Abstract
Purpose
This study was done to evaluate the appropriateness of dose indices in computed tomography (CT) by comparing the body computed tomography dose index (CTDI) and the size-specific dose estimates (SSDE) to determine which of these two parameters is more appropriate to estimate the radiation dose to both adult and paediatric patients.
Materials and methods
We analysed 150 thoracic CT and 150 abdominal CT scans, half of which from adult patients and the other half from paediatric patients. We compared the values of the CTDIvol and the SSDE reporting the average, maximum and minimum percentage difference for each body region and depending on the age of the patients.
Results
In the thoracic CT and abdominal CT scans, we found values of difference between the SSDE and the CTDIvol of 26.3 and 27.3 %, respectively, in adult patients and of 46.9 and 48.5 % in paediatric patients.
Conclusions
The SSDE is a good tool for estimating the average radiation dose for a given patient depending on the input parameters and the dimensions of the specific person in question before a CT examination.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The recent progressive increase in the number of radiological examinations, especially of computed tomography (CT) examinations, has led to a substantial increase in the dose to the population from medical exposures [1, 2]. This phenomenon must be governed by a more stringent application of the principles of radiation protection, such as “justification” and “optimisation” of the examination, in order to ensure the appropriateness and minimisation of the dose in the population [3, 4].
Although it has been a long time since the use of RIS–PACS for archiving of examinations entered clinical practice, similar systems which combine the radiation dose to the examination and allow, through statistical processing, organisation of the procedures and doses according to reference levels established for each examination, have not yet been implemented on a large scale [5]. So far, there have been only a few sporadic reports of single-centre trials investigating computer systems for the storage of the dose [6, 7].
The current CT systems display on the screen of the device both the computed tomography dose index (CTDI) and the dose-length product (DLP), before and after the execution of the examination [8].
The CTDI is an index of local dose, which is independent of the length of the scanned volume. The CTDI was developed to provide a standardised method for comparing the output level of radiation between different CT scanners using a phantom reference (head or body, measuring 16 and 32 cm in diameter, respectively). To better represent the radiation dose in CT examinations also performed in helical mode, the CTDIvol (CTDI volumetric) was introduced, which also takes into account the pitch [9].
The CTDIvol remains, however, a dose index independent of the length of the scan. To better represent the total radiation dose delivered it is necessary to introduce a CT dose index that takes into account the full extent of the acquired volume. Therefore, the DLP was introduced as the dosimetric value that characterises a complete acquisition scan. The DLP is obtained by multiplying the CTDIvol by the length of the scan [10].
Both of these dosimetric quantities are sensitive to the variation of scanning parameters, such as tube voltage (kVp), current (mAs), gantry rotation time, pitch and bow-tie filtration, but they are both independent of the size of the patient [9, 10]. In fact, for a given CT scan of a patient, the CTDIvol and its DLP are displayed for a reference phantom (head or body), the diameter of which (16 or 32 cm) is selected by the scanner. In general, the first is selected for CT scans of the head, while the second for the examinations of the torso (chest and abdomen) [11].
For paediatric patients the head phantom should always be selected, even if, for paediatric body CT protocols, some systems use the 16-cm phantom as a benchmark and others use the 32-cm phantom. This is a problem as it may cause an underestimation of dose levels in the younger paediatric patients if the 32-cm phantom is used as a Ref. [12].
The CTDIvol and the DLP are, therefore, limited since the measurements are carried out using only two standard cylindrical and homogeneous phantoms, which do not represent the correct dose for objects of substantially different shape, size and attenuation, such as the human body.
The radiation dose received by a patient during a CT examination depends on both the radiation output of the scanner and the size of the patient, and the CTDIvol provides information regarding only the output of the device, without taking into account the size of the patient being examined. For these two reasons, it does not allow a specific estimate of the radiation dose for a given individual, particularly in paediatrics [13, 14].
Radiologists, medical physicists and radiographers need computational tools which are easy to use and estimate the radiation dose as accurately as possible [15]. To provide these tools, not only for paediatric CT examinations but also for CT examinations of adult patients of any size, a working group (AAPM Task Group Report 204, 2011) was appointed to develop conversion factors that could be applied to the dose index the CTDIvol displayed on the CT scanner [8]. This way, a new parameter is obtained that allows an estimate of patient dose according to the individual’s specific dimensions, which is called a size-specific dose estimate (SSDE).
The SSDE was defined in the “Report of AAPM Task Group 204” as the estimation of dose to the patient that takes into account the corrections based on linear dimensions measured in the same patient or in CT images. The values of the SSDE are specifically based on the CTDIvol reported in the CT scanner (measured conventionally using a 16 or 32-cm PMMA phantom), which is normalised by factors dependent on patient size. This normalisation process does not take into account most of the differences between each scanner and the settings of the scanner tube voltages, but it is very important because it allows us to estimate the radiation dose to the patient depending on the type examined, finding its greatest benefits for CT scans of children or small adults [13, 14].
The correction factors to be applied to the CTDIvol in order to derive the SSDE have emerged by combining the results from four research groups that worked independently of each other [8]. The good concordance recorded suggests a level of reliability of factors that would have been higher if only one working group had produced these same data. The measurement methods and tools used were different for each group and this further extends the experimental validity which allowed the size-dependent conversion factors to be obtained and tabulated. Common to all the working groups, to obtain the correction factors, was the calculation of some quantities associated with the related size phantoms used and subsequently transported to the resulting tables, which are necessary to determine the appropriate correction factor for each individual patient. Indeed, to know which factor should be applied to the CTDIvol of a single patient, it is necessary to know at least one of these size-related parameters: lateral (LAT), anterior-posterior (AP), sum of AP + LAT and effective diameter. These measurements can be derived from the centring images (scout views) of the CT scan or from some axial CT scans acquired in certain areas of the body.
The effective diameter is the diameter of the patient in a specific position along the z axis, assuming that he has a circular cross section. While some body parts are close to a circular cross section, many are not. The effective diameter can, therefore, be thought of as the diameter of a circle whose area corresponds to that of a cross section of the patient on an image. In the paper of Brady et al. [16] the effective diameter is the parameter with less variation for the calculation of the SSDE.
Our study aimed to evaluate the appropriateness of the dose indices and focuses mainly on the comparison between the CTDI and the SSDE in body CT of both adult and paediatric patients, who present a more critical situation. The analysis is intended to define which of these two parameters is more suitable to estimate the radiation dose to the patient, which can then also be indicated in the scan report and recorded in the appropriate database.
Materials and methods
We analysed 150 thoracic and 150 abdominal CT scans, half of which from adult patients and the other half from paediatric patients, carried out between January and June 2013.
The examinations were carried out using the following CT systems: LightSpeed 16 GE (Milwaukee, USA); LightSpeed Ultra GE (Milwaukee, USA); LightSpeed VCT GE (Milwaukee, USA).
For adult patients the acquisition protocol for abdominal and thoracic CT was: helical scan, automatic mAs, 120 kV, 3–5-mm slice thickness, pitch ≥1 <1.5, gantry rotation time 0.6 s, large acquisition field of view (FOV). For paediatric patients the acquisition protocol for abdominal and thoracic CT was: helical scan, automatic mAs, 80–100 kV, 2–5 mm slice thickness, pitch ≥1 <1.3, gantry rotation time 0.5 s, small acquisition FOV.
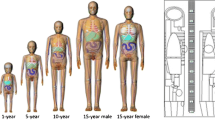
The paediatric patients were divided according to age group (0–3, 4–10, 11–18 years).
We used the software “DoseWatch” (GE, Milwaukee, USA) to extract and collect the dosimetric data. DoseWatch is a client–server software designed to ensure automatic retrieval and analysis of dosimetric data directly from medical imaging systems. Along with the collection and storage of dosimetric data, the programme also offers statistical analysis, integrated connections with RIS and PACS, automatic alarms and tools to optimise the dose and the image quality.
The following dosimetric data were recorded: the CTDIvol, the type of phantom used for the calculation of CTDI and the dimensional parameters necessary for the SSDE calculation, in particular: the lateral dimension (LAT), the anterior-posterior dimension (AP), the AP + LAT dimension and the effective diameter. We calculated the patient’s effective diameter according to the formula: √AP + LAT.
The SSDE of each patient was then calculated through the CTDIvol, the effective diameter and tables that show the conversion factors, as reported by AAPM Report n. 204 [8].
We compared the values of the CTDIvol and the SSDE reporting the average, maximum and minimum percentage differences for each body system and according to the patients’ age. We evaluated the evolution of the sizes of paediatric patients in relation to the phantoms taken into account for the calculation of CTDI.
Results
Analysing the data of the adult patients we obtained the results shown in Tables 1 and 2. In thoracic CT and abdominal CT of adult patients, we found differences between the SSDE and the CTDIvol of 26.3 and 27.3 %, respectively. Analysing the data separately in thoracic CT and abdominal CT, very high difference rates, up to 91 % (Figs. 1, 2), were also detected.
The data relating to paediatric patients are shown in Tables 3 and 4. The average percentages of difference between the two parameters are greater than in adults and close to 50 % (46.9 % in thoracic CT and 48.5 % in abdominal CT). By examining in detail the individual examinations of the chest and abdomen, offset values of 106.1 and 129.8 % were also found (Figs. 3, 4).
Patients between 0 and 3 years old showed a low percentage of difference between the CTDIvol and the SSDE (11.2 %), with a maximum of 26.8 % and a minimum of 1 %. In all the cases examined, to calculate the CTDIvol we used the head phantom, whose dimensions do not differ particularly from the average effective diameter detected (13.38 cm) in this age group. Different results were found for patients aged between 4 and 10 years old, who presented a difference in the average percentage of 62.4 %, and for those falling between 11 and 18 years old, with a gap of 52.7 %.
There were maximum percentage differences of 106.1 % (4–10 years) and 84 % (11–18 years). In these cases the CT scanner used the body phantom (32 cm in diameter) for the calculation of the CTDIvol, which is much larger (even double) compared to that of the paediatric patients examined. As shown in Fig. 1, the peak of effective diameter is around 20–25 cm, a value that corresponds neither to the size of the 16-cm head phantom nor to that of the 32-cm body phantom.
As concerns the abdominal CT of paediatric patients, stratified by age, we obtained the results shown in Table 4.
The results of abdominal CT are very similar to those of thoracic CT.
The CTDIvol does not reflect the average effective diameter neither of patients in the 4–10 years age group (17.77 cm) nor of patients aged 11–18 years (23.08 cm).
Analysing in detail the evolution of the effective diameter of the paediatric patients who underwent abdominal CT (Fig. 2), it can be seen that there are many differences among patients, with effective diameters ranging from 9.87 to 32 cm.
Discussion
Our data show that the CTDIvol has limitations in the estimation of dose because it is calculated with reference to only two phantoms, 16 and 32 cm in diameter, regardless of the type of patient examined. These phantoms do not reflect the general population and are also often chosen inappropriately by the CT scanner, especially in the paediatric examinations, where even if a patient has an effective diameter of about 16 cm, the CT scanner will use the 32-cm phantom for the calculation of the CTDIvol.
Analysing the data separately in thoracic CT and abdominal CT, very high differences (up to 91 %) were also detected, indicating an underestimation by the CTDIvol of the radiation dose, or even negative (up to −15 %) which, on the contrary, indicates an overestimation of the dose.
Very high or negative percentage values are a consequence of the size of the patient, respectively, smaller or larger than the reference phantom used to obtain the CTDIvol. In all these cases, the CTDIvol is, therefore, inappropriate in the estimation of radiation dose, as not corresponding to the delivered dose for that patient, but referred to a standard reference phantom, the dimensions of which deviate from the actual dimensions of the patient. The SSDE, on the other hand, takes into account the size of the individual subjected to the specifications and therefore more accurately expresses the dose delivered.
Analysing the overall average values of the SSDE and the CTDIvol in paediatric patients, without distinguishing by age, one can immediately see how the percentages of difference between the two parameters are greater than in adults, close to 50 % (46.9 % in thoracic CT and 48.5 % in abdominal CT). By examining in detail the individual examinations of the chest and abdomen, offset values of 106.1 and 129.8 % were also found. Patients between 0 and 3 years old show a low percentage of difference between the CTDIvol and the SSDE (11.2 %), with a maximum of 26.8 % and a minimum of 1 %. In all the cases examined, the head phantom was used to calculate the CTDIvol, the dimensions of which do not differ particularly from the average effective diameter detected (13.38 cm) in this age group.
The results differ, however, for patients ranging from 4 to 10 years old, presenting a difference in the average percentage of 62.4 %, and for those who are between 11 and 18 years old, with a standard deviation of 52.7 %. These values reveal an inappropriateness of the CTDIvol to estimate the radiation dose to the patient, since it underestimates the average dose by more than 50 %.
Maximum percentage differences of 106.1 % (4–10 years) and 84 % (11–18 years) are also reached. In these cases, for the calculation of the CTDIvol the CT scanner uses the body phantom (32 cm in diameter), which is much larger (even double the size) compared to the paediatric patients examined. As shown in Fig. 5, the peak of effective diameter is at 20–25 cm, a value that does not correspond either to the size of the head phantom of 16 cm or to that of the body phantom of 32 cm.
This actually indicates that both phantoms do not represent the paediatric population, which varies widely in size (from 10.08 to 32.97 cm) between ages, but also within the same age group. The CTDIvol is, therefore, unsuitable to represent an estimate of patient dose in paediatric CT studies of the chest, being calculated in reference to only two standard phantoms, as opposed to the SSDE, which instead assesses the dimensions of each individual patient.
The values obtained for abdominal CT in paediatric patients show a very similar situation to that of thoracic CT.
Even here, the percentage of difference (14.8 %) for paediatric patients between 0 and 3 years old is not so high, due to the fact that in most cases, for the calculation of the CTDIvol, the head reference phantom is used, which does not differ much from the average effective diameter which characterises this age group (13.58 cm). In the few cases in which, instead, the body phantom is used, very high percentage deviations are detected, up to 129.8 %, which reveals an incorrect choice by the CT scanner of the reference phantom to be used for the calculation of the CTDIvol.
As was the case in the thoracic CT, also in abdominal CT there are significantly higher percentage differences between the SSDE and the CTDIvol, both in the 4–10 years age group (64.1 %) and in the 11–18 years age group (53.1 %). By analysing individually each examination, maximum values of 122.2 and 84 % were detected, respectively.
As seen in Fig. 6, the peak is at 15–20 cm in diameter, a value that is close to the size of the head phantom (16 cm), but which differs greatly from the body phantom (32 cm). The wide range of values, however, indicates a wide dimensional variety among patients of different ages, but also between patients of the same age, which does not allow the CTDIvol an accurate dose estimation, given that it refers only to two standard measures. For this reason, even in the abdominal CT of paediatric patients the measurement of the SSDE is more precise.
In most cases the CTDIvol underestimates the radiation dose in small-sized adult patients and in paediatric patients with a peak percentage difference of up to approximately 130 % compared to the SSDE. In contrast, in large patients, the CTDIvol tends to overestimate the radiation dose. Therefore, it is not a dosimetric index specific for each patient, but above all it is a surrogate of the output of the CT scanner, as already reported by some papers [13, 14].
The SSDE is a good tool to estimate the average radiation dose for a given patient before a CT study, based on the input parameters and the size of the specific person to be examined, but it is not correct for the differences in the distribution of the dose to organs [16].
Given that the majority of modern CT scanners can display the CTDIvol before a scan, the correction factors proposed can be used by the technician or by the radiologist to estimate in advance the specific radiation dose for that patient, so as to have a feedback on the appropriateness of the parameters associated with size. This way, the accuracy of dosimetry is improved compared to using only the scanner output (CTDIvol) as a surrogate of the radiation dose to the patient.
Conclusions
The results obtained indicate that it is important that the dose recording systems appearing on the market are able to calculate and record the SSDE for each patient. Such systems are good tools for the optimisation of the examination not only from a dosimetric point of view, but also as an analysis of incorrect patient positioning with respect to the scanner coordinates, allowing for a more accurate evaluation of the examination in general. The strategy for the dose evaluation and optimisation, especially in paediatric patients, should start from the size of the patient.
References
Smith-Bindaman R (2010) Is computed-tomography safe? New Engl J Med 363:1–4
Brenner DJ, Hricak H (2010) Radiation exposure from medical imaging: time to regulate? JAMA 304:208–209
Goske MJ, Applegate KE, Bulas D et al (2012) Image gently 5 years later: what goals remain to be accomplished in radiation protection for children? AJR Am J Roentgenol 199:477–479
Kalra MK, Maher MM, Tothet TL et al (2004) Strategies for CT radiation dose optimization. Radiology 230:619–628
Golding SJ (2010) Radiation exposure in CT: what is the professionally responsible approach? Radiology 255:683–686
Robinson TJ, Robinson JD, Kanal K (2013) Implementation of the ACR dose index registry at a large academic institution: early experience. J Digit Imaging 26:309–315
Cook TS, Zimmerman SL, Steingall S et al (2011) RADIANCE: an automated, enterprise-wide solution for archiving and reporting CT radiation dose estimates. Radiographic 31:1833–1846
Boone J, Strauss KJ, Cody DD et al (2011) Size specific dose estimates (SSDE) in pediatric and adult body CT examinations. Report of AAPM Task Group 204. College Park: American Association of Physicists in Medicine
Wilting JE, Zwartkruis A, van Van Leeuwen MS (2001) A rational approach to dose reduction in CT: individualized scan protocols. Eur Radiol 11:2627–2632
Bauhs NT (2008) Dosimetry: comparison of measurement techniques and devices. Radiographics 28:245–253
Colagrande S, Origgi D, Zatelli G et al (2014) CT exposure in adult and paediatric patients: a review of the mechanisms of damage, relative dose and consequent possible risks. Radiol Med 119:803–810
Li B, Behrman RH, Norbash AM (2012) Comparison of topogram-based body size indices for CT dose consideration and scan protocol optimization. Med Phys 39:3456–3465
Larson DB, Wang LL, Podberesky DJ, Goske MJ (2013) System for verifiable CT radiation dose optimization based on image quality. Part I. Optimization model. Radiology 269:167–176
Larson DB, Malarik RJ, Hall SM, Podberesky D (2013) System for verifiable CT radiation dose optimization based on image quality. Part II. Process control system. Radiology 269:177–185
Christianson O, Li X, Frush D, Samei E (2012) Automated size-specific CT dose monitoring program. Assessing variability in CT dose. Med Phys 39:7131–7139
Brady SL, Kaufman RA (2012) Investigation of the American Association of Physicists in Medicine Report 204 size-specific dose estimates for pediatric CT implementation. Radiology 265:832–840
Conflict of interest
The authors declare that they have no conflict of interest related to the publication of this article
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Valeri, G., Cegna, S., Mari, A. et al. Evaluating the appropriateness of dosimetric indices in body CT. Radiol med 120, 466–473 (2015). https://doi.org/10.1007/s11547-014-0476-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-014-0476-y