage over others may have resulted in a systematic error in the translocation values used in this study. While a study of radiation-induced breakpoints in human chromosomes found evidence supporting a non-random breakpoint distribution in certain chromosomes, the authors concluded that the effect was insufficient to invalidate cytogenetic analysis using a subset of the genome for biodosimetry (Johnson et al. 1999).
With the increasing use of new diagnostic X-ray procedures, such as CT, the collective radiation dose to the public from medical procedures is rising and may be an underappreciated health risk. Individual doses from these procedures are approaching magnitudes that have been associated with increased risk of cancer in other settings (Brenner and Hall 2007). While the benefit of radiation use in disease diagnosis and patient treatment remains undisputed, the current pooled study demonstrates that low-dose diagnostic X-rays are associated with measurable cumulative chromosome damage. This includes procedures that were performed in healthy individuals for annual screening purposes rather than to follow-up active disease processes. The relationship between chromosome damage and specific disease outcomes remains uncertain, but there is supporting evidence that chromosome damage is associated with an increase in cancer risk (Boffetta et al. 2007; Bonassi et al. 2008). Potential adverse health outcomes from various relatively high-dose imaging procedures such as CT scans or in the scenario of repeated examinations to monitor chronic conditions has become appreciated recently by the medical community (Ron 2003; Berrington de Gonzalez and Darby 2004; Brenner and Elliston 2004; Lee et al. 2004; Hampton 2006; Martin and Semelka 2006; Brenner and Hall 2007; Einstein et al. 2007; Mettler et al. 2008; Peloquin et al. 2008; Fazel et al. 2009; Sodickson et al. 2009) but effects from very low doses related to screening examinations may also be an emerging concern.
References
Berrington de Gonzalez A, Darby S (2004) Risk of cancer from diagnostic X-rays: estimates for the UK and 14 other countries. Lancet 363(9406):345–351
Bhatti P, Preston DL, Doody MM, Hauptmann M, Kampa D, Alexander BH, Petibone D, Simon SL, Weinstock RM, Bouville A, Yong LC, Freedman DM, Mabuchi K, Linet MS, Edwards AA, Tucker JD, Sigurdson AJ (2007) Retrospective biodosimetry among United States radiologic technologists. Radiat Res 167(6):727–734
Bhatti P, Doody MM, Preston DL, Kampa D, Ron E, Weinstock RW, Simon S, Edwards AA, Sigurdson AJ (2008) Increased frequency of chromosome translocations associated with diagnostic x-ray examinations. Radiat Res 170(2):149–155
Boffetta P, van der Hel O, Norppa H, Fabianova E, Fucic A, Gundy S, Lazutka J, Cebulska-Wasilewska A, Puskailerova D, Znaor A, Kelecsenyi Z, Kurtinaitis J, Rachtan J, Forni A, Vermeulen R, Bonassi S (2007) Chromosomal aberrations and cancer risk: results of a cohort study from Central Europe. Am J Epidemiol 165(1):36–43
Bonassi S, Norppa H, Ceppi M, Stromberg U, Vermeulen R, Znaor A, Cebulska-Wasilewska A, Fabianova E, Fucic A, Gundy S, Hansteen IL, Knudsen LE, Lazutka J, Rossner P, Sram RJ, Boffetta P (2008) Chromosomal aberration frequency in lymphocytes predicts the risk of cancer: results from a pooled cohort study of 22 358 subjects in 11 countries. Carcinogenesis 29(6):1178–1183
Brenner DJ, Elliston CD (2004) Estimated radiation risks potentially associated with full-body CT screening. Radiology 232(3):735–738
Brenner DJ, Hall EJ (2007) Computed tomography—an increasing source of radiation exposure. N Engl J Med 357(22):2277–2284
Burak LE, Kodama Y, Nakano M, Ohtaki K, Itoh M, Okladnikova ND, Vasilenko EK, Cologne JB, Nakamura N (2001) FISH examination of lymphocytes from Mayak workers for assessment of translocation induction rate under chronic radiation exposures. Int J Radiat Biol 77(8):901–908
Einstein AJ, Henzlova MJ, Rajagopalan S (2007) Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography. JAMA 298(3):317–323
Fazel R, Krumholz HM, Wang Y, Ross JS, Chen J, Ting HH, Shah ND, Nasir K, Einstein AJ, Nallamothu BK (2009) Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med 361(9):849–857
Hampton T (2006) Researchers examine long-term risks of exposure to medical radiation. JAMA 296(6):638–640
Johnson KL, Brenner DJ, Nath J, Tucker JD, Geard CR (1999) Radiation-induced breakpoint misrejoining in human chromosomes: random or non-random? Int J Radiat Biol 75(2):131–141
Kodama Y, Pawel D, Nakamura N, Preston D, Honda T, Itoh M, Nakano M, Ohtaki K, Funamoto S, Awa AA (2001) Stable chromosome aberrations in atomic bomb survivors: results from 25 years of investigation. Radiat Res 156(4):337–346
Lee CI, Haims AH, Monico EP, Brink JA, Forman HP (2004) Diagnostic CT scans: assessment of patient, physician, and radiologist awareness of radiation dose and possible risks. Radiology 231(2):393–398
Lloyd DC, Edwards AA, Leonard A, Deknudt GL, Verschaeve L, Natarajan AT, Darroudi F, Obe G, Palitti F, Tanzarella C et al (1992) Chromosomal aberrations in human lymphocytes induced in vitro by very low doses of X-rays. Int J Radiat Biol 61(3):335–343
M’Kacher R, Violot D, Aubert B, Girinsky T, Dossou J, Beron-Gaillard N, Carde P, Parmentier C (2003) Premature chromosome condensation associated with fluorescence in situ hybridisation detects cytogenetic abnormalities after a CT scan: evaluation of the low-dose effect. Radiat Prot Dosimetry 103(1):35–40
Martin DR, Semelka RC (2006) Health effects of ionising radiation from diagnostic CT. Lancet 367(9524):1712–1714
Matsumoto K, Ramsey MJ, Nelson DO, Tucker JD (1998) Persistence of radiation-induced translocations in human peripheral blood determined by chromosome painting. Radiat Res 149(6):602–613
Mettler FA Jr, Thomadsen BR, Bhargavan M, Gilley DB, Gray JE, Lipoti JA, McCrohan J, Yoshizumi TT, Mahesh M (2008) Medical radiation exposure in the U.S. in 2006: preliminary results. Health Phys 95(5):502–507
Peloquin JM, Pardi DS, Sandborn WJ, Fletcher JG, McCollough CH, Schueler BA, Kofler JA, Enders FT, Achenbach SJ, Loftus EV Jr (2008) Diagnostic ionizing radiation exposure in a population-based cohort of patients with inflammatory bowel disease. Am J Gastroenterol 103(8):2015–2022
Preston-Martin S, Pogoda JM (2003) Estimation of radiographic doses in a case-control study of acute myelogenous leukemia. Health Phys 84(2):245–259
Ramsey MJ, Moore DH II, Briner JF, Lee DA, Olsen L, Senft JR, Tucker JD (1995) The effects of age and lifestyle factors on the accumulation of cytogenetic damage as measured by chromosome painting. Mutat Res 338(1–6):95–106
Ron E (2003) Cancer risks from medical radiation. Health Phys 85(1):47–59
Sigurdson AJ, Bhatti P, Preston DL, Doody MM, Kampa D, Alexander BH, Petibone D, Yong LC, Edwards AA, Ron E, Tucker JD (2008a) Routine diagnostic X-ray examinations and increased frequency of chromosome translocations among U.S. radiologic technologists. Cancer Res 68(21):8825–8831
Sigurdson AJ, Ha M, Hauptmann M, Bhatti P, Sram RJ, Beskid O, Tawn EJ, Whitehouse CA, Lindholm C, Nakano M, Kodama Y, Nakamura N, Vorobtsova I, Oestreicher U, Stephan G, Yong LC, Bauchinger M, Schmid E, Chung HW, Darroudi F, Roy L, Voisin P, Barquinero JF, Livingston G, Blakey D, Hayata I, Zhang W, Wang C, Bennett LM, Littlefield LG, Edwards AA, Kleinerman RA, Tucker JD (2008b) International study of factors affecting human chromosome translocations. Mutat Res 652(2):112–121
Simon SL, Weinstock RM, Doody MM, Neton J, Wenzl T, Stewart P, Mohan AK, Yoder RC, Hauptmann M, Freedman DM, Cardarelli J, Feng HA, Bouville A, Linet M (2006) Estimating historical radiation doses to a cohort of U.S. radiologic technologists. Radiat Res 166(1 Pt 2):174–192
Sodickson A, Baeyens PF, Andriole KP, Prevedello LM, Nawfel RD, Hanson R, Khorasani R (2009) Recurrent CT, cumulative radiation exposure, and associated radiation-induced cancer risks from CT of adults. Radiology 251(1):175–184
Tawn EJ, Whitehouse CA, Tarone RE (2004) FISH chromosome aberration analysis on retired radiation workers from the Sellafield nuclear facility. Radiat Res 162(3):249–256
Tucker JD, Breneman JW, Briner JF, Eveleth GG, Langlois RG, Moore DH II (1997) Persistence of radiation-induced translocations in rat peripheral blood determined by chromosome painting. Environ Mol Mutagen 30(3):264–272
Weber J, Scheid W, Traut H (1995) Biological dosimetry after extensive diagnostic x-ray exposure. Health Phys 68(2):266–269
Yong LC, Sigurdson AJ, Ward EM, Waters MA, Whelan EA, Petersen MR, Bhatti P, Ramsey MJ, Ron E, Tucker JD (2009) Increased frequency of chromosome translocations in airline pilots with long-term flying experience. Occup Environ Med 66:56–62
Acknowledgments
This research was supported by the Intramural Research Program of the Division of Cancer Epidemiology and Genetics, National Cancer Institute and in part by an interagency agreement between the National Institute for Occupational Safety and Health and the National Cancer Institute (contract Y1CP802904). Work was performed in part under the auspices of the US DOE by the Lawrence Livermore National Laboratory under contract no. W-7405-ENG-48. We thank the two anonymous reviewers for their helpful comments on the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bhatti, P., Yong, L.C., Doody, M.M. et al. Diagnostic X-ray examinations and increased chromosome translocations: evidence from three studies. Radiat Environ Biophys 49, 685–692 (2010). https://doi.org/10.1007/s00411-010-0307-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00411-010-0307-z